Summary
Abstract
Dutasteride (Avodart®), an oral synthetic 4-azasteroid, is a potent, selective, irreversible inhibitor of type 1 and type 2 5α-reductase (5AR), the enzyme that converts testosterone to dihydrotestosterone (DHT) intracellularly. Although type 2 5AR predominates, both isoenzymes are overexpressed in prostate tissue in benign prostatic hyperplasia (BPH) and at all stages in some prostate cancers. Oral dutasteride 0.5 mg once daily is approved for the treatment of moderate to severe symptomatic BPH in men with an enlarged prostate to improve symptoms, and to reduce the risk of acute urinary retention (AUR) and the need for BPH-related surgery.
In pivotal 2-year phase III trials, oral dutasteride 0.5 mg once daily improved urinary symptoms, decreased total prostate volume (TPV), and reduced the risk of AUR and BPH-related surgery in men with moderate to severe symptoms of BPH and prostate enlargement. The good efficacy and tolerability of dutasteride was maintained for up to 4 years in open-label extension studies. Results of the preplanned, 2-year interim analysis of the CombAT trial showed that the combination of dutasteride and tamsulosin was superior to either drug as monotherapy in improving BPH-related symptoms, peak urinary flow and BPH-related health status. The overall adverse event profile for combination therapy was consistent with those reported for both monotherapies. Although drug-related adverse events were more frequent with combination therapy versus both monotherapies, most did not result in treatment cessation.
Dutasteride is being investigated for its efficacy in reducing the risk of prostate cancer in at-risk men in the 4-year REDUCE study and as treatment to extend the time to progression in men with low-risk localized prostate cancer who would otherwise undergo watchful waiting in the 3-year REDEEM study. Thus, dutasteride is an effective treatment option in patients with moderate to severe symptomatic BPH and demonstrable prostatic enlargement, and may have potential to reduce the risk of developing biopsy-detectable prostate cancer in at-risk individuals or extending the time to progression in low-risk localized prostate cancer.
Pharmacological Properties
Dutasteride is a more potent inhibitor of type 1 (45-fold) and type 2 5AR (2.5-fold) than finasteride (a type 2 5AR inhibitor) in vitro. In patients with symptomatic BPH, oral dutasteride 0.5 mg once daily for 2 years was associated with a median 93.7% decrease in serum DHT levels from baseline compared with placebo (p < 0.001 vs baseline and placebo) in the phase III dutasteride trials, and this was maintained during the 2-year open-label extension studies. In phase II trials, mean intraprostatic DHT levels were reduced from baseline by 94% with dutasteride compared with placebo in men with BPH, and by 90–97% in men with prostate cancer receiving dutasteride 0.5–5 mg once daily. After 24 weeks’ treatment, dutasteride 0.5 mg once daily reduced serum DHT levels from baseline to a greater extent and with less variability than finasteride 5 mg once daily in a dose-ranging study (adjusted mean reductions of 95% vs 71%; p < 0.001).
Mean levels of serum prostate-specific antigen (PSA), a powerful predictor of prostate size, were halved after 2 years of dutasteride therapy in the phase III dutasteride trials (p < 0.001 vs baseline and placebo), whereas those in placebo recipients were increased. Reductions in mean serum PSA levels seen at 2 years were maintained for up to 4 years in the open-label extension studies. Dutasteride had no clinically significant effects on serum testosterone or luteinizing hormone levels, bone density, markers of bone metabolism or serum lipid levels, and had modest, reversible effects on semen parameters.
Mean peak serum concentrations of dutasteride were achieved 1–3 hours after oral administration of a single 0.5 mg dose, with steady-state concentrations achieved after 24 weeks’ administration of a once-daily 0.5 mg dose. The absolute bioavailability of dutasteride is ≈60% and the drug is highly bound to plasma proteins. It is extensively distributed throughout central and peripheral compartments, including semen, with a large volume of distribution (300–500 L). Steady-state concentrations of the drug are seen in semen after 6 months. Dutasteride is extensively metabolized in the liver via the cytochrome P450 (CYP) isoenzymes CYP3A4 and CYP3A5, and is mainly excreted via the faeces. The terminal elimination half-life at steady state is 5 weeks. Dutasteride has no pharmacokinetic interactions with α1-adrenergic antagonists, warfarin, digoxin or cholestyramine. Because of the potential for increased systemic exposure, caution is required when dutasteride is coadministered with potent, chronic CYP3A4 inhibitors, such as ritonavir.
