Summary
Nonsteroidal anti-inflammatory drugs (NSAIDs) are a group of agents with similar actions but diverse chemical structures. Aspirin (acetylsalicylic acid) and sodium salicylate were the first drugs of this type to be used clinically. However, over the past 3 decades there has been a dramatic increase in the number of NSAIDs available for the treatment of postoperative pain.
Tissue injury, such as occurs with surgical intervention, is associated with the release of numerous inflammatory mediators including prostaglandins. Prostaglandins derived from the arachidonic acid cascade are implicated in the production of inflammatory pain, and in sensitising nociceptors to the actions of other mediators. They are synthesised from arachidonic acid via the endoperoxide biosynthesis pathway, the initial step of which is catalysed by the enzyme cyclo-oxygenase. Two forms of the cyclo-oxygenase enzyme (COX-1 and COX-2) have been characterised. COX-1 is important in circumstances where prostaglandins have a protective effect such as gastric mucus production and renal blood flow maintenance. NSAIDs inhibit the synthesis of prostaglandins at 1 or more points in the endoperoxide pathway. Three mechanisms of inhibition of the biosynthetic enzymes have been proposed: (i) rapid, reversible competitive inhibition; (ii) irreversible, time-dependent inhibition; and (iii) rapid, reversible noncompetitive (free radical trapping) inhibition. In addition, there is evidence that NSAIDs have a central antinociceptive mechanism of action that augments the peripheral effect. This may involve inhibition of central nervous system prostaglandins or inhibition of excitatory amino acids or bradykinins.
There is considerable variability in the pain relief obtained from NSAIDs. Such variability in drug response may be explained in terms of differences between agents with respect to either pharmacodynamic actions or pharmacokinetic parameters or a combination of both. Stereoisomerism, where preparations exist as racemic mixtures and where only 1 enantiomer is active, may also be important. However, chiral inversion from inactive to active enantiomer may occur and may be rapid or slow.
NSAIDs have numerous adverse effects. Gastrointestinal disturbances including ulceration are the commonest adverse responses to NSAIDs and carry the greatest risk of death. Also significant are renal impairment and an increased risk of postoperative haemorrhage. Asthma and allergic reactions are uncommon.
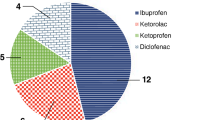
The choice of NSAID should be made on a rational basis. For short term perioperative use it is advisable to favour drugs with good safety profiles, which are available in a range of formulations. It is important to review therapy regularly, changing to an alternative NSAID if there is poor response to treatment. NSAIDs should not be used in patients with known contraindications to their use. Disparity between clinical effect and plasma concentration of some NSAIDs may be due to a complex, time-dependent concentration-effect relationship. Dosage of NSAIDs should be tailored to individual patient response, based on clinical assessment. Oral mandatory dosage regimens and intravenous (or even intramuscular) infusions may result in steady state therapeutic plasma concentrations of NSAIDs and therefore provide consistent analgesia. Finally, there seems to be little benefit from preoperative administration of NSAIDs, indeed haemorrhagic complications may be more likely.
