Summary
Synopsis
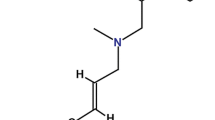
Miconazole 1 is an imidazole antifungal drug which has recently become available for systemic use. Its antifungal activity has been well studied and it is active in vitro against a wide range of fungi. Published and unpublished reports of the use of miconazole in conditions such as systemic or mucocutaneous candidosis, coccidioidomycosis, fungal meningitis, and paracoccidioidomycosis (which seems especially responsive) have often been encouraging, particularly in view of the serious, refractory nature of the conditions treated, but in most areas of use experience is limited. There are few effective drugs available for treating most systemic fungal infections, and if further studies confirm the encouraging results often seen to date, miconazole will be an important addition to the limited choices available for such conditions.
Antimicrobial Activity
Miconazole has useful in vitro activity against a wide range of dermatophytes (e.g. Trichophyton mentagrophytes, Epidermophyton floccosum), yeasts (e.g. Candida albicans, Pityrosporum orbiculare and pachydermatis, Cryptococcus neoformans) and actinomycetes (e.g. Streptomyces madurae, Nocardia asteroides), as well as some Gram-positive and anaerobic bacteria (e.g. Staphylococcus aureus, Streptococcus faecalis, Bacteroides fragilis). Like the closely related compound, econazole, it has no useful activity against Gram-negative rods. Candida albicans is moderately sensitive, most strains being inhibited by a miconazole concentration of 0.5 to 4µg/ml. Coccidioides immitis is also moderately sensitive. The causative organism of South American blastomycosis (Paracoccidioides brasiliensis), a serious endemic disease in parts of Central and South America, is highly sensitive in vitro, the minimum inhibitory concentration being about 0.001µg/ml.
In in vivo studies, intramuscular miconazole markedly increased the survival rate of rats with experimental systemic candidosis compared with placebo controls, and increased survival of mice infected with Coccidioides immitis. However, subcutaneous and intraperitoneal administration were ineffective in treating mice infected with Cryptococcus neoformans. ‘Higher’ oral doses (160mg/kg/day) were effective in treating cutaneous dermatophyte infections in guinea pigs, and oral doses of 1.5 to 3g daily markedly reduced colony counts in asymptomatic volunteers with C. albicans in their sputum.
The mode of antimicrobial action of miconazole may involve an effect on cell membranes or, according to more recent studies, miconazole may result in the accumulation of toxic reactive peroxide compounds within the microbial cell.
Pharmacokinetic Studies
Miconazole is only partially absorbed from the gastrointestinal tract, oral bioavailability being about 25 to 30%. After intravenous infusion of 522mg over 15 minutes in patients, peak plasma concentrations of 2 to 9µg/ml occurred, declining to 0.1 to 0.2µg/ml at 8 hours. Miconazole is widely distributed to body tissues. It readily penetrates into infected joints and into vitreous humour, but penetration into cerebrospinal fluid and sputum is variable and relatively low, CSF concentrations varying from less than 3% to about 50% of plasma concentrations. About 90% of the drug is bound to plasma proteins. The apparent volume of distribution in man is about 1400L. Miconazole is extensively metabolised, less than 1% being excreted in the urine unchanged. The elimination half-life in volunteers or patients is about 20 to 25 hours.
Neither renal impairment nor haemodialysis appear to affect the elimination of miconazole, but plasma concentrations are higher in patients with impaired renal function receiving the same dose as patients with normal renal function, due to a decreased distribution volume in renal impairment.
Clinical Use
Much of the clinical experience with miconazole has been reported in the form of individual case studies or reports of small series of patients. Methods of evaluation of treatment results, and duration of follow-up, often varied among reports or were not clearly stated. Most patients who have received miconazole to date have been seriously ill or dying, and many either did not respond to, or did not tolerate, previous treatment with amphotericin B or flucytosine. Nevertheless, further well designed studies are needed before the relative effectiveness of miconazole, as compared with other systemic antifungal drugs, can be stated with any certainty.
In patients with systemic or mucocutaneous candidosis, the overall response rates appear encouraging, about 80 to 90% of patients showing some improvement. The largest experience is in candidal septicaemia, and gastrointestinal, mucocutaneous and bronchopulmonary candidosis, with a small number of patients with genitourinary candidosis also reported in the literature.