Therapeutic Efficacy
Dutasteride was superior to placebo in the treatment of symptomatic BPH in the phase III dutasteride trials. The co-primary endpoints in these trials, which were evaluated using pre-planned pooled analyses in ≥4000 patients, were changes in the American Urological Association Symptom Index (AUA-SI) from baseline at 1 year and in the risk of AUR at 2 years. Dutasteride 0.5 mg once daily for 2 years was associated with a clinically significant improvement in the mean AUA-SI score from baseline (mean reduction of 4.5 points; p < 0.001 vs baseline and placebo). Clinically relevant improvements from baseline were seen after 6 months’ therapy with dutasteride and between-group differences evident at 1 year were maintained throughout the treatment period. The relative risks of AUR and BPH-related surgical interventions in dutasteride recipients were reduced by 57% and 48%, respectively, versus placebo at 2 years (both p < 0.001). Dutasteride reduced TPV (by a mean of ≈26%), improved urinary flow (Qmax) from baseline and was associated with clinically relevant improvements in health-related quality of life. The beneficial effects of dutasteride on AUA-SI scores, urinary flow, AUR, BPH-related surgery and TPV were maintained for up to 4 years in extension studies.
The efficacy of dutasteride and tamsulosin, alone and in combination, is under investigation in the 4-year CombAT trial, which has enrolled 4844 men with moderate to severe symptoms of BPH and prostate enlargement. Combination therapy with dutasteride and tamsulosin was superior (p < 0.001) to each drug as monotherapy with regard to symptom improvements in the 2-year interim analysis. Improvements in symptoms from baseline were significantly greater with combination therapy from month 3 versus dutasteride, and from month 9 versus tamsulosin (both p < 0.001). Improvements in Qmax from baseline were significantly (p ≤ 0.006) greater with combination therapy versus each monotherapy at each post-baseline visit from month 6 through to year 2.
Tolerability
Dutasteride was generally well tolerated, with similar proportions of dutasteride or placebo recipients reporting an adverse event in the phase III dutasteride trials. Although the incidence of treatment-related sexual adverse events (impotence, decreased libido, ejaculation disorder and gynaecomastia) was increased with dutasteride versus placebo, this was generally transient and the incidence of each event was low (1.8–6.0% vs 0.5–3.0% in year 1, reducing to 0.5–1.7% vs 0.1–1.2% in year 2). Only gynaecomastia occurred significantly more frequently with dutasteride than with placebo after the first 6 months of treatment. The tolerability profile of dutasteride after 4 years of treatment in the extension studies was consistent with that at 2 years. In the CombAT trial, the profile of adverse events at the 2-year interim analysis with the combination of dutasteride and tamsulosin was consistent with those of the respective monotherapies. Although the incidence of drug-related adverse events was significantly higher in the combination therapy group compared with each monotherapy group (both p < 0.001) in the CombAT trial, withdrawal rates were low, with no substantial differences between treatment groups.