Similar content being viewed by others
References
Vane JR, Botting RM. The mode of action of anti-inflammatory drugs. Postgrad Med J 1990; 66 Suppl. 4: S2–S17
Ferreira SH, Moncada S, Vane JR. Indomethacin and aspirin abolish prostaglandin release from spleen. Nature 1971; 231: 237–9
Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nature (New Biol) 1971; 231: 232–5
Ferreira SH. Peripheral analgesia: mechanism of the analgesic action of aspirin like drugs and opiate-antagonists. Br J Clin Pharmacol 1980; 10: 237–245S
Von Euler US. On the specific vasodilating and plain muscle stimulating substance from accessory genital glands in man and certain animals (prostaglandin and vesiglandin). J Physiol 1937; 88: 213–34
Hemler M, Lands WEM, Smith WL. Purification of the cyclooxygenase that forms prostaglandins. Demonstration of two forms of iron in the holoenzyme. J Biol Chem 1976; 251: 2629–36
Ferreira SH. Prostaglandins, aspirin-like drugs and analgesia. Nature 1972; 240: 200–3
Higgs GA, Higgs EA, Salmon JA. Prostacyclin in inflammation. In: Vane JAR, Bergstrom S, editors. Prostacyclin. New York: Raven Press, 1979: 187–92
Higgs GA, Salmon JA, Henderson B, et al. Pharmacokinetics of aspirin and salicylate in relation to inhibition of arachidonate cyclooxygenase and antiinflammatory activity. Proc Natl Acad Sci USA 1987; 84: 1417–20
Higgs GA. Arachidonic acid metabolism, pain and hyperalge- sia: the mode of action of non-steroid mild analgesics. Br J Pharmacol 1980; 10: 233–235S
Higgs GA, Moncada S, Vane JR. Prostacyclin as a potent dilator of arterioles in the hamster cheek pouch. J Physiol (Lond) 1978; 275: 30–1
Higgs EA, Moncada S, Vane JR. Inflammatory effects of prostacyclin (PGI2) and 6-oxo-PGFla in the rat paw. Prostaglandins 1978; 16: 153–62
Dray A, Bevan S. Inflammation and hyperalgesia: the team effort. Trends Pharm Sci 1993; 14: 287–90
Vane JR, Flower RJ, Botting RM. The mechanism of action of aspirin. In: Vane JR, Botting RM, editors. Aspirin and other salicylates. London: Chapman & Hall Medical, 1992
Flower R, Gryglewski R, Herbaczynska-Cedro K, et al. Effects of anti-inflammatory drugs on prostaglandin biosynthesis. Nature (New Biol) 1972; 238: 104–6
Vane JR. The mode of action of aspirin and similar compounds. J Allergy Clin Immunol 1976; 58: 691–712
Flower RJ. Drugs which inhibit prostaglandin biosynthesis. Pharmacol Rev 1974; 26: 33–67
Lands WEM. Actions of anti-inflammatory drugs. Trends Pharmacol Sci 1981; 2: 78–80
Rome LH, Lands WEM. Structural requirements for time-dependent inhibition of prostaglandin biosynthesis by anti-inflammatory drugs. Proc Nat Acad Sci USA 1975; 72: 4863–4865
Roth GJ, Majerus PW. The mechanism of the effect of aspirin on human platelets — 1: acetylation of a particulate fraction protein. J Clin Invest 1975; 56: 624–32
Roth GJ, Stanford N, Majerus PW. Acetylation of prostaglandin synthase by aspirin. Proc Natl Acad Sci USA 1975; 72: 3073–6
Kulmacz RJ, Lands WEM. Stoichometry and kinetics of the interaction of prostaglandin H synthase with anti-inflammatory agents. J Biol Chem 1985; 260: 12572–8
Appleton RA, Brown K. Conformational requirements at the prostaglandin cyclo-oxygenase receptor site: a template for designing non-steroidal anti-inflammatory drugs. Prostaglandins 1979; 18: 29–34
Hemler ME, Lands WEM. Evidence for peroxide-initiated free radical mechanism of prostaglandin biosynthesis. J Biol Chem 1980; 255: 6253–61
Lands WEM, Cook HW, Rome LH. Prostaglandin biosynthesis: consequences of oxygenase mechanisms on in vitro assays of drug effectiveness. Adv Prostaglandin Thromboxane Leukot Res 1976; 1: 7–17