The response rate in patients with chronic, severe coccidioidomycosis has varied somewhat between studies, 30% of a very small series of patients with severe disseminated disease responding and about 40 to 60% of patients with chronic pulmonary, skin and soft tissue, or musculoskeletal involvement. Many patients had been unsuccessfully treated with amphotericin B. The duration of follow-up was often not clear, but as with amphotericin B relapses occurred frequently after an initial response (about 25 to 50% of responders), and many patients received more than 1 treatment course of miconazole. The response rate in patients with paracoccidioidomycosis (South American blastomycosis) has been high (85 to 100%). This serious condition, endemic in some areas, may prove to be an important area of use. Encouragingly, when miconazole was administered orally* for 2 years (1.5g daily) following an adequate intravenous regimen, relapse did not occur. Indeed, oral therapy alone has been successful in some patients. However, the period of follow-up must be extended to confirm the absence of relapses.
A small number of patients with fungal meningitis, usually due to Coccidioides immitis or Cryptococcus neoformans, have been treated. All of these patients were seriously ill or moribund when miconazole therapy was begun. Although the response in some of these small series has been impressive (about 60% of patients), further well designed and reported studies are needed to expand the clinical experience. Many of these patients received intrathecal as well as intravenous treatment, but it has not been clearly shown that intrathecal administration improves the response.
Small numbers of patients with other fungal conditions, such as pulmonary or musculoskeletal cryptococcosis, North American blastomycosis, aspergillosis, histoplasmosis, Petriellidium boydii infections etc. have been treated with miconazole with varying degrees of success, but again further data are needed before clear statements about the response rates in such conditions can be made.
In the only controlled study available, oral miconazole (2g daily) was more effective than a placebo in preventing development of mycotic infections in cancer patients undergoing intensive cytotoxic drug therapy.
Side Effects
In data collated by the manufacturer from published and unpublished reports in the USA, the most frequent side effects were phlebitis (28%), pruritus, nausea (both about 20%), fever or chills, rash (both about 10%), vomiting and anaemia (6 to 7%). However, in a relatively large individual series of patients in the USA the incidence of some such reactions was higher, and hyponatraemia also occurred frequently (50%), especially in patients with meningitis. Other reversible haematological abnormalities (decreased haematocrit and thrombocytosis, leucopenia, erythrocyte aggregation on blood smears), possibly related to the carrier solution (a polyethoxylated castor oil; ‘Cremophor EL’), have also occurred. Reversible hyperlipidaemia also appears to be due to the carrier solution. Allergic reactions have occurred rarely.
Interestingly, the incidence of some adverse reactions was lower in studies conducted outside the USA, probably due to the generally lower doses used in non-USA studies or to formulation differences.
Dosage and Administration
Miconazole should be administered by intravenous infusion, each dose diluted in at least 200ml of 0.9% sodium chloride or 5% dextrose and infused over 30 to 60 minutes. The recommended daily dose, which may be given in 3 equal infusions 8-hourly, is 1.8 to 3.6g in coccidioidomycosis, 1.2 to 2.4g in cryptococcosis, 0.6 to 1.8g in candidosis and 0.2 to 1.2g in paracoccidioidomycosis. Children should receive about 20 to 40mg/kg daily, not exceeding 15mg/kg in a single infusion. An initial dose of 200mg should be given under observation in all patients. In the treatment of lower urinary tract infections, direct instillation into the bladder is necessary (200mg miconazole daily in an appropriate volume). In fungal meningitis, daily administration of the undiluted injection solution of miconazole (20mg per dose) by the various intrathecal routes is recommended by the manufacturer, in addition to intravenous therapy.
Similar content being viewed by others
References
Bagnarello, A.G.; Lewis, L.A.; McHenry, M.C.; Weinstein, A.J.; Naito, H.K.; McCullough, A.J.; Lederman, R.J. and Gavan, T.L.: Unusual serum lipoprotein abnormality induced by the vehicle of miconazole. New England Journal of Medicine 296: 497 (1977).