Similar content being viewed by others
References
Andriole G, Bruchovsky N, Chung LW, et al. Dihydrotestoster-one and the prostate: the scientific rationale for 5α-reductase inhibitors in the treatment of benign prostatic hyperplasia. J Urol 2004 Oct; 172(4 Pt 1): 1399–403
Schalken JA. The androgen cascade in ageing men: blessing or curse? Eur Urol Suppl 2003; 2(8): 8–12
Schalken JA. Molecular and cellular prostate biology: origin of prostate-specific antigen expression and implications for benign prostatic hyperplasia. BJU Int 2004 Mar; 93 Suppl. 1: 5–9
Carson 3rd C, Rittmaster R. The role of dihydrotestosterone in benign prostatic hyperplasia. Urology 2003 Apr; 61 (4 Suppl. 1): 2–7
Andriole GL, Kirby R. Safety and tolerability of the dual 5α-reductase inhibitor dutasteride in the treatment of benign prostatic hyperplasia. Eur Urol 2003; 44(1): 82–8
Iehle C, Radvanyi F, Gil Diez de Medina S, et al. Differences in steroid 5α-reductase iso-enzymes expression between normal and pathological human prostate tissue. J Steroid Biochem Mol Biol 1999 Mar; 68(5–6): 189–95
Berthaut I, Mestayer C, Portais MC, et al. Pharmacological and molecular evidence for the expression of the two steroid 5α-reductase isozymes in normal and hyperplastic human prostatic cells in culture. Prostate 1997 Aug 1; 32(3): 155–63
Lepor H. Pathophysiology, epidemiology, and natural history of benign prostatic hyperplasia. Rev Urol 2004; 6 Suppl. 9: S3–10
Thomas LN, Douglas RC, Vessey JP, et al. 5α-reductase type 1 immunostaining is enhanced in some prostate cancers compared with benign prostatic hyperplasia epithelium. J Urol 2003 Nov; 170: 2019–25
Thomas LN, Lazier CB, Gupta R, et al. Differential alterations in 5α-reductase type 1 and type 2 levels during development and progression of prostate cancer. Prostate 2005 May 15; 63(3): 231–9
Titus MA, Gregory CW, Ford 3rd OH, et al. Steroid 5α-reductase isozymes I and II in recurrent prostate cancer. Clin Cancer Res 2005 Jun 15; 11(12): 4365–71
Kaufman KD. Androgens and alopecia. Mol Cell Endocrinol 2002 Dec 30; 198(1–2): 89–95
Marks LS. 5α-reductase: history and clinical importance. Rev Urol 2004; 6 Suppl. 9: S11–21
Marberger M. Drug insight: 5α-reductase inhibitors for the treatment of benign prostatic hyperplasia. Nat Clin Pract Urol 2006 Sep; 3(9): 495–503
Xu Y, Dalrymple SL, Becker RE, et al. Pharmacologic basis for the enhanced efficacy of dutasteride against prostatic cancers. Clin Cancer Res 2006 Jul 1; 12(13): 4072–9
Thomas LN, Douglas RC, Lazier CB, et al. Type 1 and type 2 5αlpha-reductase expression in the development and progression of prostate cancer. Eur Urol 2008; 53(2): 244–52
Thomas LN, Douglas RC, Lazier CB, et al. Levels of 5alpha-reductase type 1 and type 2 are increased in localized high grade compared to low grade prostate cancer. J Urol 2008 Jan; 179(1): 147–51
Andriole G, Bostwick D, Brawley O, et al. Chemoprevention of prostate cancer in men at high risk: rationale and design of the Reduction by Dutasteride of Prostate Cancer Events (REDUCE) trial. J Urol 2004 Oct 1; 172(4): 1314–7
Andriole GL, Roehrborn C, Schulman C, et al. Effect of dutasteride on the detection of prostate cancer in men with benign prostatic hyperplasia. Urology 2004 Sep; 64(3): 537–43
Clark RV, Hermann DJ, Cunningham GR, et al. Marked suppression of dihydrotestosterone in men with benign prostatic hyperplasia by dutasteride, a dual 5α-reductase inhibitor. J Clin Endocrinol Metab 2004 May; 89(5): 2179–84
GlaxoSmithKline. Prescribing information: Avodart® (dutasteride) soft gelatin capsules. Triangle Park (NC): GlaxoSmithKline, 2004 Sep
