Abstract
Pseudomonas aeruginosa is a non-capsulate and non-sporing Gram-negative bacillus that most commonly affects the lower respiratory system in humans. Burkholderia (previously Pseudomonas) cepacia has emerged as an important respiratory pathogen in patients with cystic fibrosis (CF). The ability of P. aeruginosa to persist and multiply in moist environments and equipment, such as humidifiers in hospital wards, bathrooms, sinks and kitchens, maybe of importance in cross-infection. P. aeruginosa infections of the lower respiratory tract can range in severity from colonisation (without an immunological response) to a severe necrotising bronchopneumonia. Infection is seen in patients with CF and other chronic lung diseases such as non-CF bronchiectasis. In patients with CF, once P. aeruginosa is established in the airways it is almost impossible to eradicate, but prior to this, aggressive treatment can delay the development of chronic infection. 30 to 40% of the present paediatric population with CF will have chronic pseudomonal infection.
B. cepacia has a particular predisposition to infect patients with CF and may be distinguished from P. aeruginosa by accelerated lung disease in about one-third of patients. Overwhelming septicaemia and necrotising pneumonia are well described (cepacia syndrome); events that are rare with P. aeruginosa. With the propensity for social cross-infection, segregation policies have been accepted as means of controlling outbreaks.
A number of antipseudomonal agents are available. The most commonly used are the extended-spectrum penicillins, aminoglycosides, cephalosporins, fluoro-quinolones, polymixins and the monobactams. An aminoglycoside with a β-lactam penicillin is usually considered to be the first line treatment. No trial has shown any significant clinical advantage of any particular combination regimen over another. The emergence of resistance continues to be a concern. Pipericillin, piperacillin/tazobactam and meropenem have good but equivalent antibacterial activity against P. aeruginosa. However, B. cepacia is characterised by in vitro resistance to colistin (colomycin), aminoglycosides and ciprofloxacin but better susceptibility to ceftazidime. Nebulised delivery of antipseudomonal antibiotics is thought to prevent recurrent exacerbations, reduce antibiotic usage and maintain lung function, particularly in patients with CF. Colistin, tobramycin and gentamicin are currently the most commonly prescribed nebulised antibiotics. Much effort is directed at treating chronic P. aeruginosa infection but as chronic infection is seldom if ever eradicated when first established, prevention is preferable. Early intensive treatment for P. aeruginosa infection is advocated in order to maintain pulmonary function and postpone the onset of chronic P. aeruginosa infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The term Pseudomonad describes a large group of aerobic Gram-negative bacilli saprophytes commonly found in soil, water and other moist environments. Pseudomonas aeruginosa is the species most commonly associated with human disease, particularly that affecting the lower respiratory tract. Burkholderia (previously Pseudomonas) cepacia has emerged as an important respiratory pathogen in immunocompromised patients and in patients with cystic fibrosis (CF). This article reviews the current antibacterial chemotherapy options for respiratory pseudomonal infection with particular relevance to CF.
1. Bacteriology and Pathogenesis
Molecular analyses of the Pseudomonad group have led to revised taxonomic classifications and some species have been allocated to new genera which include Burkholderia, Comanonas, Stenotrophomonas and Brevundimonas. The reasons for the growing importance of P. aeruginosa as an opportunistic pathogen lie in its resistance to many antibiotics and disinfectants, its putative virulence factors and the increasing number of immunocompromised patients as a result of increasing age, underlying disease and immunosuppressive therapy.
P. aeruginosa is a Gram-negative bacillus, non-capsulate and non-sporing. Most strains produce diffusible coloured pigments pyocyanin (green-blue) and pyoverdin (yellow-green fluorescent). Some strains appear mucoid because of the abundance of a polysaccharide capsule (particularly common in patients with CF). This capsule protects the organism and also anchors it to cell surfaces. Lipopolysaccharide endotoxin is a major cell wall antigen in P. aeruginosa; the lipid A component mediates the various biological effects of the sepsis syndrome. Exotoxin A is an important virulence factor blocking protein synthesis in eukaryotic cells and mediates tissue damage in chronic pulmonary infections.
B. cepacia (previously best known as the causative agent of soft rot of onions; cepacia, Latin = onion) has innate resistance to antibacterial agents and concerns have arisen regarding transmission by social contact. With the exception of pulmonary infections, B. cepacia has a relatively low level of virulence and laboratory identification is aided by the use of selective media and multitest identification systems.[1–3]
2. Epidemiology
The ability of P. aeruginosa to persist and multiply in moist environments, soil detritus and equipment such as humidifiers in hospital wards, urinary catheters, bathroom sinks[4] and kitchens is of particular importance in cross-infection. In the community, carriage rate is less than in the hospital environment. In a large survey of 47 679 P. aeruginosa isolates in Bristol UK,[5] 18% came from the primary care physician. From the inpatient isolates (n = 17 440), 39% were isolated from urine (39% of these catheter specimens), 36% from skin and soft tissue and 18% from the lower respiratory tract. 20% of the isolates originated from surgical wards, 18% care of the elderly, 13% general medicine, 10% paediatrics and 9% intensive care wards.