Balk, M.W.; Crumrine, M.H. and Fischer, G.W.: Evaluation of miconazole therapy in experimental disseminated candidiasis in laboratory rats. Antimicrobial Agents and Chemotherapy 13: 321 (1978).
Bannatyne, R.M. and Cheung, R.: Cooperative activity of miconazole and rifampin against strains of Candida albicans. Current Therapeutic Research 22: 869 (1977).
Bannatyne, R.M. and Cheung, R.: Susceptibility of Candida albicans to miconazole. Antimicrobial Agents and Chemotherapy 13: 1040 (1978).
Barr, R.J.; Fujita, W.H. and Graham, J.H.: Eruptive xanthomas associated with intravenous miconazole therapy. Archives of Dermatology 114: 1544 (1978).
Beggs, W.H. and Sarosi, G.A.: Synergistic action of miconazole and sulfamethoxazole on strains of Candida albicans. Current Therapeutic Research 21: 547 (1977).
Belda, W.; Lombardi, C.; Manini, M.P. and Renata Katz, D.: Miconazol, por via oral, no tratamento das dermatofltoses. Revista brasiliera Clinica Terapeutica 7: 309 (1978).
Blomqvist, K. and Horsmanheimo, M.: Systemic miconazole treatment of a patient with chronic granulomatous mucocutaneous candidiasis. Acta Dermatovener (Stockholm) 58: 455 (1978).
Bolaert, J.; Daneels, R.; Van Landuyt, H. and Symoens, J.: Miconazole plasma levels in healthy subjects and in patients with impaired renal function. Chemotherapy 6: 165 (1976).
Borelli, D. and Marcano, C.: Oral miconazole in the treatment of tinea. Boletin Mensual 9: 83 (1976).
Braincker, H.: Prophylactic treatment with miconazole in patients highly predisposed to fungal infection. A placebo-controlled double-blind study. Acta Medica Scandinavica 204: 123 (1978).
Brugmans, J.; van Cutsem, J.; Heykants, J.; Schuermans, V. and Thienpont, D.: Systemic antifungal potential, safety, biotransport and transformation of miconazole nitrate. European Journal of Clinical Pharmacology 5: 93 (1972).
Chick, E.W. and Dillon, M.L.: Miconazole therapy for aspergillomas. Unpublished report, on file Janssen Pharmaceutica (1979).
Daneels, R.; Demeyere, R.; Eggers, L.; Lust, P.; Van Landuyt, H. and Symoens, J.: Treatment of systemic candidosis with miconazole. Medizinische Welt 25: 428 (1974).
Davis, S.J. and Donovan, W.H.: Combined intravenous miconazole and intrathecal amphotericin B for treatment of disseminated coccidioidomycosis. Chest 76: 235 (1979).
de Nollin, S. and Borgers, M.: The ultrastructure of Candida albicans after in vitro treatment with miconazole. Sabouraudia 12: 341 (1974).
de Nollin, S. and Borgers, M.: The effects of miconazole on the ultrastructure of Candida albicans. Proceedings of the Royal Society of Medicine 70 (Suppl. 1): 9 (1977).
de Nollin, S.; Van Belle, H.; Goossens, F.; Thone, F. and Borgers, M.: Cytochemical and biochemical studies of yeasts after in vitro exposure to miconazole. Antimicrobial Agents and Chemotherapy 11: 500 (1977).
Deppermann, D. and Iwand, A.: Miconazole therapy for Candida septicaemia. Innere Medezin 3: 283 (1976).
Deresinski, S.C.; Galgiani, J.N. and Stevens, D.A.: Miconazole treatment of human coccidioidomycosis. Third International Syposium on Coccidioidomycosis, Tucson, Arizona, No. 17–19 (1976a).
Deresinski, S.C.; Galgiani, J.N. and Stevens, D.A.: Miconazole treatment of human coccidioidomycosis: Status report; in Ajello (ed) Coccidioidomycosis, Current Clinical and Diagnostic Status, pp.267–292 (Symposia Specialists, Miami 1977).
Deresinski, S.C.; Lilly, R.B.; Levine, H.B.; Galgiani, J.N. and Stevens, D.A.: Treatment of fungal meningitis with miconazole. American Review of Respiratory Disease 113: 71 (1976b).