GlaxoSmithKline UK. Avodart: summary of prescribing information [online]. Available from URL: http://emc.medicines.org.uk [Accessed 2005 Aug 2]
Critchley P, Brin S, Komas B, et al. Dutasteride: clinical investigators brochure (US). Triangle Park (NC): GlaxoSmithKline, 2002
Frye SV. Discovery and clinical development of dutasteride, a potent dual 5α-reductase inhibitor. Curr Top Med Chem 2006; 6(5): 405–21
Roehrborn CG, Boyle P, Nickel JC, et al. Efficacy and safety of a dual inhibitor of 5alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. ARIA 3001, ARIA 3002 and ARIA 3003 study investigators. Urology 2002 Sep; 60(3): 434–41
Debruyne F, Barkin J, van Erps P, et al. Efficacy and safety of long-term treatment with the dual 5alpha-reductase inhibitor dutasteride in men with symptomatic benign prostatic hyperplasia. Eur Urol 2004 Oct; 46(4): 488–95
Roehrborn CG, Marks LS, Fenter T, et al. Efficacy and safety of dutasteride in the four-year treatment of men with benign prostatic hyperplasia. Urology 2004 Apr; 63(4): 709–15
Botto H, Lan O, Poulain JE, et al. Effect of dutasteride on reduction of plasma DHT following finasteride therapy in patients with benign prostatic hyperplasia [in French]. Prog Urol 2005 Dec; 15(6): 1090–5
Wurzel R, Ray P, Major-Walker K, et al. The effect of dutasteride on intraprostatic dihydrotestosterone concentrations in men with benign prostatic hyperplasia. Prostate Cancer Prostatic Dis 2007; 10(2): 149–54
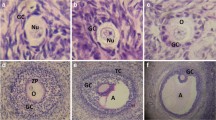
Andriole GL, Humphrey P, Ray P, et al. Effect of the dual 5-α-reductase inhibitor dutasteride on markers of tumor regression in prostate cancer. J Urol 2004 Sep; 172(3): 915–9
Gleave M, Qian J, Andreou C, et al. The effects of the dual 5α-reductase inhibitor dutasteride on localized prostate cancer: results from a 4-month pre-radical prostatectomy study. Prostate 2006; 66(15): 1674–85
Olsen EA, Hordinsky M, Whiting D, et al. The importance of dual 5α-reductase inhibition in the treatment of male pattern hair loss: results of a randomized placebo-controlled study of dutasteride versus finasteride. J Am Acad Dermatol 2006 Dec; 55(6): 1014–23
Roehrborn CG, Boyle P, Gould AL, et al. Serum prostate-specific antigen as a predictor of prostate volume in men with benign prostatic hyperplasia. Urology 1999 Mar; 53(3): 581–9
Bosch JL, Bohnen AM, Groeneveld FP. Validity of digital rectal examination and serum prostate specific antigen in the estimation of prostate volume in community-based men aged 50 to 78 years: the Krimpen Study. Eur Urol 2004 Dec; 46(6): 753–9
Roehrborn CG, Siami P, Barkin J. The effects of dutasteride, tamsulosin and combination therapy on lower urinary tract symptoms in men with benign prostatic hyperplasia and prostatic enlargement: 2-year results from the CombAT study. J Urol 2008 Feb; 179(2): 616–21
Andriole GL, Marberger M, Roehrborn CG. Clinical usefulness of serum prostate specific antigen for the detection of prostate cancer is preserved in men receiving the dual 5α-reductase inhibitor dutasteride. J Urol 2006 May; 175(5): 1657–62
Lazier CB, Thomas LN, Douglas RC, et al. Dutasteride, the dual 5α-reductase inhibitor, inhibits androgen action and promotes cell death in the LNCaP prostate cancer cell line. Prostate 2004 Feb 1; 58(2): 130–44
Schmidt LJ, Murillo H, Tindall DJ. Gene expression in prostate cancer cells treated with the dual 5α-reductase inhibitor dutasteride. J Androl 2004 Nov 31; 25(6): 944–53