Dreser H. Pharmacologisches uber Aspirin (Acetylsalicyl-saure). Pfluger’s Arch Gesamte Physiol Menschen Tiere 1899; 76: 306–18
Wiler JC, De Brouckner T, Bussel B, et al. Central analgesic effect of ketoprofen in humans — electrophysiological evidence for a supraspinal mechanism in a double-blind and cross-over study. Pain 1989; 38: 1–7
Ferreira SH, Nakamura M, de Abreu Castro MS. The hyperalgesic effects of prostacyclin and prostaglandin E2. Prostaglandins 1978; 16: 31–7
Malmbergh AB, Yaksh TL. Hyperalgesia mediated by spinal glutamate or substance receptor blocked by spinal cyclo-oxygenase inhibition. Science 1992; 257: 1276–9
Carlsson K-H, Mangel W, Jurna I. Depression by morphine and the non-opioid analgesic agents, metamizol (dipyrone), lysine acetylsalicylate, and paracetamol, of activity in rat thalamus neurones by electrical stimulation of nociceptive afferents. Pain 1988; 32: 313–26
Jurna I, Brune K. Central effect of the non-steroid anti-inflammatory agents, indometacin, ibuprofen, and diclofenac, determined in C fibre-evoked activity in single neurones of the rat thalamus. Pain 1990; 41: 71–80
Ferreira SH, Lorenzetti BB, Correa FEM. Central and peripheral antialgesic action of aspirin-like drugs. Eur J Pharmacol 1978; 53: 39–48
Hunskaar S. Similar effects of acetylsalicylic acid and morphine on immediate responses to acute noxious stimulation. Pharmacol Toxicol 1987; 60: 167–70
McCormack K, Brune K. Dissociation between the antinociceptive and anti-inflammatory effects of the non-steroidal antiinflammatory drugs. Drugs 1991; 41: 533–47
Attal N, Kayser V, Eschalier A, et al. Behavioural and electrophysiological evidence for an analgesic effect of a non-steroidal anti-inflammatory agent, diclofenac. Pain 1988; 35: 341–8
Devoghel J-C. Small intrathecal doses of lysine-acetylsalicylate relieve intractable pain in man. J Int Med Res 1983; 11: 90–1
Day RO, Brooks PM. Variations in response to non-steroidal antiinflammatory drugs. Br J Clin Pharmacol 1987; 23: 655–8
Bellamy N. Variance in NSAID studies: contribution of patient variance. Agents Actions Suppl 1985; 17: 21–8
Day RO. Variability in response to NSAID. Agents Actions Suppl 1985; 17: 15–9
Scott DL, Roden S, Marshall T, et al. Variations in response to non-steroidal anti-inflammatory drugs. Br J Clin Pharmacol 1982; 14: 691–4
Huskisson EC, Woolf DL, Balme HW, Scott J, Franklyn S. Four new anti-inflammatory drugs: responses and variations. BMJ 1976; 48: 1048–9
Gall EP, Caperton JF, McComb JE, et al. Clinical comparison of ibuprofen, fenoprofen calcium, naproxen and tolmetin sodium in rheumatoid arthritis. J Rheumatol 1982; 9: 402–7
Capell HA, Konetschnik B, Glass RC. Anti-inflammatory analgesic drug responders and non-responders: a clinico-pharmacological study of flurbiprofen. Br J Clin Pharmacol 1977; 15: 311–6
Baber N, Halliday LDC, Van Den Heuvel WJA, et al. Indomethacin in rheumatoid arthritis: clinical effects, pharmacokinetics, and platelet studies in responders and non-responders. Ann Rheum 1979; 13: 128–37
Orme ML’E, Baber N, Keenan L, et al. Pharmacokinetics and biochemical effects in responders and non-responders to nonsteroidal anti-inflammatory drugs. Scand J Rheumatol 1981; (Suppl. 39): 19-27
Grennan DM, Aarons L, Siddiqui M, et al. Dose-response study with ibuprofen in rheumatoid arthritis: clinical and pharmacokinetic findings. Br J Clin Pharmacol 1983; 18: 311–6
Preston SJ, Arnold MH, Beller EM, et al. Variability in response to non-steroidal anti-inflammatory analgesics: evidence from controlled clinical therapeutic trial of flurbiprofen in rheumatoid arthritis. Br J Clin Pharmacol 1988; 26: 759–64
Lee EJD, Williams K, Day R, et al. Stereoselective disposition of ibuprofen enantiomers in man. Br J Clin Pharmacol 1985; 19: 669–74