Deresinski, S.C.; Lilly, R.B.; Levine, H.B.; Galgiani, J.N. and Stevens, D.A.: Treatment of fungal meningitis with miconazole. Archives of Internal Medicine 137: 1180 (1977).
Dixon, D.M.; Wagner, G.E.; Shadomy, S. and Shadomy, H.J.: In vitro comparison of the antifungal activities of R34,000, miconazole and amphotericin B. Chemotherapy 24: 364 (1978).
Doornbos, L.: Intravenous and intrathecal administration of miconazole to a premature baby. A case report. Unpublished report, Janssen Pharmaceutica (1976).
Earis, J.E. and Bernstein, A.A.: Mucoid impaction of the bronchi apparently responding to antifungal therapy. Chest 76: 116 (1979).
Evers, K.G. and Knoop, U.F.: Miconazole treatment of Candida sepsis in aminophenazone induced agranulocytosis. Acta Paediatrica Belgica 31: 151 (1978).
Fischer, T.J.; Klein, R.B.; Kershnar, H.E.; Borut, T.C. and Stiehm, E.R.: Miconazole in the treatment of chronic mucocutaneous candidiasis: A preliminary report Journal of Pediatrics 91: 815 (1977).
Fisher, J.F.; Duma, R.J.; Markowitz, S.M.; Shadomy, S.; Espinel-Ingroff, A. and Chew, W.H.: Therapeutic failures with miconazole. Antimicrobial Agents and Chemotherapy 13: 965 (1978).
Fransen, G. and Van Camp, K.: Renal and urinary tract Candida infections. Acta Urologica Belgica 42: 452 (1974).
Galgiani, J.N. and Stevens, D.A.: Antimicrobial susceptibility testing of yeasts: a turbidimetric technique independent of inoculum size. Antimicrobial Agents and Chemotherapy 10: 721 (1976).
Goenen, M.; Reynaert, M.; Jaumin, P.; Chalant, Ch.H. and Tremouroux, J.: A case of Candida albicans eudocarditis 3 years after an aortic valve replacement. Journal of Cardiovascular Surgery 18: 391 (1977).
Gratti, F.; Rossetti, C.; Mazebo, S. and Lontie, M.: Miconazole treatment of superficial mycoses in a tropical environment. Afrique Medical 13: 785 (1974).
Graybill, J.R. and Levine, H.B.: Successful treatment of cryptococcal meningitis with intraventricular miconazole. Archives of Internal Medicine 138: 814 (1978).
Graybill, J.R.; Mitchell, L. and Levine, H.B.: Treatment of experimental murine cryptococcosis: a comparison of miconazole and amphotericin B. Antimicrobial Agents and Chemotherapy 13: 277 (1978).
Grendahl, J.G. and Sung, J.P.: Synergistic action of miconazole and Atromid-S on Candida albicans. Military Medicine 144: 474 (1979).
Haller, I. and Plempel, M.: Experimental in vitro and in vivo comparison of modern antimycotics. Current Medical Research and Opinion 5: 315 (1978).
Halpern, A.A.; Nagel, D.A. and Schurman, D.J.: Allescheria boydii osteomyelitis following multiple steroid injections and surgery. Clinical Orthopedics and Related Research, No. 126, p.232 (1977).
Hatala, M.: Miconazole in systemic candidosis. Proceedings of the Royal Society of Medicine 70 (Suppl. 1): 20 (1977).
Hatala, M.; Modr, Z. and Kejda, J.: Miconazole treatment in systemic candidosis. 12th International Congress of Microbiology, September 3–8, Munchen (1978).
Heseltine, P.N.R.; Meyer, R.D.; Klein, R.A.; Busch, D.F.; Nesbitt, N. and Finegold, S.M.: Progression of disseminated coccidioidomycosis during miconazole therapy; in Ajello (ed) Coccidioidomycosis, Current Clinical and Diagnostic Status, pp.311–318 (Symposia Specialists, Miami 1977).
Hoeprich, P.D. and Goldstein, E.: Miconazole therapy for coccidioidomycosis. Journal of the American Medical Association 230: 1153 (1974).