McCrohan AM, Morrissey C, O’Keane C, et al. Effects of the dual 5α-reductase inhibitor dutasteride on apoptosis in primary cultures of prostate cancer epithelial cells and cell lines. Cancer 2006; 106(12): 2743–52
Amory JK, Wang C, Swerdloff RS, et al. The effect of 5α-reductase inhibition with dutasteride and finasteride on semen parameters and serum hormones in healthy men. J Clin Endocrinol Metab 2007 May; 92(5): 1659–65
Clark RV, Matsumoto AM. Bone density, bone metabolism markers and lipid profiles in healthy men are unaffected by the novel dual 5α-reductase inhibitor dutasteride [abstract no. 1796]. J Urol 2003; 169 Suppl.: 479
GlaxoSmith Kline. GlaxoSmithKline clinical trial register — dutasteride study no.: ARIA 1012 [online]. Available from URL: http://www.gsk.com/index.htm [Accessed 2005 Feb 23]
Marks LS, Roehrborn CG. Duration of dihydrotestosterone suppression following discontinuation of dutasteride: implications for missed doses [abstract no. 914]. J Urol 2004; 171(4): 242
Costa F, Walls RG. The dual 5α-reductase inhibitor dutasteride is safe and effective in men with benign prostatic hyperplasia receiving a PDE-5 inhibitor [abstract no. 1368]. J Urol 2004 Apr; 171 Suppl. 4: 360
McNicholas T, Tamella T, Harkaway R. The novel dual 5α-reductase inhibitor dutasteride is well tolerated with the concomitant use of commonly prescribed cardiovascular medications and PDE-5 inhibitors [abstract no. 287]. Eur Urol Suppl 2003; 2(1): 74
GlaxoSmith Kline. GlaxoSmithKline clinical trial register — dutasteride study no.: ARI10015 [online]. Available from URL: http://www.gsk.com/index.htm [Accessed 2005 Feb 23]
Clark R, Haberer 1. The dual 5α-reductase inhibitor dutasteride is well tolerated and has no effect on the pharmacokinetic profiles of tamsulosin or terazosin when used in combination in healthy male volunteers [abstract no. 840]. Eur Urol Suppl 2005; 4(3): 212
O’Leary MP, Roehrborn C, Andriole G, et al. Improvements in benign prostatic hyperplasia-specific quality of life with dutasteride, the novel dual 5αlpha-reductase inhibitor. BJU Int 2003; 92(3): 262–6
Marberger M, Roehrborn CG, Marks LS, et al. Relationship among serum testosterone, sexual function, and response to treatment in men receiving dutasteride for benign prostatic hyperplasia. J Clin Endocrinol Metab 2006 Jan 24; 91(3): 1323–8
Te AE, Kaplan S. Dutasteride provides improvement in urodynamic parameters over 2 years: analysis of data from the phase III dutasteride studies [abstract no. 1363]. J Urol 2004 Apr; 171 (4 Suppl.): 359
Marks LS, Roehrborn CG, Wolford E, et al. The effect of dutasteride on the peripheral and transition zones of the prostate and the value of the transition zone index in predicting treatment response. J Urol 2007 Apr; 177(4): 1408–13
Roehrborn CG, Ray P. Efficacy and tolerability of the dual 5α-reductase inhibitor, dutasteride, in the treatment of benign prostatic hyperplasia in African-American men. Prostate Cancer Prostatic Dis 2006; 9(4): 432–8
Gilling PJ, Jacobi G, Tammela TL, et al. Efficacy of dutasteride and finasteride for the treatment of benign prostate hyperplasia: results of the 1-year Enlarged Prostate International Comparator Study (EPICS) [abstract no. U051]. BJU Int 2005 Feb; 95 (1 Suppl.): 12
Hagerty J, Ginsberg PC, Metro MJ, et al. A prospective, comparative study of the onset of symptomatic benefit of dutasteride versus finasteride in men with benign prostatic hyperplasia in everyday clinical practice [abstract no. 1353]. J Urol 2004 Apr; 171 Suppl. 4: 356
Roehrborn CG, Lukkarinen O, Mark S, et al. Long-term sustained improvement in symptoms of benign prostatic hyperplasia with the dual 5α-reductase inhibitor dutasteride: results of 4-year studies. BJU Int 2005 Sep; 96(4): 572–7