The natural habitats of B. cepacia have been described as soil, water and vegetation but extensive surveillance studies have shown that culture of B. cepacia from natural sources is surprisingly difficult. Although airborne dissemination may present a small risk of acquisition, the use of bacterial fingerprinting techniques have provided compelling evidence that person-to-person spread accounts for the highest risk of acquisition of infection through direct exchange of respiratory secretions. Different B. cepacia strains differ greatly in their rates of transmission. In the UK, a transmissible strain has been identified which is identical to a strain from Ontario, Canada. This strain labelled ET12 or UK ‘epidemic’ strain has a unique form of pilus designated ‘cable pilus’ because of its length (2μm) and intertwining properties. Recently molecular analyses of type strains and clinical isolates have revealed that isolates identified previously as B. cepacia belong to at least 3 distinct species and have increased concerns regarding the reliability of current laboratory detection and identification systems.[6]
3. Clinical Respiratory Features
P. aeruginosa infections of the lower respiratory tract can range in severity from only colonisation (without an immunological response) to a severe necrotising bronchopneumonia. Infection is seen in patients with CF and other chronic lung diseases such as non-CF bronchiectasis, severe chronic obstructive pulmonary disease (COPD) and also patients in the intensive care unit. In patients with CF, once P. aeruginosa is established in the airways it is almost impossible to eradicate. Historically, more than 60% of these patients are colonised with P. aeruginosa by adolescence. However, there is a younger cohort of adult patients with CF presently leaving paediatric units with early aggressive therapy policies who do not develop chronic pseudomonal infection until much later and only about 30 to 40% of the paediatric population will have chronic pseudomonal infection. Over 60% of isolates have a mucoid morphology in contrast to those found in other chronic lung disease.[3]
Patients with non-CF bronchiectasis are more commonly infected with uncapsulated Haemophilus influenza, Streptococcus pneumoniae and Moraxella catarrhalis, but in those with more severe disease the incidence of non-mucoid and mucoid P. aeruginosa rises. Similarly, in COPD, nosocomial P. aeruginosa infection is more common in those with severe disease [forced expiratory volume in 1 second (FEV1) predicted <40%] perhaps as a consequence of repeated hospital admissions and multiple antibacterial therapy for exacerbations.[7] Pseudomonal pneumonia occurs as a consequence of oro-pharyngeal contamination (sometimes from contaminated nebuliser equipment) or secondary to bacteraemia from an extrapulmonary focus in immunocompromised patients, and presents as an acute toxic illness with high morbidity and mortality. Complications such as abscess or empyema formation are not uncommon.
In the intensive care setting, P. aeruginosa is a common isolate and a cause of nosocomial ventilator-associated pneumonia particularly in the immunocompromised.[8]
B. cepacia has a particular predisposition to infect patients with CF and is distinguished from P. aeruginosa by accelerated lung disease in some patients.[9] Overwhelming septicaemia and necrotising pneumonia are well described; such events are rare with P. aeruginosa. B. cepacia has also been reported to cause chronic respiratory disease in a patient with normal lungs following acquisition from a relation with CF.[10] With the propensity for cross-infection, segregation policies as means of controlling outbreaks are strongly recommended.[11–13] Early UK surveillance studies suggested a maximum prevalence of less than 10% but recent reports have suggested this has risen with some centres approaching the 40% described in the US.[14]
4. Antibacterial Therapy
4.1 Antibacterial Types
In the 1950s mortality rates were high for P. aeruginosa respiratory infection. Colistin (colomycin; polymixin E) was commercially released in 1959 and was the first antibacterial agent with significant in vitro activity against P. aeruginosa. The mechanism of action of polymixins involves interaction with the phospholipids of the cell membrane and disruption of its structure. Unfortunately, clinical efficacy did not match in vitro susceptibility and adverse effects such as neurotoxicity and nephrotoxicity were reported. Later products such as carbenicillin proved more successful but it was not long before resistance against this extended-spectrum penicillin occurred. Other extended-spectrum penicillins have been developed for use. These include carboxypenicillins such as ticarcillin, the ureidopenicillins, for example, azlocillin, and the piperazine penicillins, for example, piperacillin. Ticarcillin is available in conjunction with the β-lactamase inhibitor clavulanic acid. The pharmacokinetics of both are closely matched and like other penicillins are excreted via the kidney. Azlocillin is very active against Pseudomonas spp. and given parenterally; the half-life (t½) is 60 minutes and it is excreted both in urine and bile. Manufacture of azlocillin has ceased, although stocks do exist around the world. Piperacillin may also be administered in conjunction with tazobactam, a potent inhibitor of many β-lactamases, in particular the plasmid mediated enzymes that commonly cause resistance to penicillins and cephalosporins. Rash, urticaria and pruritis are common adverse effects, particularly in patients with CF (up to 30%).[15] Haemolytic anaemia, although rare, has also been reported with piperacillin in patients with CF.[16] The presence of tazobactam enhances and extends the antibiotic spectrum of piperacillin.
Ceftazidime, a cephalosporin, is a commonly used bactericidal agent causing inhibition of cell wall synthesis. It is highly stable to most clinically important β-lactamases produced by both Gram-positive and -negative organisms. It has generally good activity in vitro and advantages include ease of parental administration, no requirement for monitoring drug concentrations, twice daily administration if preferred (3 times daily usage in the US) and low toxicity. It has a serum t½ of 1.8 hours in healthy volunteers and is not metabolised but is excreted unchanged in the urine.