Holt, R.J. and Azmi, A.: Miconazole-resistant candida. Lancet 1: 226 (1978).
Huijgens, P.C.; Boeijinga, J.K. and van der Meer, J.: Side effects of drugs. Possible cardiotoxic reaction to miconazole injection. Nederlandsch Tijdschrift voor Geneeskunde 119: 1549 (1975).
Ito, C.; Shibutani, Y.; Sugawara, T.; Axaoka, T.; Nakano, K.; Ohnishi, H. and Kawaoi, A.: Toxicological studies of miconazole (I). Acute and subacute toxicity studies of miconazole in mice and rats. Iyakuhin Kenkyu 7: 353 (1976a).
Ito, C.; Hayashi, Y.; Seo, T.; Asaoka, T.; Ohnishi, H. and Kawaoi, A.: Toxicological studies of miconazole (IV). Chronic toxicity study of miconazole in rats. Iyakuhin Kenkyu 7: 504 (1976b).
Ito, C.; Hayashi, Y.; Seo, T.; Sato, S.; Ohnishi, H. and Yajima, G.: Toxicological studies of miconazole (V). Chronic toxicity study of miconazole in dogs. Iyakuhin Kenkyu 7: 518 (1978c).
Ito, C.; Shibutani, Y.; Inoue, K.; Nakana, K. and Ohnishi, H.: Toxicological studies of miconazole (II). Teratological studies of miconazole in rats. Iyakuhin Kenkyu 7: 367 (1976d).
Ito, C.; Tsukuda, S.; Inoue, K.; Kasuya, S.; Fukuzawa, I.; Nakano, K.; Shibutani, Y. and Ohnishi, H.: Toxicological studies of miconazole (VI). Effects of miconazole on reproduction in rats. Iyakuhin Kenkyu 7: 535 (1976e).
Ito, C.; Shibutani, Y.; Taya, K. and Ohnishi, H.: Toxicological studies of miconazole (III). Teratological studies of miconazole in rabbits. Iyakuhin Kenkyu 7: 377 (1976f).
Iwand, A. and Depperman, D.: Miconazole in systemic mycosis. Proceedings of the Royal Society of Medicine 70 (Suppl. 1): 43 (1977).
Jones, H.E.: Miconazole in the treatment of chronic mucocutaneous candidosis and other fungal infections. Unpublished report, Janssen Pharmaceutica (1977).
Katz, M.E. and Cassileth, P.A.: Disseminated candidiasis in a patient with acute leukemia. Journal of the American Medical Association 237: 1124 (1977).
Kosuzume, H.; Ishiguro, J.; Tsuchiya, T.; Kurita, M. and Ohnishi, H.: Metabolic fate of miconazole (I). Iyakuhin Kenkyu 7: 382 (1976).
Lampert, R.P.; Hutto, J.H.; Donnelly, W.H. and Shulman, S.T.: Pulmonary and cerebral mycetoma caused by Curvularia pallescens. Journal of Pediatrics 91: 603 (1977).
Lee, C. and Maderazo, E.G.: Interference of granulocyte function by the vehicle of miconazole. Antimicrobial Agents and Chemotherapy 13: 548 (1978).
Levine, H.B.: R34000, a dioxolane imidazole in the therapy for experimental coccidioidomycosis. Comparison with miconazole and econazole. Chest 70: 755 (1976).
Levine, H.B.; Stevens, D.A.; Cobb, J.M. and Gebhart, A.E.: Miconazole in coccidioidomycosis. I. Assays of activity in mice and in vitro. Journal of Infectious Diseases 132: 407 (1975).
Lewi, P.J.; Boelaert, J.; Daneels, R.; De Meyere, R.; Van Landuyt, H.; Heykants, J.J.P.; Symoens, J. and Wynants, J.: Pharmacokinetic profile of intravenous miconazole in man. Comparison of normal subjects and patients with renal insufficiency. European Journal of Clinical Pharmacology 10: 49 (1976).
Lima, N.S.; Teixeira, G.A. and Miranda, J.L.: Treatment of South American Blastomycosis with oral miconazole. Satisfactory results in 5 cases. Anais Brasileiros de Dermatologia 49: 245 (1974).
