Abstract
The management of nursing home-acquired pneumonia (NHAP) continues to be debatable because of the lack of clinical trials and controversy regarding its aetiology. The controversy regarding aetiology stems, in part, from studies that utilised sputum cultures for the diagnosis of NHAP without assessing the quality of the samples. These studies found a high proportion of Gram-negative aerobic bacilli in cultures as well as Staphylococcus aureus. However, in studies that have assessed the reliability of sputum samples, Gram-negative bacilli and S. aureus were isolated infrequently and Streptococcus pneumoniae and Haemophilus influenzae isolated most commonly. Since Gram-negative aerobic bacilli and S. aureus frequently cause hospital-acquired pneumonia, some authors have considered NHAP to be a variant of this group. Many other studies, however, have considered NHAP as part of the community-acquired pneumonia category. Depending on which categorisation is used for NHAP, the treatment recommendations have varied.
There are several factors to consider in the management of NHAP in addition to choice of antibacterial: hospitalisation decision, initial route of administration of antibacterials for treatment in the nursing home, timing of switch from a parenteral to an oral agent and the duration of therapy. These factors, which have not been addressed in published guidelines, are discussed in this review. Recent guidelines recommend a fluoroquinolone (gatifloxacin, levofloxacin or moxifloxacin) or amoxicillin/clavulanic acid plus a macrolide for initial treatment of NHAP in the nursing home. For treatment in the hospital, a parenteral fluoroquinolone (as listed above) or a second- or third-generation cephalosporin plus a macrolide is recommended. A recent guideline for the treatment of healthcare-associated pneumonia (that includes NHAP) recommended an antipseudomonal cephalosporin or a carbapenem or an antipseudomonal penicillin/β-lactamase inhibitor plus ciprofloxacin plus vancomycin or linezolid for treatment of NHAP based on findings in residents with severe pneumonia who required mechanical ventilation. However, this recommendation does not apply to the majority of residents who are hospitalised with pneumonia and not intubated. Other factors to consider when choosing an empiric regimen include recent antibacterial therapy and prior colonisation with a resistant organism, e.g. methicillin-resistant S. aureus.
Recently, a group of studies by investigators in The Netherlands have focused on the concept of withholding antibacterial therapy in nursing home residents with pneumonia who have advanced dementia. These studies are reviewed in some detail because this is an approach to the management of NHAP that is uncommon but deserves more consideration given the terminal status of these people.
Future studies of NHAP should focus on development of rapid (molecular) methods to identify aetiological agents, determination of the optimum antimicrobial regimen and duration of therapy, and identification of criteria that can assist physicians and families in making the decision to withhold antimicrobial therapy in residents with advanced dementia and pneumonia.
Similar content being viewed by others
Pneumonia is the second most common infection in nursing home residents but has the highest morbidity and mortality and is one of the most common reasons for transfer to hospital.[1,2] This review specifically focuses on treatment aspects of nursing home-acquired pneumonia (NHAP), including the issue of withholding therapy for pneumonia in advanced dementia, which has not been covered in previous reviews. Information regarding the epidemiology, risk factors, pathogenesis, diagnosis and prevention of NHAP can be found in recent reviews.[1–9]
1. Classification of Nursing Home-Acquired Pneumonia (NHAP)
There does not appear to be agreement as to how to classify NHAP and this impacts on treatment recommendations. Nursing home residents with pneumonia have been included in many studies of community-acquired pneumonia (CAP). For example, Fine et al.,[10] in the development of a model to predict mortality in people with CAP admitted to hospital, included nursing home residents in the derivation and validation cohorts and found that nursing home residence was an independent predictor of mortality. Other investigators have suggested that NHAP is a distinct clinical entity and should be considered separately from CAP.[11,12] The first published guidelines for the management of CAP did not mention NHAP separately in their recommendations.[13,14] However, CAP guidelines published since 2000 have included specific recommendations for the management of NHAP and considered it a separate entity from CAP.[15–17]
In contrast, some investigators have classified NHAP as a ‘hospital-acquired’ infection, mainly on the basis of results of studies in which there was a high rate of Gram-negative aerobic bacilli isolated in sputum cultures of residents with NHAP.[18] In 2005, the American Thoracic Society (ATS) partnered with the Infectious Diseases Society of America (IDSA) and published a guideline for hospital-acquired pneumonia, ventilator-associated pneumonia and healthcare-associated pneumonia.[19] This guideline classified NHAP as a ‘healthcare-associated pneumonia’ and did not mention the recommendations for treatment of NHAP in prior guidelines published separately by each society.