Ciprofloxacin, a fluoroquinolone, has the advantage over other agents in that an oral preparation is available. Oral bioavailibility is between 70 to 80% and a t½ of 5 hours allows twice daily administration regimens. Elimination is partly via hepatic metabolism by cytochrome P450 enzymes, which are inhibited leading to the potential for drug interactions. Constant prophylactic therapy is inadvisable because of a steady increase over time in the minimum inhibitory concentration (MIC) to P. aeruginosa.[17] Such constant therapy will eventually lead to resistance and, hence, we believe this agent should be used sparingly and for special circumstances. Unfortunately, however, it is often the only oral antibiotic effective in patients with CF with P. aeruginosa respiratory infections. Ciprofloxacin (MIC90 0.12 to 0.25 mg/L) is twice as active against P. aeruginosa than other fluoroquinolones such as trovafloxacin (0.25 to 0.5 mg/L), levofloxacin (0.5 to 1.0 mg/L) and sparfloxacin (0.5 to 1.0 mg/L), and 4 times as active as ofloxacin (1.0 mg/L).[18] The use of trovafloxacin is restricted because of the risk of severe hepatic toxicity.
Other β-lactam antibiotics include the carbapenems imipenem and meropenem and the monobactam aztreonam. They were developed to deal with β-lactamase producing Gram-negative organisms resistant to extended-spectrum penicillins. Imipenem, like other β-lactam antibiotics, acts on the synthesis of the cell wall. It is given intravenously and is broken down at the proximal tubule by a dehydropeptidase; hence it is given in combination with cilastatin, a specific inhibitor of this enzyme. Meropenem is similar to imipenem but is not broken down by dehydropeptidase. Aztreonam is a simple monocyclic β-lactam with good activity against Gram-negatives such Pseudomonads but no action against Gram-positive bacteria.
The aminoglycosides are a group of antibiotics with a complex chemical structure resembling each other in antimicrobial, pharmacokinetic characteristics and toxicity. They include gentamicin, tobramycin and amikacin, and act by inhibiting bacterial protein synthesis. They are not absorbed in the gastrointestinal tract and the serum t½ is 2 to 3 hours. Elimination is virtually entirely through glomerular filtration and care with the dosage should be taken in patients with renal impairment. Serum concentrations are measured just prior intravenous administration (trough) and 1 hour after (peak). For gentamicin and tobramycin, the ideal maximum trough and peak concentrations to provide a therapeutic effect and avoid toxicity are 2 and 10 μg/ml, respectively (10 and 30 μg/ml for amikacin). Clinical experience with 3 times daily usage suggests that the trough level above 2 μg/ml is a better marker of potential toxicity than peak levels. It is also likely that frequency of aminoglycoside courses will be found to have an important role in toxicity. There is increasing interest in once-daily administration, which is more convenient than multiple-dose regimens.[19] Animal studies and clinical trials suggest that once-daily administration is as efficacious and no more toxic, and indeed such a regimen is now standard for many patients in the US. However, there is some reluctance for routine use in neutropenic patients because of the potential risk of breakthrough bacteraemia.
Aminoglycosides demonstrate a post-antibiotic effect where bacteria that survive following exposure may not metabolise normally for up to 8 hours afterwards despite undetectable drug concentrations. Increasing oxygen tensions are also reported to augment this post-antibiotic effect. Consequently, the more traditional approach of maintaining serum and tissue concentrations above the MICs for as long as possible may be no more effective than achieving a higher concentration for a short period. Despite the possibility of reduced toxicity with once-daily regimens, serum monitoring particularly the trough is still necessary. As yet no agreed consensus regarding the timing or the interpretation of the post-dose sample concentrations has been reached.
The pharmacokinetics of aminoglycosides, β-lactams and cephalosporins are altered in patients with CF. This is a result of increased renal clearance, liver enzyme induction and a larger volume of distribution due to an increased amount of lean tissue per kilogram bodyweight (as a consequence of malnutrition and paucity of adipose tissue). Larger doses of antibacterials must therefore be given to optimise therapeutic benefit. Aminoglycoside adverse effects such as ototoxicity (high-tone deafness) are more common than previously thought (16% in one case series of patients with CF[20]) but are more common in non-CF related treatment episodes.[21] Nephrotoxicity requires particular precautions in ill patients who also are prone to hypotension and those who are exposed to other nephrotoxic drugs such as loop diuretics and cephalosporins. A summary of antibacterial dosages and adverse effects are given in table I.[22]
4.2 Antibacterial Resistance
The emergence of antibiotic resistance is a concern and there have been numerous testings of clinical P. aeruginosa isolates for susceptibility and resistance.[5,23,24] Data is available from the UK (17 000 isolates),[5] Spain (1000 isolates)[23] and Italy (1000 isolates).[24] Ceftazidime susceptibility was lower in the Spanish and Italian studies compared with the UK (85 and 87% vs 93%). The best susceptibility was for piperacillin/tazobactam of 93% (Spain) closely followed by meropenem 92% (Spain) and 91% (Italy). Ciprofloxacin susceptibility was lower at 77% in Spain, 68% in Italy but 90% in the UK. Susceptibility patterns to ceftazidime, ciprofloxacin, gentamicin, imipenem and piperacillin did not change significantly over the years between 1986 and 1993. However, B. cepacia is characterised by in vitro resistance to colistin and aminoglycosides but less so for ceftazidime compared with P. aeruginosa.[25,26]
4.3 Combination versus Monotherapy
In vitro susceptibility testing offers a biological rationale for selecting antibacterial agents for the treatment of infection. However, the correlation of clinical outcome with in vitro susceptibility is not always guaranteed and patients infected by organisms resistant to antipseudomonal antibiotics may not necessarily fare worse; clinical response to an antibacterial regimen is more important than in vitro sensitivity. The demonstration of in vitro synergy with combination therapies such as antipseudomonal penicillins and aminoglycoside agents, and the earlier clinical disappointment of gentamicin monotherapy and the emergence of resistance with carbenicillin monotherapy, have prompted trials of combination therapy. Combination therapy has long been shown to be more effective in the treatment of tuberculosis and successful in preventing the emergence of the resistance. However, the occurrence of synergy may be unpredictable and traditional methods of reporting strains as ‘resistant’ or ‘susceptible’ may be crude.