Lima, N.S.; Teixeira, G.; Miranda, J. and do Valle, A.C.F.: Treatment of South American blastomycosis (paracoccidioidomycosis) with miconazole by the oral route: An ongoing study. Proceedings of the Royal Society of Medicine 70 (Suppl. 1): 35 (1977).
Lutwick, L.I.; Galgiani, J.N.; Johnson, R.H. and Stevens, D.A.: Visceral fungal infections due to Petriellidium boydii (Allescheria boydii). In vitro sensitivity studies. American Journal of Medicine 61: 632 (1976).
Lutwick, L.I.; Rytel, M.W.; Yanez, J.P.; Galgiani, J.N. and Stevens, D.A.: Deep infections from Petriellidium boydii treated with miconazole. Journal of the American Medical Association 241: 272 (1979).
Mader, J.T.; Ream, R.S. and Heath, P.W.: Petriellidium boydii (Allescheria boydii) sphenoidal sinusitis. Journal of the American Medical Association 239: 2368 (1978).
Marmion, L.C.; Desser, K.B.; Lilly, R.B. and Stevens, D.A.: Reversible thrombocytosis and anemia due to miconazole therapy. Antimicrobial Agents and Chemotherapy 10: 447 (1976).
Meade, R.H. and Weinstein, L.: Miconazole in the treatment of systemic fungal infections. Unpublished report, Janssen Pharmaceutica (1977).
Meyer, R.D.; Sattler, F.R.; Linne, S.R. and Ruskin, J.: Miconazole for treatment of disseminated coccidioidomycosis. Unfavourable experience. Chest 73: 825 (1978).
Michaux, J.L.; Jacquemin, P.; Cornu, G.; Wauters, G.; Gigi, J.; Noel, H.; Turine, J.B. and Ferrant, A.: Use of miconazole for prevention of opportunistic fungal infection during treatment of haematological malignancies. Proceedings of the Royal Society of Medicine 70 (Suppl. 1): 32 (1977).
Morgans, M.E.; Thomas, M.E.M. and Mackenzie, D.W.R.: Successful treatment of systemic cryptococcosis with miconazole. British Medical Journal 2: 100 (1979).
Negroni, R.; Libonatti, E.; Rubinstein, P.; Ramo, H.; Palmieri, O.; Waismann, M.; Elder, M. and Cablinsky, E.: Preliminary study of the action of miconazole on paracoccidioidomycosis. Castellania 4: 11 (1976).
Negroni, R.; Rubinstein, P.; Herrmann, A. and Gimenez, A.: Results of miconazole therapy in twenty-eight patients with paracoccidioidomycosis (South American blastomycosis). Proceedings of the Royal Society of Medicine 70 (Suppl. 1): 24 (1977).
Niell, H.B.: Miconazole carrier solution, hyperlipidaemia and hematologic problems. New England Journal of Medicine 296: 1479 (1977).
Quie, P. and Peterson, B.: Intravenous miconazole in the treatment of six patients with systemic candidosis, and of one patient with cryptococcosis. Unpublished report, Janssen Pharmaceutica (1977).
Rifkind, D.; Petersen, E.A. and Friedman, B.: Intravenous miconazole in the treatment of systemic fungus infections. Unpublished report, Janssen Pharmaceutica (1977).
Roca, G.A.: Treatment of viscero-cutaneous moniliasis with oral miconazole. Investigacion Medica Internacional 3: 302 (1976).
Rohwedder, J.J. and Archer, G.: Pulmonary sporotrichosis: Treatment with miconazole. American Review of Respiratory Disease 114: 403 (1976).
Rose, H. and Stevens, D.A.: Efficacy of I.V. miconazole in the treatment of blastomycosis. Unpublished report, on file Janssen Pharmaceutica (1978).
Rose, H.D. and Varkey, B: Miconazole treatment of relapsed pulmonary blastomycosis. American Review of Respiratory Disease 118: 403 (1978).
Rose, H.D.; Roth, D.A. and Barboriak, J.J.: Hyperlipidemia related to miconazole therapy. Annals of Internal Medicine 91: 491 (1979).