Hayball PJ, Tamblyn JG, Holden Y, et al. Stereoselective analysis of ketorolac in human plasma by high-performance liquid chromotography. Chirality 1993; 5: 31–5
Williams K, Day R, Knihinicki R, et al. The stereoselective uptake of ibuprofen enantiomers into adipose tissue. Biochem Pharmacol 1986; 35: 3403–5
Oates JA, Wood AJJ. Nonsteroidal antiinflammatory drugs — differences and similarities. N Eng J Med 1991; 24: 1716–25
Hutt AJ, Caldwell J. The metabolic chiral inversion of 2- arylpropionic acids — a novel route with pharmacological consequences. J Pharm Pharmacol 1983; 35: 693–704
Day RO, Williams KM, Graham GG, et al. Stereoselective disposition of ibuprofen enantiomers in synovial fluid. Clin Pharmacol Ther 1988; 43: 480–7
Knihinicki RD, Williams KM, Day RO. Chiral inversion of 2- arylpropionic acid non-steroidal anti-inflammatory drugs -1: in vitro studies of ibuprofen and flurbiprofen. Biochem Pharmacol 1989; 38: 4389–95
Ahn AHY, Amidon GL, Smith DE. Stereoselective systemic disposition of ibuprofen enantiomers in the dog. Pharm Res 1991; 8: 1186–90
Brocks DR, Liang WT, Jamali F. Influence of the route of administration on the pharmacokinetics of pirprofen enantiomers in the rat. Chirality 1993; 5: 61–4
Olliary J, Tod M, Nicolas P, et al. Pharmacokinetics of ibuprofen enantiomers after single and repeated doses in man. Biopharm Drug Dispos 1992; 13: 337–44
Knihinicki RD, Day RO, Williams KM. Chiral inversion of 2- arylpropionic acid non-steroidal anti-inflammatory drugs — II: racemization and hydrolysis of (R)- and (S)-ibuprofen-CoA thioesters. Biochem Pharmacol 1991; 42: 1905–11
Stock KP, Geisslinger G, Loew D, et al. S-ibuprofen versus ibuprofen-racemate: a randomized double-blind study in patients with rheumatoid arthritis. Rheumatol Int 1991; 11: 199–202
Geisslinger G, Stock KP, Loew D, et al. Variability in the stereoselective disposition of ibuprofen in patients with rheumatoid arthritis. Br J Clin Pharmacol 1993; 35: 603–7
Kehlet H, Dahl JB. Are perioperative nonsteroidal anti-inflammatory drugs ulcerogenic in the short term? Drugs 1992; 44 Suppl. 5: 38–41
Kenny GNC. Potential renal, haematological and allergic adverse effects associated with nonsteroidal anti-inflammatory drugs. Drugs 1992; 44 Suppl. 5: 31–7
Committee on Safety of Medicines and the Medicines Control Agency. Relative Safety of oral non-aspirin NSAIDs. Current Problems Pharmacovig 1994; 20 Aug: 9-11
Jahn U. Survey of toxicological investigations of azapropozone. In: Rainsford KD, editor. Azapropazone. Dordrecht: Kluwer Academic Publishers, 1989: 21–9
Which NSAID? [editorial]. Drug Ther Bull 1978; 25: 81–4
Carson JL, Strom BL, Soper KA, et al. The association of nonsteroidal antiinflammatory drugs with upper gastrointestinal tract bleeding. Arch Intern Med 1987; 147: 85–8
Aspirin and the stomach [editorial]. BMJ 1981; 282: 91–2
Soll AH, Weinstein WM, Kursta J, et al. Nonsteroidal anti-inflammatory drugs and peptic ulcer disease. Ann Intern Med 1991; 114: 307–19
Fenn GC, Robinson GC. Misoprostol — a logical therapeutic approach to gastroduodenal mucosal injury induced by nonsteroidal anti-inflammatory drugs?. J Clin Pharm Ther 1991; 16: 385–409
Tsai BS, Kessler LK, Schoenhard G, et al. Demonstration of specific E-type prostaglandin receptors using enriched preparations of canine parietal cells and [3H] misoprostol free acid. Am J Med 1987; 83 Suppl. 1A: 9–14
Roth S, Agrawal N, Mahowald M, et al. Misoprostal heals gastroduodenal injury in patients with rheumatoid arthritis receiving aspirin. Arch Intern Med 1989; 149: 775–9
Agrawal NM, Saggioro A. Treatment and prevention of NSAID induced gastroduodenal mucosal damage. J Rheumatol 1991; 18 (Suppl.): 15–8