Gittelman M, Ramsdell J, Young J, et al. Dutasteride improves objective and subjective disease measures in men with benign prostatic hyperplasia and modest or severe prostate enlargement. J Urol 2006 Sep; 176(3): 1045–50
Barkin J, Guimaraes M, Jacobi G, et al. α-Blocker therapy can be withdrawn in the majority of men following initial combination therapy with the dual 5 α-reductase inhibitor dutasteride. Eur Urol 2003 Oct; 44(4): 461–6
AUA Practice Guidelines Committee. AUA guideline on management of benign prostatic hyperplasia (2003). Chapter 1: diagnosis and treatment recommendations. J Urol 2003 Aug 1; 170(2): 530–47
Barry MJ, Williford WO, Chang Y, et al. Benign prostatic hyperplasia specific health status measures in clinical research: how much change in the American Urological Association symptom index and the Benign Prostatic Hyperplasia Impact Index is perceptible to patients? J Urol 1995; 154: 1770–4
GlaxoSmith Kline. GlaxoSmithKline clinical trial tegister — dutasteride study no.: ARI40001 — year 1 [online]. Available from URL: http://www.gsk.com/index.htm [Accessed 2005 Feb 23]
O’Leary MP, Roehrborn CG, Black L, et al. Dutasteride significantly improves quality of life measures in patients with enlarged prostate. Prostate Cancer Prostatic Dis. Epub 2007 Jun 26
Roehrborn C, Heaton JPW. Medical management for BPH: the role of combination therapy. Eur Urol Suppl 2006; 5(12): 716–21
Marberger M, Harkaway R, de la Rosette J. Optimising the medical management of benign prostatic hyperplasia. Eur Urol 2004 Apr; 45(4): 411–9
Schulman C, Pommerville P, Hofner K, et al. Long-term therapy with the dual 5α-reductase inhibitor dutasteride is well tolerated in men with symptomatic benign prostatic hyperplasia. BJU Int 2006 Jan; 97(1): 73–9
Boehringer Ingelheim Pharmaceuticals, Inc. Ridgefield (CT). Flomax® (tamsulosin hydrochloride) capsules, 0.4mg. US prescribing information [online]. Available from URL: http://www.boehringer-ingelheim.com [Accessed 2007 Oct 6]
Tammela T. Benign prostatic hyperplasia: practical treatment guidelines. Drugs Aging 1997; 10(5): 349–66
Wei JT, Calhoun E, Jacobsen SJ. Urologic diseases in America project: benign prostatic hyperplasia. J Urol 2005 Apr; 173(4): 1256–61
American Cancer Society. Cancer facts and figures 2006. Atlanta (GA): American Cancer Society, 2006
Issa MM, Fenter TC, Black L, et al. An assessment of the diagnosed prevalence of diseases in men 50 years of age or older. Am J Manag Care 2006 Mar; 12 (4 Suppl.): S83–9
Bartsch G, Fitzpatrick JM, Schalken JA, et al. Consensus statement: the role of prostate-specific antigen in managing the patient with benign prostatic hyperplasia. BJU Int 2004; 93 Suppl. 1: 27–9
Kaplan S, Naslund M. Public, patient, and professional attitudes towards the diagnosis and treatment of enlarged prostate: a landmark national US survey. Int J Clin Pract 2006 Oct; 60(10): 1157–65
Kaplan SA. AUA guidelines and their impact on the management of BPH: an update. Rev Urol 2004; 6 Suppl. 9: S46–52
Chapple CR. Pharmacological therapy of benign prostatic hyperplasia/lower urinary tract symptoms: an overview for the practising clinician. BJU Int 2004 Sep; 94(5): 738–44
Kaplan SA, McConnell JD, Roehrborn CG, et al. Combination therapy with doxazosin and finasteride for benign prostatic hyperplasia in patients with lower urinary tract symptoms and a baseline total prostate volume of 25 ml or greater. J Urol 2006 Jan; 175(1): 217–20