Rutgeerts, L. and Verhaegen, H.: Intravenous miconazole in the treatment of chronic oesophageal candidiasis. Gastroenterology 72: 316 (1977).
Sawyer, P.R.; Brogden, R.N.; Pinder, R.M.; Speight, T.M. and Avery, G.S.: Miconazole: A review of its antifungal activity and therapeutic efficacy. Drugs 9: 406 (1975).
Schacter, L.P.; Owellen, R.J.; Rathbun, H.K. and Buchanan, B.: Antagonism between miconazole and amphotericin B. Lancet 2: 318 (1976).
Schar, G.; Kayser, F.H. and Dupont, M.C.: Antimicrobial activity of econazole and miconazole in vitro and in experimental candidiasis and aspergillosis. Chemotherapy 22: 211 (1976).
Scheef, W.; Symoens, J.; Van Camp, K. and Daneels, R.: Chemotherapy of candidiasis. British Medical Journal 1: 78 (1974).
Shadomy, S.; Paxton, L.; Espinel-Ingroff, A. and Shadomy, H.J.: In vitro studies with miconazole and miconazole nitrate. Journal of Antimicrobial Chemotherapy 3: 147 (1977).
Stevens, D.A.: Miconazole in the treatment of systemic fungal infections. American Review of Respiratory Disease 116: 801 (1977).
Stevens, D.A.; Levine, M.B. and Deresinski, S.C.: Miconazole in coccidioidomycosis. II. Therapeutic and pharmacologic studies in man. American Journal of Medicine 60: 191 (1976).
Stevens, D.A.; Restrepo, M.; Cortes, A.; Betancourt, J.; Galgiani, J.N. and Gomez, I.: Paracoccidioidomycosis (South American blastomycosis): Treatment with miconazole. American Journal of Tropical Medicine and Hygiene 27: 801 (1978).
Stiehm, E.R.; Kershnar, H.E.; Klein, R. and Fischer, T.J.: Miconazole in the treatment of chronic mucocutaneous candidosis of childhood. Unpublished report, Janssen Pharmaceutica (1977).
Stille, W.; Helm, E. and Kilp, W.: Treatment of fungal infections with miconazole. Proceedings of the Royal Society of Medicine 70 (Suppl. 1): 40 (1977).
Sung, J.P.: Treatment of disseminated coccidioidomycosis with miconazole. Western Journal of Medicine 124: 61 (1976).
Sung, J.P. and Grendahl, J.G.: Side effects of miconazole for systemic mycoses. New England Journal of Medicine 297: 786 (1977).
Sung, J.P.; Campbell, G.D. and Grendahl, J.G.: Miconazole therapy for fungal meningitis. Archives of Neurology 35: 443 (1978).
Sung, J.P.; Grendahl, J.G. and Levine, H.B.: Intravenous and intrathecal miconazole therapy for systemic mycoses. Western Journal of Medicine 126: 5 (1977).
Sung, J.P.; Rajani, K.; Chopra, DR.; Grendahl, J.G. and Haws, E.B.: Miconazole therapy for systemic candidiasis in a conjoined (Siamese) twin and a premature newborn. American Journal of Surgery 138: in press (1979).
Svejgaard, E.: Miconazole in the treatment of candidiasis of the digestive tract. Acta Dermatovener (Stockholm) 56: 303 (1976).
Swamy, K.H.S.; Joshi, A. and Rao, G.R.: Mechanism of action of miconazole: labilization of rat liver lysosomes in vitro by miconazole. Antimicrobial Agents and Chemotherapy 9: 903 (1976a).
Swamy, K.H.S.; Sirsi, M. and Rao, G.R.: Studies on the mechanism of action of miconazole: effect of miconazole on respiration and cell permeability of Candida albicans. Antimicrobial Agents and Chemotherapy 5: 420 (1974).
Swamy, K.H.S.; Sirsi, M. and Rao, G.R.: Studies on the mechanism of action of miconazole — II. Interaction of miconazole with mammalian erythrocytes. Biochemical Pharmacology 25: 1145 (1976b).
Thong, Y.H. and Rowan-Kelly, B.: Inhibitory effect of miconazole on mitogen-induced lymphocyte proliferative responses. British Medical Journal 1: 149 (1978).