Walan A, Bader J-P, Classen M, et al. Effect of omeprazole and ranitidine on ulcer healing and relapse rates in patients with benign gastric ulcer. N Engl J Med 1989; 320: 69–75
Lanza FL, Royer Jr GL, Nelson RS, et al. The effects of ibuprofen, indomethacin, aspirin, naproxen and placebo on the gastric mucosa of normal volunteers. Digest Dis Sci 1979; 24: 823–8
Reasbeck PG, Rice ML, Reasbeck JC. Double-blind controlled trial of indomethacin as an adjunct to narcotic analgesia after major abdominal surgery. Lancet 1982; i: 115–8
Ingham JM, Portenoy RK. Drugs in the treatment of pain: NSAIDS and opioids. Curr Opin Anaesthesiol 1993; 6: 838–44
Garcia Rodriguez LA, Jick H. Risk of upper gastrointestinal bleeding and perforation associated with individual non-steroidal anti-inflammatory drugs. Lancet 1994; 343: 769–72
Langman MJ, Weil J, Wainwright P, et al. Risks of bleeding peptic ulcer associated with individual non-steroidal anti-inflammatory drugs. Lancet 1994; 343: 1075–8
Gray DA, Langrieger N, Reschmaier J, et al. The effect of acetylsalicylic acid on renal function in the Pekin duck. Br J Pharmacol 1984; 82: 329–38
Harris K. The role of prostaglandins in the control of renal function [editorial]. Br J Anaesth 1992; 69: 233–5
O’Callaghan CA, Andrews PA, Ogg CS. Renal disease and use of topical non-steroidal anti-inflammatory drugs. BMJ 1994; 308: 110–1
Whelton A, Stout RL, Spilman PS, et al. Renal effects of ibuprofen, piroxicam and sulindac in patients with asymptomatic renal failure. Ann Intern Med 1990; 112: 568–76
Pearce CJ, Gonzales FM, Wallin JD. Renal failure and hyperkalaemia associated with ketorolac tromethamine. Arch Intern Med 1993; 153: 1000–2
Perttunen K, Kalso E, Heinonen J, et al. I.V. diclofenac in postthoracotomy pain. Br J Anaesth 1992; 68: 474–80
Smith K, Halliwell RMT, Lawrence S, et al. Acute renal failure associated with intramuscular ketorolac. Anaesth Intens Care 1993; 21: 700–3
Aitken HA, Burns JW, McArdle CS, et al. Effects of ketorolac trometamol on renal function. Br J Anaesth 1992; 68: 481–5
Doogan DP. Topical non-steroidal anti-inflammatory drugs. Lancet 1989; ii: 1270–1
Power I. Aspirin-induced asthma. Br J Anaesth 1993; 71: 619–21
Asad SI, Kemeny DM, Youlten L, et al. Effect of aspirin in ‘aspirin sensitive’ patients. BMJ 1984; 288: 745–8
Orme M. Profile of non-steroidal anti-inflammatory drugs. Prescribers J 1990; 30: 95–100
Parkhouse J, Rees-Lewis M, Skolinik M, et al. The clinical dose response to aspirin. Br J Anaesth 1968; 40: 433–41
Seymour RA, Rawlins MD. Efficacy and pharmacokinetics of aspirin in post-operative dental pain. Br J Clin Pharmacol 1982; 13: 807–10
Levy G. Clinical pharmacokinetics of salicylates: a reassessment. Br J Clin Pharmacol 1980; 10: 285–290S
Greenwald RA. Ketorolac: an innovative non-steroidal analgesic. Drugs Today 1992; 28: 41–6
McCormack K. Mathematical model for assessing risk of gastrointestinal reactions to NSAIDs. In: Rainsford KD, editor. Azopropizone. Dordrecht: Kluwer Academic Publishers, 1989: 81–93
Levy G. Kinetics of pharmacologic effects. Clin Pharmacol Ther 1967; 7: 362–72
Cass LJ, Frederik WS. A clinical evaluation of a sustained-release aspirin. Curr Ther Res 1965; 7: 683–92
Honig WJ, Van Ochten J. A multiple-dose comparison of ketorolac tromethamine with diflunisal and placebo in postmeniscectomy pain. J Clin Pharmacol 1986; 26: 700–5
Lovett PE, Stanton SL, Hennessey D, et al. Pain relief after major gynaecological surgery. Br J Nurs 1994; 3: 159–62
Owen H, Glavin RJ, Shaw NA. Ibuprofen in the management of postoperative pain. Br J Anaesth 1986; 58: 1371–5