Susceptibility patterns of 122 isolates of P. aeruginosa from patients with CF to 5 individual antibiotics (tobramycin, ceftazidime, piperacillin, ticarcillin and imipenim) and 4 antibacterial combinations (tobramycin with the other 4 agents) were evaluated.[27] Synergy was demonstrable against 32% strains with tobramycin plus ticarcillin, 31% with tobramycin plus piperacillin, 39% with tobramycin plus ceftazidime and against 19% with tobramycin plus imipenem. No combination exhibited antagonism. In vitro activity of aztreonam combined with tobramycin and with gentamicin was assessed in 78 clinical isolates of P. aeruginosa and 11 clinical isolates of B. cepacia from patients with CF.[28] Synergy was detected in 56% of P. aeruginosa isolates and 60% of B. cepacia isolates with the aztreonam plus tobramycin combination and in 49% of P. aeruginosa isolates and 82% of B. cepacia isolates with the aztreonam plus gentamicin combination. No antagonism was observed. Monotherapy, particularly with ceftazidime, has been associated with outbreaks of resistance. An epidemic of multiresistant P. aeruginosa in 1983 in the Copenhagen Cystic Fibrosis unit was attributed to the extensive use of ceftazidime.[29] Similarly and more recently, in Liverpool UK,[30] 65 out of 92 P. aeruginosa isolates (from a total of 120 children) were ceftazidime resistant. By molecular techniques, 55 out of 65 children were shown to be infected with the same epidemic strain, which was resistant to azlocillin and imipenem.
The antibacterial practices of 26 physicians in the UK and Republic of Ireland caring for patients with CF was assessed in 1993 by a postal questionnaire.[31] Ceftazidime monotherapy was regularly used by 5 (19%) physicians, although the majority 20 (77%) used combination therapy of a penicillin with an aminoglycoside. 73% of the physicians used the latest sputum microbiological susceptibility results to guide the choice of antibacterial regimen. In a recent double-blind, randomised controlled trial, azlocillin plus placebo were compared with azlocillin plus tobramycin in 76 patients with CF with P. aeruginosa exacerbations.[32] There was no difference in clinical outcomes such as spirometry and sputum bacteriology but combination therapy did lead to a longer clinical remission (as measured by time to readmission for a new exacerbation).
A recent trial has compared once daily intravenous tobramycin 15 mg/kg/day with three times daily intravenous tobramycin in combination therapy with intravenous ceftazidime.[33] Although the numbers were small (n = 22), there was no difference in clinical outcome or adverse effects, suggesting that a once daily regimen may be as effective and well tolerated as a three times daily regimen. Once daily regimens of other aminoglycosides investigated in clinical trials include netilmicin[34] and amikacin (in patients without CF).[35] A large UK trial based in Nottingham is currently further investigating the potential advantages of once daily tobramycin and will have the power to show equal efficacy and toxicity. A combination of gentamicin plus aztreonam was tested in a multicentre trial in Florida, USA.[36] Aztreonam 2g 8 hourly and gentamicin 3 to 5 mg/kg/day in 3 equal doses was given to 57 patients with CF with P. aeruginosa infections. The clinical response was 84% and the combination was generally well tolerated. However, as with many previous trials, there was no control group for comparison.
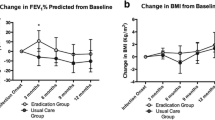
Over the last few years, there has been resurgence in the use of intravenous colistin for P. aeruginosa in patients with CF. Despite P. aeruginosa being fully sensitive to colistin, there has been reluctance in the past to use it because of the potential risk of neuro- and nephrotoxicity. In one study in Leeds, UK, of 71 P. aeruginosa exacerbations in 53 patients with CF, intravenous colistin 2 million units (MU) three times daily was compared with colistin 2MU three times daily plus another antipseudomonal depending on the latest sputum susceptibilities.[37] Both treatments were effective in producing a clinical improvement, although the combination therapy produced a more rapid and greater improvement. However, there were 37 adverse neurological events (dizziness, numbness, tingling, incoordination, unsteadiness and muscle weakness) in the monotherapy group and a similar number in the combination group, but only one patient withdrew from the trial as a consequence. Interestingly, at another UK CF unit, no neurotoxic events were recorded in 52 patients with CF receiving the same regimen of 2MU three times daily intravenously.[38] Both cohorts of patients from the two UK studies were well matched with regard to gender, FEV1 % predicted and body mass index. The authors in the second UK study advocate the more widespread use of colistin.[38]
There have been no double-blind, randomised controlled trials investigating antibacterial chemotherapy for B. cepacia, although an in vitro study of 66 sputum isolates from patients with CF found meropenem to have the best MIC90.[39] The same group found a combination of β-lactam, ciprofloxacin plus tobramycin to have the best synergistic effect. The addition of ciprofloxacin significantly enhanced the killing activities of meropenem. Another study looking at 36 isolates of B. cepacia from blood cultures found 86% of the strains susceptible to ceftazidime.[40] Susceptibilities above 80% were also shown for ciprofloxacin. 69% of the strains exhibited a synergistic effect when ceftazidime was combined with ciprofloxacin. We recommend that first line treatment of exacerbations with both P. aeruginosa and B. cepacia should include ceftazidime and an aminoglycoside with the consideration of adding ciprofloxacin, particularly at late stage disease.