Thong, Y.H.; Rowan-Kelly, B.; Shepherd, C. and Ferrante, A.: Growth inhibition of Naegleria fowleri by tetracyclines, rifamycin and miconazole. Lancet 2: 876 (1977).
Thong, Y.H. and Ferrante, A.: In vitro susceptibility of Bacteroides fragilis to miconazole. IRCS Medical Science 6: 405 (1978).
Tytgat, G.N.; Surachno, S.; De Groot, W.P. and Schellekens, P.T.: A case of chronic oropharyngo-esophageal candidiasis with immunological deficiency: Successful treatment with miconazole. Gastroenterology 72: 536 (1977).
Vanbreuseghem, R. (Chairman): Round table discussion and chairman’s summing up. (1) Miconazole — tolerance and toxicity. Proceedings of the Royal Society of Medicine 70 (Suppl. 1): 51 (1977).
Van Cutsem, J.M. and Thienpont, D.: Miconazole, a broad-spectrum antimycotic agent with antibacterial activity. Chemotherapy 17: 392 (1972).
Van den Bossche, H.: Biochemical effects of miconazole on fungi — I. Effects on the uptake and/or utilization of purines, pyrimidines, nucleosides, amino acids and glucose by Candida albicans. Biochemical Pharmacology 23: 887 (1974).
Van den Bossche, H.; Willemsens, G.; Cools, W.; Lauwers, W.F.J. and Le Jeune, L.: Biochemical effects of miconazole on fungi. II. Inhibition of ergosterol biosynthesis in Candida albicans. Chemico-Biological Interactions 21: 59 (1978).
Verhaegen, H.: Miconazole treatment in candidal oesophagitis. Proceedings of the Royal Society of Medicine 70 (Suppl. 1): 47 (1977).
Wade, T.R.; Jones, H.E. and Chanda, J.J.: Intravenous miconazole therapy of mycotic infections. Archives of Internal Medicine 139: 784 (1979).
Wust, H.J. and Lennartz, H.: Erfolgreiche Behandlung der Hefesepsis mit Miconazol. Deutsche Medizinische Wochenschrift 99: 2515 (1974).
Wust, H.J. and Lennartz, H.: Miconazole in systemic candidiasis. Proceedings of the Royal Society of Medicine 70 (Suppl. 1): 18 (1977).
Yamaguchi, H.: Antagonistic action of lipid components of membranes from Candida albicans and various other lipids on two imidazole antimycotics, clitrimazole and miconazole. Antimicrobial Agents and Chemotherapy 12: 16 (1977).
Yamaguchi, H.: Protection by unsaturated lecithin against the imidazole antimycotics, clotrimazole and miconazole. Antimicrobial Agents and Chemotherapy 13: 423 (1978).
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: R.Y. Cartwright, Public Health Laboratory, St. Luke’s Hospital, Guildford, England; J.F. Fisher, Infectious Diseases Section, Medical College of Georgia, Augusta, Georgia, USA; J.R. Graybill, Division of Infectious Diseases, Department of Medicine, University of Texas Health Science Center at San Antonio, USA; R.J. Holt, Queen Mary’s Hospital for Children, Department of Clinical Microbiology, Carshalton, England; G. Medoff, Washington University School of Medicine, St. Louis, Missouri, USA; R.D. Meyer, Veterans Administration, Wadsworth Hospital Center, Los Angeles, USA; D.A. Stevens, Division of Infectious Diseases, Santa Clara Valley Medical Center, San Jose, California, USA; J.P. Sung, Veterans Administration Hospital, Fresno, California, USA; J.P. Utz, Georgetown University Hospital, Washington, DC, USA.
‘Monistat i.v.’ (Janssen Pharmaceutica).
Miconazole for systemic use is presently generally available only in parenteral form.
Rights and permissions
About this article
Cite this article
Heel, R.C., Brogden, R.N., Pakes, G.E. et al. Miconazole: A Preliminary Review of its Therapeutic Efficacy in Systemic Fungal Infections. Drugs 19, 7–30 (1980). https://doi.org/10.2165/00003495-198019010-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-198019010-00002