Hodsman NBA, Burns J, Blyth A, et al. The morphine sparing effects of diclofenac sodium following abdominal surgery. Anaesthesia 1987; 42: 1005–8
Derbyshire DR, Richardson J. Voltarol (diclofenac) as a perioperative analgesic supplement. Br J Anaesth 1987; 59: 1327–8
Thind P, Sigsgaard T. The analgesic effect of indomethacin in the early postoperative following abdominal surgery. Acta Chirug Scand 1988; 154: 9–12
Pavy T, Medley C, Murphy DF. Effect of indomethacin on pain relief after thoracotomy. Br J Anaesth 1990; 65: 624–7
Engel C, Lund B, Kristensen AA, et al. Indomethacin as an analgesic after hysterectomy. Acta Anaesthesiol Scand 1989; 33: 498–501
Lindgren U, Djupso H. Diclofenac for pain after hip surgery. Acta Orthop Scand 1985; 55: 28–31
Bossi L, Galante G, Conoscente F, et al. Tratamento del dolore postoperatorio. Confronto in doppio cieco fra diclofenac e pentazocin. Minerva Anest 1984; 50: 373–8
Carlos DE. A comparative study of the efficacy of diclofenac sodium, meperidine HC1 and nalbuphine HC1 in postoperative analgesia. In: Birdwood GFB, Gantmacher JV, editors. Further experience with voltaren. Bern: Hans Huber, 1984: 73–8
Burns JW, Aitken HA, Bullingham RES, et al. Double-blind comparison of the morphine sparing effect of continuous and intermittent i.m. administration of ketorolac. Br J Anaesth 1991; 67: 235–8
Gillies GW, Kenny GN, Bullingham RE, et al. The morphine sparing effect of ketorolac tromethamine: a study of a new non-steroidal anti-inflammatory agent after abdominal surgery. Anaesthesia 1987; 42: 727–31
Harris PA, Riegelman. Influence of the route of administration on the area under the plasma concentration-time curve. J Pharm Sci 1969; 58: 71–5
Loo JCK, Riegelman S. New method for calculating the intrinsic absorption rate of drugs. J Pharm Sci 1968; 57: 918–28
Rowland M, Riegelman S. Pharmacokinetics of acetylsalicylic acid and salicylic acid after intravenous administration in man. J Pharmaceut Sci 1968; 57: 1313–9
Miralies FS, Carceles MD, Nicol JA, et al. Administration of lysine acetylsalicylate and pethidine in acute postoperative pain. Rev Esp Anestiol Reanim 1992; 39: 149–54
Cashman JN, Jones RM, Foster JMG, et al. Comparison of infusions of morphine and lysine acetyl salicylate for the relief of pain after surgery. Br J Anaesth 1984; 57: 255–8
Jones RM, Cashman JN, Foster JMG, et al. Comparisons of infusions of morphine and lysine acetyl salicylate for the relief of pain following thoracic surgery. Br J Anaesth 1984; 57: 259–63
Mattila MK, Ahlstrom-Bengs E, Pekkola P. Intravenous indomethacin in prevention of post-operative pain. BMJ 1993; 287: 1026
Campbell WI, Kendrick R, Patterson C. Intravenous diclofenac sodium. Anaesthesia 1990; 45: 763–6
Hovorka J, Kallela H, Kortilla K. Effect of intravenous diclofenac on pain and recovery profile after day-case laparoscopy. Eur J Anaesthiol 1993; 10: 105–8
Laitinan J, Nuutinen L, Kiiskial E-L, et al. Comparison of intravenous diclofenac, indomethecin and oxycodone as postoperative analgesics in patients undergoing knee surgery. Eur J Anaesthiol 1992; 9: 29–34
Murphy DF, Medley C. Preoperative indomethacin for pain relief after thoracotomy: comparison with postoperative indomethacin. Br J Anaesth 1993; 70: 298–300
Kavanagh BP, Katz J, Sandier AN, et al. Multimodal analgesia before thoracic surgery does not reduce postoperative pain. Br J Anaesth 1994; 73: 184–9
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Cashman, J., McAnulty, G. Nonsteroidal Anti-Inflammatory Drugs in Perisurgical Pain Management. Drugs 49, 51–70 (1995). https://doi.org/10.2165/00003495-199549010-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199549010-00005