Emberton M. Understanding patient attitudes towards BPH treatment: results from the PROBE survey [abstract no. 15]. Eur Urol Suppl 2005; 4(3): 6
de la Rosette J, Alivizatos G, Madersbacher S. Guidelines on benign prostatic hyperplasia (2006). European Association of Urology [online]. Available from URL: http://uroweb.org [Accessed 2006 Oct 12]
de la Rosette J. Optimising assessment and treatment decisions for men with BPH. Eur Urol Suppl 2006; 5(12): 710–5
McKeage K, Plosker GL. Alfuzosin: a review of the therapeutic use of the prolonged-release formulation given once daily in the management of benign prostatic hyperplasia. Drugs 2002; 62(4): 633–53
Fulton B, Wagstaff AJ, Sorkin EM. Doxazosin: an update of its clinical pharmacology and therapeutic applications in hypertension and benign prostatic hyperplasia. [published erratum appears in Drugs 1995; 49 (2): 304]. Drugs 1995; 49: 295–320
Cooper KL, McKiernan JM, Kaplan SA. α-Adrenoceptor antagonists in the treatment of benign prostatic hyperplasia. Drugs 1999; 57(1): 9–17
Croom KF, Wagstaff AJ. Management of benign prostatic hyperplasia: defining the role of tamsulosin. Dis Manage Health Outcomes 2004; 12(5): 337–50
Gillis JC, Wilde MI. Management of benign prostatic hyperplasia: defining the roles of terazosin and finasteride. Dis Manage Health Outcomes 1997 Dec; 2: 302–17
Schwinn DA, Price DT, Narayan P. α1-Adrenoceptor subtype selectivity and lower urinary tract symptoms. Mayo Clin Proc 2004; 79(11): 1423–34
Vela-Navarrete R, Gonzalez-Enguita C, Garcia-Cardoso JV, et al. The impact of medical therapy on surgery for benign prostatic hyperplasia: a study comparing changes in a decade (1992–2002). BJU Int 2005 Nov; 96(7): 1045–8
Boyle P, Roehrborn C, Harkaway R, et al. 5α reductase inhibition provides superior benefits to a blockade by preventing AUR and BPH-related surgery. Eur Urol 2004; 45(5): 620–7
Watson V, Ryan M, Brown CT, et al. Eliciting preferences for drug treatment of lower urinary tract symptoms associated with benign prostatic hyperplasia. J Urol 2004; 172(61): 2321–5
Nickel JC. Comparison of clinical trials with finasteride and dutasteride. Rev Urol 2004; 6 Suppl. 9: S31–9
Andriole G, Djavan B, Fleshner N, et al. The case for prostate cancer screening with prostate-specific antigen. Eur Urol Suppl 2006; 5: 737–45
Naslund MJ, Gilsenan AW, Midkiff KD, et al. Prevalence of lower urinary tract symptoms and prostate enlargement in the primary care setting. Int J Clin Pract 2007 Sep; 61(9): 1437–45
Marks LS, Andriole GL, Fitzpatrick JM, et al. The interpretation of serum prostate specific antigen in men receiving 5α-reductase inhibitors: a review and clinical recommendations. J Urol 2006 Sep; 176(3): 868–74
Thompson IM, Chi C, Ankerst DP, et al. Effect of finasteride on the sensitivity of PSA for detecting prostate cancer. J Natl Cancer Inst 2006 Aug 16; 98(16): 1128–33
Kristal AR, Arnold KB, Schenk JM, et al. Race/ethnicity, obesity, health related behaviors and the risk of symptomatic benign prostatic hyperplasia: results from the prostate cancer prevention trial. J Urol 2007 Apr; 177(4): 1395–400; quiz 1591
Desgrandchamps F, Droupy S, Irani J, et al. Effect of dutasteride on the symptoms of benign prostatic hyperplasia, and patient quality of life and discomfort, in clinical practice. BJU Int 2006 Jul; 98(1): 83–8
Pfizer Labs. Prescribing information: Viagra® (sildenafil citrate) [online]. Available from URL: http://www.viagra.com [Accessed 2005 Mar 17]
Emberton M, Zinner N, Michel MC, et al. Managing the progression of lower urinary tract symptoms/benign prostatic hyperplasia: therapeutic options for the man at risk. BJU Int 2007 Aug; 100(2): 249–53