Despite the abundance of in vitro trials, results of in vivo clinical trials are more meaningful. However, more trials need to be adequately powered to investigate the possibility of superiority of new antibacterial agents compared with others. No trial has shown any significant clinical advantage of any particular combination regimen over another. Most clinicians rely on the latest microbiological susceptibility as a guide; aminoglycoside (for example, tobramycin) in combination with a β-lactam penicillin being the most common regimen used. Some centres such as the Copenhagen group advocate the regular use (every 3 months) of intravenous therapy to encourage a slower decline in lung function.[41] However, this must be weighed against the possibility of selecting for resistant bacteria, frequent hospital admissions and therefore risk of cross-infection, disruption of lifestyle and risk of drug sensitisation.
4.4 Desensitisation to Antibacterial Drugs
Occasionally a patient will develop an allergy to parental antibacterial agents, particularly pipericillin,[42] aztreonam[43] and ceftazidime.[44] Given the problems of multidrug resistance, desensitisation to the antibacterial agent may be necessary. In the case of ceftazidime desensitisation,[44] starting with a low dose such as 1mg per hour and doubling the dose every hour by continuous infusion, a rate of 150 to 300 mg/kg/day was reached. For patients who tolerated the maximum infusion rate but reacted adversely to the bolus doses, the procedure was restarted and once the normal daily dosage rate had been achieved, the treatment was completed by continuous intravenous infusion rather than bolus doses. Such a regimen allowed 4 patients out of 6 to have further courses of ceftazidime who had previously exhibited allergic reactions. Similar regimens have been attempted in patients with hypersensitivity reactions to other antibacterials. The intravenous procedure has the advantage of allowing the antibacterial agent to be diluted to permit accurate administration of small quantities of drug with the ability to stop the infusion at the first sign of a reaction.
4.5 Home versus Hospital Therapy
There is good evidence that home intravenous antibacterial therapy for patients with CF is as effective as hospital therapy.[45,46] Clinical improvements are similar and home treatment provides less disruption to personal and family, as well as sleeping patterns. Hospital therapy does allow a greater degree of control of administration of antibacterial agents but the total cost for hospital treatment in one study was twice that of home treatment.[46]
4.6 Nebulised Antibacterials
Aerosol delivery of antibiotics via a nebuliser allows around 10% deposition in the lungs and, although the concentration of the aerosolised antibiotic in the bronchial secretions may not always achieve bactericidal levels, sublethal concentrations may diminish bacterial virulence factors.
Regular use of aerosolised antibacterial agents is now common in patients chronically infected with P. aeruginosa to reduce rate of deterioration. In an analysis of 12 trials of nebulised antibacterials in patients with CF, the overall conclusion was that such treatment does reduce the number of hospital admissions with improvement of lung function.[47] There was no enhancement of clinical effects when used in conjunction with intravenous antibacterial therapy for acute exacerbations. It is recommended to use nebulised agents after physiotherapy and bronchodilators to ensure maximum deposition and protection from bronchoconstriction that usually occurs immediately after administration (up to 10% of those using colistin). Colistin, tobramycin and gentamicin are currently the most commonly prescribed nebulised antibacterial agents.
Colistin is probably the best first choice as P. aeruginosa resistance is rare; however, resistance to B. cepacia is total. Dosages are as follows: colistin 2MU 12 hourly, gentamicin 80mg 12 hourly and tobramycin 80mg 12 hourly. Toxicity studies carried out have shown no renal or ototoxicity, and development of resistance is uncommon, although it may appear occasionally on a temporary basis. With regard to patient safety, it is recommended that nebulisers should be cleaned after every use and no patient should share nebuliser equipment with others.[48] A recent trial compared the administration of inhaled tobramycin 300mg twice daily with placebo twice daily in a total of 520 patients with CF over a period of 26 weeks, alternating one month on and one month off treatment.[49] The tobramycin group had a mean increase of FEV1 of 10% compared to a 2% decline in the placebo group (p < 0.001). The tobramycin group also had better bacterial loads (p < 0.001) and were 26% [95% confidence interval (CI) 2 to 43%] less likely to be hospitalised compared with placebo. The authors suggest that concomitant inhaled tobramycin provides additional benefit in patients with CF. Evidence of superiority of this regimen over other inhaled drugs and regimens is not currently available.
Newer technology such as the adaptive aerosol delivery (AAD) system has been found to have potential advantages over the older traditional nebulisers.[50,51] It is a breath-enhanced nebuliser which delivers a precise and reproducible drug dose, adapting to each individual’s breathing pattern and delivering aerosol during the first 50% of inspiration only rather than the traditional method of generating a continuous aerosol cloud with environmental contamination. The AAD system will not deliver aerosol if the patient interrupts treatment because of, for example, coughing or nasal breathing. As a result, the nebuliser dose delivered with this system may be reduced without a loss of effect; clinical trials are awaited.
Chronic P. aeruginosa infection in patients with non-CF bronchiectasis should have nebulised antibacterials analogous to the patients with CF in conjunction with regular postural drainage and intravenous antibacterials for acute exacerbations.[52] This author prefers gentamicin 80mg twice daily,[52] although few trials have been performed to determine which nebulised antibiotic may have a better clinical effect.
4.7 Delaying Infection with Pseudomonas aeruginosa in the Lung
Chronic pulmonary infection with P. aeruginosa develops in most patients with CF and is associated with deterioration in lung function. Much effort is directed at treating chronic infection but as chronic infection is almost impossible to eradicate when first established, prevention is preferable. A prospective study (n = 26) in Copenhagen[53] found treatment with colistin inhalation twice daily and oral ciprofloxacin for 3 weeks every time P. aeruginosa was isolated in patients never treated before with antipseudomonal agents resulted in fewer chronic infections than no treatment.
The same Danish group use a ‘3-step protocol’ in all non-infected patients. Step 1 (first isolate P. aeruginosa): 3 weeks colistin 1MU twice daily plus ciprofloxacin; step 2 (the following isolate): 3 weeks colistin 2MU three times daily plus ciprofloxacin; step 3 (third isolate within 6 months): 3 months colistin 2MU three times daily plus ciprofloxacin. The same group has shown that 3 months treatment was superior to the 3 weeks treatment in delaying the time until recurrence of P. aeruginosa in the sputum. A follow-up study on the patients treated with such a regimen between 1989 and 1993 was compared with historic controls between 1983 and 1986 and found that early intensive treatment for early P. aeruginosa infection maintained pulmonary function in addition to postponing the onset of chronic P. aeruginosa infection (16 vs 72% over 44 months).[54] Latest figures from the Danish group have shown that with early aggressive antibacterial therapy, the probability of not developing chronic infection after first isolating P. aeruginosa in the sputum after 7 years was more than 80%.[55] Although these data are compelling, it might be difficult to reproduce these results in countries that do not reimburse for this intensity of healthcare, including the full costs of regular clinic visits with the same set of physicians, the costs of medications, and the costs of regular assessments of pulmonary function and sputum culture with sensitivity testing.
4.8 Antimicrobial Peptides — Potential Future Antibacterial Agents?
Mammalian epithelial surfaces are remarkable for their ability to provide critical physiological functions in the face of frequent microbial challenges. The fact that these mucosal surfaces remain infection-free in the normal host suggests that highly effective mechanisms of host defence have evolved to protect these environmentally exposed tissues. Throughout the animal and plant kingdoms, endogenous genetically encoded antimicrobial peptides have been shown to be key elements in the response to epithelial compromise and microbial invasion. In mammals, a variety of such peptides have been identified, including the well-characterised defensins and cathelicidins. A major source of these host defence molecules is circulating phagocytic leucocytes. However, more recently, it has been shown those resident epithelial cells of the skin and respiratory, alimentary and genitourinary tracts also synthesise and release antimicrobial peptides. Both in vitro and in vivo data support the hypothesis that these molecules are important contributors to intrinsic mucosal immunity. Alterations in their level of expression or biological activity can predispose the organism to microbial infection.[56] Bronchoalveolar lavage fluids from patients with CF have found significantly lower levels of antimicrobial peptides than in patients without CF.[57] In vitro studies of two antimicrobial peptides have shown useful antibacterial activity against P. aeruginosa suggesting a potential role for such agents in the treatment of patients with CF infected with multidrug-resistant P. aeruginosa.[58] More data on antimicrobial peptide agents is awaited before their potential clinical role is fully understood.
5. Summary
Antibacterial therapy in patients with chronic lung disease infected with Pseudomonas spp. aims to prevent, eradicate and reduce lower respiratory tract infection and eradicate Pseudomonas spp. if possible. The clinical condition may deteriorate more rapidly after chronic infection becomes established particularly patients with CF.
Exacerbations are treated with a combination of aminoglycoside and most commonly a β-lactam; the choice depending on previous clinical response with some guidance from identification and susceptibility of bacteria isolated from the sputum. Table II describes the antibacterial clinical guidelines in place at the authors’ adult CF centre for patients with established chronic pseudomonal respiratory infection in order of preference. If in vitro resistance to the antibacterial is shown but clinical improvement has been demonstrated during previous courses, the same regimen will be used again. Such guidelines help preserve antibacterial sensitivity and minimise excessive drug expenditure.
For the maintenance treatment of chronic pseudomonal infection, there is good evidence, especially in patients with CF, that nebulised antipseudomonals, particularly aminoglycosides and colistin, have a role in maintaining respiratory function. The debate between regular intravenous therapy and treatment only for exacerbations will continue until good randomised controlled trials have directly compared both regimens.