McConnell JD, Roehrborn CG, Bautista OM, et al. The long-term effect of doxazosin, finasteride and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med 2003 Dec; 349(25): 2387–98
Merck & Co.. Prescribing information: Proscar® (finasteride) tablets [online]. Available from URL: http://www.proscar.com [Accessed 2005 Mar 17]
Roehrborn CG, Barkin J, Quast D, et al. COMBAT and MTOPS: a comparison of the study designs and study populations [abstract no. 938]. Urology 2006; 68 Suppl. 1: 107–8
Siami P, Roehrborn CG, Barkin J, et al. Combination therapy with dutasteride and tamsulosin in men with moderate-to-severe benign prostatic hyperplasia: the CombAT (Combination of Avodart and Tamsulosin) trial rationale and study design. Cont Clin Trials 2007 Nov; 28(6): 770–9
International Agency for Research on Cancer. GLOBOCAN 2002 [online]. Available from URL: http://www-dep.iarc.fr/ [Accessed 2006 Aug 10]
Roehrborn CG, Lotan Y. The motion: prevention of prostate cancer with a 5α-reductase inhibitor is feasible. Eur Urol 2006 Feb; 49(2): 396–400
Chan JM, Jou RM, Carroll PR. The relative impact and future burden of prostate cancer in the United States. J Urol 2004 Nov; 172(5 Pt 2): S13–7
Turini M, Redaelli A, Gramegna P, et al. Quality of life and economic considerations in the management of prostate cancer. Pharmacoeconomics 2003; 21(8): 527–41
Roehrborn C. Insights into the relationships between prostatic disorders and their potential impact on future urologic practice. Eur Urol Suppl 2006; 5(12): 698–703
Iczkowski KA, Qiu J, Qian J, et al. The dual 5-α-reductase inhibitor dutasteride induces atrophic changes and decreases relative cancer volume in human prostate. Urology 2005 Jan; 65(1): 76–82
Thompson IM, Goodman PJ, Tangen CM, et al. The influence of finasteride on the development of prostate cancer. N Engl J Med 2003 Jul 17; 349(3): 215–24
Schalken J. New developments in the pathobiology of prostate disease. Eur Urol Suppl 2006; 5: 729–36
Akduman B, Crawford ED. The PCPT: new findings, new insights, and clinical implications for the prevention of prostate cancer. Eur Urol Suppl 2006; 5(9): 634–9
Andriole G, Brawley O, Somerville MC, et al. Chemoprevention of prostate cancer: racial differences in baseline characteristics of men in the REDUCE trial [abstract no. 26]. 2006 Prostate Cancer Symposium; 2006 Feb 24–26; San Francisco (CA)
Gomella LG. Chemoprevention using dutasteride: the REDUCE trial. Curr Opin Urol 2005 Jan; 15(1): 29–32
Nickel JC, Roehrborn CG, O’Leary MP, et al. The relationship between prostate inflammation and lower urinary tract symptoms: examination of baseline data from the REDUCE trial. Eur Urol. Epub 2007 Nov 20
Andriole G, Bostwick D, Civantos F, et al. The effects of 5α-reductase inhibitors on the natural history, detection and grading of prostate cancer: current state of knowledge. J Urol 2005 Dec; 174(6): 2098–104
Andriole G. 5α-reductase inhibitors and chemoprevention: the PCPT and beyond. Eur Urol Suppl 2006; 5(12): 746–51
Fleshner N, Gomella LG, Cookson MS, et al. Delay in the progression of low-risk prostate cancer: rationale and design of the reduction by dutasteride of clinical progression events in expectant management (redeem) trial. Contemp Clin Trials 2007 Nov; 28(6): 763–9
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keam, S.J., Scott, L.J. Dutasteride. Drugs 68, 463–485 (2008). https://doi.org/10.2165/00003495-200868040-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200868040-00008