References
Murray PR, Rosenthal KS, Kobayashi GS, et al. Pseudomonas and related organisms. In: Murray PR, Rosenthal KS, Kobayashi GS, et al., editors. Medical microbiology. 3rd ed. New York: Mosby-Year Book, 1998: 258–64
Govan GRW. Pseudomonads and non-fermenters: opportunistic infection: cystic fibrosis; meliodosis. In: Greenwood D, Slack RC, Peutherer JF, editors. Medical microbiology: a guide to microbial infections: pathogenesis, immunity, laboratory diagnosis and control. 15th ed. London: Churchill Livingstone, 1997: 284–9
Govan JRW, Nelson JW. Microbiology of cystic fibrosis lung infections: themes and issues. J R Soc Med 1993; 86 Suppl. 20: 11–18
Doring G, Jansen S, Noll H, et al. Distribution and transmission of Pseudomonas aeruginosa and Burkholderia cepacia in a hospital ward. Pediatr Pulmonol 1996; 21(2): 90–100
Spencer RC. An 8 year microbe base survey of the epidemiology, frequency, and antibiotic susceptibility of Pseudomonas aeruginosa hospital isolates in the United Kingdom. J Antimicrob Chemother 1996; 37: 295–301
Govan JRW, Hughes JE, Vandamme P. Burkholderia cepacia: medical, taxonomic and ecological issues. J Med Microbiol 1996; 45: 395–407
Eller J, Ede A, Scaberg T. Infective exacerbations of chronic bronchitis. Chest 1998; 113: 1542–8
Bergmans D, Bonten M. Colonization and infection with Pseudomonas aeruginosa in intensive care: endogenous or exogenous origin? In: J-L Vincent, editor. Yearbook of intensive care and emergency medicine. New York: Springer, 1999: 131–40
Mudhi K, Edenborough FP, Gumery L, et al. Outcome of patients colonised with Burkholderia cepacia in a Birmingham adult cystic fibrosis clinic and the end of an epidemic. Thorax 1996; 51(4): 374–7
Ledson MJ, Gallagher MJ, Walshaw MJ. Chronic Burkholderia cepacia bronchiectasis in a non-cystic fibrosis individual. Thorax 1998; 53: 430–2
Smith DL, Gumery LB, Smith EG, et al. Epidemic of Burkholderia cepacia in an adult cystic fibrosis unit: evidence of person-to-person transmission. J Clin Microbiol 1993; 31(11): 3017–22
Smith DL, Smith EG, Gumery LB, et al. Pseudomonas cepacia infection in cystic fibrosis [letter]. Lancet 1994; 339: 252
Stableforth DE, Smith DL. Pseudomonas cepacia in cystic fibrosis. Thorax 1994; 49(7): 629–30
Spencer RC. The emergence of epidemic, multiple-antibiotic-resistant Stenotrophomonas (Xanthomonas) maltophilia and Burkholderia (Pseudomonas) cepacia. J Hosp Infect 1995; 30 Suppl.: 453–64
Pleasants RA, Walker TR, Samuelson WM. Allergic reactions to parenteral beta-lactam antibiotics in patients with cystic fibrosis. Chest 1994; 106: 1124–8
Thickett KM, Wildman MJ, Fegan CD, et al. Haemolytic anaemia following treatment with piperacillin in a patient with cystic fibrosis. J Antimicrob Chemother 1999; 43: 435–6
Campbell IA, Jenkins J, Prescott RJ. Intermittent ciprofloxacin in adults with cystic fibrosis and chronic Pseudomonas pulmonary infection. Med Sci Res 1989; 17(19): 797–8
Hoogkamp-Korstanje JAA. In-vitro activities of ciprofloxacin, levofloxacin, lomefloxacin, ofloxacin, perfloxacin, sparfloxacin and trovafloxacin against Gram-positive and Gram-negative pathogens from respiratory tract infections. J Antimicrob Chemother 1997; 40: 427–31
Cunningham R. Humphreys H. Once-daily gentamicin: translating theory into practice. EurJ Clin Pharmacol 1996; 50: 151–4
Mulherin D, Fahy J, Grant W, et al. Aminoglycoside induced ototoxicity in patients with cystic fibrosis. Ir J Med Sci 1991; 160(6): 173–5
Begg EJ, Barclay ML. Aminoglycosides-50 years on. Br J Clin Pharmacol 1995; 39(8): 597–603
Association of the British Pharmaceutical Industry (ABPI). Compendium of data sheets and summaries of product characteristics 1999–2000. 3rd edition. London: Datapharm Publications Limited, 1999
Bouza E, Garcia-Garrote F, Cercenado E, et al. Pseudomonas aeruginosa: a survey of resistance in 136 hospitals in Spain: the Spanish Pseudomonas aeruginosa Study group. Antimicrob Agents Chemother 1999; 43(4): 981–2
Bonfiglio G, Carciotto V, Russo G, et al. Antibiotic resistance in Pseudomonas aeruginosa: an Italian survey. J Antimicrob Chemother 1998; 41(2): 307–10
Simmonds EJ, Conway SP, Ghoneim ATM, et al. Pseudomonas cepacia: a new pathogen in patients with cystic fibrosis referred to a large centre in the United Kingdom. Arch Dis Child 1990; 65: 874–7
Isles A, Maclusky I, Corey M, et al. Pseudomonas cepacia infection in cystic fibrosis: an emerging problem. J Pediatr 1984; 104: 206–10
Weiss K, Lapointe JR. Routine susceptibility testing of four antibiotic combinations for improvement of laboratory guide to therapy of cystic fibrosis infections caused by Pseudomonas aeruginosa. Antimicrob Agents Chemother 1995; 39(11): 2411–14
Bosso JA, Saxon BA, Matsen JM. In vitro activity of aztreonam combined with tobramycin and gentamicin against clinical isolates of Pseudomonas aeruginosa and Pseudomonas cepacia from patients with cystic fibrosis. Antimicrob Agents Chemother 1987; 31(9): 1403–5
Pederen SS, Koch C, Hoiby N, et al. An epidemic spread of multiresistant Pseudomonas aeruginosa in a cystic fibrosis centre. J Antimicrob Chemother 1986; 17(4): 505–16
Cheng K, Smyth RL, Govan JR, et al. Spread of beta-lactam-resistant Pseudomonas aeruginosa in a cystic fibrosis clinic. Lancet 1996; 348: 632–42
Taylor RF, Hodson ME. Cystic fibrosis: antibiotic prescribing practices in the United Kingdom and Eire. Respir Med 1993; 87: 535–9
Smith AL, Doershuk C, Goldmann D, et al. Comparison of beta-lactam alone versus beta-lactam and an aminoglycoside for pulmonary exacerbation in cystic fibrosis. JPaediatr 1999; 134(4): 413–21
Vic P, Ategbo S, Turck D, et al. Efficacy, tolerance, and pharmacokinetics of once daily tobramycin for pseudomonas exacerbations in cystic fibrosis. Arch Dis Child 1998; 78(6): 536–9
Smith DL, Stableforth DL, Geddes AM. Evaluation of a once-daily netilmicin regimen in the treatment of cystic fibrosis. J Antimicrob Chemother 1994; 33(1): 191–3
The International Antimicrobial Therapy Cooperative Group of the European Organization for Research and Treatment of Cancer. Efficacy and toxicity of single daily doses of amikacin and ceftriaxone for infection in patients with cancer and granulocytopenia. Ann Intern Med 1993; 119: 584–93
Andrews R, Fasoli R, Scoggins WG, et al. Combined aztreonam and gentamicin therapy for pseudomonal lower respiratory tract infections. Clin Ther 1994; 16(2): 236–52
Conway SP, Pond MN, Watson A, et al. Intravenous colistin sulphomethate in acute respiratory exacerbations in adult patients with cystic fibrosis. Thorax 1997; 52(11): 987–93
Ledson MJ, Gallagher MJ, Cowperthwaite C, et al. Four years’ experience of intravenous colomycin in an adult cystic fibrosis unit. Eur Respir J 1998; 12: 592–4
Bonacori S, Fitoussi F, Lhopital S, et al. Comparative in vitro activities of meropenem, imipenem, temocillin, piperacillin, and ceftazidime in combination with tobramycin, rifampicin, or ciprofloxacin against Burkholderia cepacia isolates from patients with cystic fibrosis. Antimicrob Agents Chemother 1999; 43(2): 213–17
Lu DC, Chang SC, Chen YC, et al. In vitro activities of antimicrobial agents, alone and in combinations, against Burkholderia cepacia isolated form blood. Diagn Microbiol Infect Dis 1997; 28(4): 187–91
Szaff M, Høiby N, Flensborg EW. Frequent antibiotic therapy improves survival of cystic fibrosis patients with chronic Pseudomonas aeruginosa infection. Acta Paediatr 1983; 72(5): 651–7
Strandvik B. Adverse reactions to pipericillin in patients with cystic fibrosis [letter]. Lancet 1984; I: 1362
Moss RB. Sensitisation to aztreonam and cross-reactivity with other beta-lactam antibiotics in high risk patients with cystic fibrosis. J Allergy Clin Immunol 1991; 87: 78–88
Battersby NC, Patel L, David TJ. Increasing dose regimen in children with reactions to ceftazidime. Clin Exp Allergy 1995; 25: 1211–17
Wolter JM, Bowler SD, Nolan PJ, et al. Home intravenous therapy in cystic fibrosis: a prospective randomised trial examining clinical, quality of life and cost aspects. Eur Respir J 1997; 10(4): 896–900
Pond MN, Newport M, Joanes D, et al. Home versus hospital intravenous antibiotic therapy in the treatment of young adults with cystic fibrosis. Eur Respir J 1994; 7(9): 1640–4
Touw DJ, Brimicombe RW, Hodson ME, et al. Inhalation of antibiotics in cystic fibrosis. Eur Respir J 1995; 8: 1594–604
Webb AK, Dodd ME. Nebulised antibiotics for adults with cystic fibrosis. Thorax 1997; 52 Suppl. 2: S69–71
Ramsey BW, Pepe MS, Quan JM, et al. Intermittent administration of inhaled tobramycin in patients with cystic fibrosis. N Engl J Med 1999; 340(1): 23–30
Nikander K. Adaptive aerosol delivery: the principles. Eur Resp Rev 1997 (7); 51: 385–7
Denyer J. Adaptive aerosol delivery in practice. Eur Resp Rev 1997 (7); 51: 388–91
Currie DC. Nebulisers for bronchiectasis. Thorax 1997; 52 Suppl. 2: S72–4
Valerius NH. Koch C, Høiby N. Prevention of chronic Pseudomonas aeruginosa colonisation in cystic fibrosis by early treatment. Lancet 1991; 338: 725–6
Frederiksen B, Koch C, Høiby N. Antibiotic treatment of initial colonization with Pseudomonas aeruginosa postpones chronic infection and prevents deterioration of pulmonary function in cystic fibrosis. Pediatr Pulmonol 1997; 23: 330–5
Frederiken B, Koch C, Høiby N. Changing epidemiology of Pseudomonas aeruginosa infection in Danish cystic fibrosis patients (1974–1995). Pdiatr Pulmonol; 28 (3): 159–66
Huttner KM, Bevins CL. Antimicrobial peptides as mediators of epithelial host defense. Pediatr Res 1999; 45(6): 785–94
Brogden KA, Ackermann MR, McCray Jr PB, et al. Differences in the concentrations of small, anionic, antimicrobial peptides in bronchoalveolar lavage fluid and in respiratory epithelia of patients with and without cystic fibrosis. Infect Immun 1999; 67(8): 4256–9
Schwab U, Gilligan P, Jaynes J, et al. In vitro activities of designed antimicrobial peptides against multidrug-resistant cystic fibrosis pathogens. Antimicrob Agents Chemother 1999; 43(6): 1435–40
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Banerjee, D., Stableforth, D. The Treatment of Respiratory Pseudomonas Infection in Cystic Fibrosis. Drugs 60, 1053–1064 (2000). https://doi.org/10.2165/00003495-200060050-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200060050-00006