There is evidence that NHAP is distinctly different from pneumonia that occurs in the community-dwelling elderly. Marrie and Blanchard[20] published a case-control study in which nursing home residents with pneumonia admitted to one hospital in Halifax, Nova Scotia, Canada were matched by age with those with pneumonia living in the community. These investigators found that mortality was significantly higher for those with NHAP (32% vs 14%). Meehan et al.[21] studied patients ≥65 years of age admitted to US hospitals with pneumonia and compared patients with CAP with those who had NHAP. Overall, CAP patients were significantly less ill and had fewer serious co-morbidities than patients with NHAP and, again, mortality was significantly higher in patients with NHAP (18.6% vs 8%). In a study in the UK, nursing home residents with pneumonia had significantly poorer functional status than elderly patients with CAP and mortality was significantly higher in the nursing home group (53% vs 13%).[22] Interestingly, in the latter study, the microbial aetiology of pneumonia was similar between the two groups (only a subset of the study population had microbiological studies done) yet the mortality was significantly higher in the nursing home group. In addition, in this study,[22] pneumonia severity as measured by the modified British Thoracic Society rule[23] or the Pneumonia Severity Index[10] was significantly worse for those with NHAP. The findings of these studies[20–23]– namely a significantly higher mortality, even when there are no differences in aetiology, as well as differences in acute severity of pneumonia — argue in favour of NHAP being distinct from pneumonia developing in community-living elderly.
In summary, variations in the classification of NHAP (community-acquired infection, a separate entity distinct from CAP, or healthcare-associated pneumonia) have resulted in different treatment recommendations, which is also due in no small part to the controversy regarding the aetiology of this infection. Because this controversy has impacted significantly on treatment recommendations it will be explored in more detail in the following section.
2. Aetiology of NHAP
Recommendations for treatment of NHAP have been influenced by the results of studies that utilised sputum cultures to make an aetiological diagnosis. Interpretation of sputum cultures in nursing home residents is confounded by the high rate of oropharyngeal colonisation by aerobic Gram-negative bacilli (including Escherichia coli, Klebsiella pneumoniae, Enterobacter species and Pseudomonas aeruginosa) and Staphylococcus aureus.[24–26] However, since microaspiration of oropharyngeal secretions is the pathogenesis for most episodes of NHAP,[27] there is a definite rationale for concern about Gram-negative bacilli and S. aureus as a cause of this infection. Nevertheless, utilising sputum cultures to identify the causative agent of NHAP is problematic for several reasons. First, sputum specimens are difficult to obtain from nursing home residents. Despite recommendations by an expert panel for obtaining sputum cultures as part of the work-up of suspected pneumonia in nursing home residents,[28] they are not usually part of the management of NHAP in clinical practice. For example, in a study of the evaluation of 94 residents with pneumonia in six nursing homes in one US city, sputum for culture was ordered in only 5%.[29] In a retrospective study, sputum specimens were obtained for culture in only 30 (19%) of 158 episodes of NHAP.[30] Secondly, to minimise the risk of culturing sputum specimens contaminated by oropharyngeal bacteria, the reliability of the specimen needs to be evaluated. Murray and Washington[31] found that the criteria that minimised the chance of contamination by oropharyngeal flora of sputum specimens was the presence of >25 polymorphonuclear leucocytes and <10 epithelial cells per 100 power microscopic field on Gram stain. However, not all studies of NHAP that have utilised results of sputum cultures to define the aetiology of this infection have evaluated sputum specimens for contamination by oropharyngeal flora. A critique of these studies is provided in the following sections.
2.1 Studies in Nonintubated Residents with Pneumonia
Muder[2] reviewed 18 studies of NHAP published between 1978 and 1994 in which the aetiology of the infection was specifically sought using sputum cultures. Studies in this review were also stratified in terms of whether or not the criteria of Murray and Washington[31] were used to determine the reliability of the specimen. Of the 18 studies reviewed, only five used the strict criteria of Murray and Washington,[31] eight used no criteria for evaluating sputum adequacy for cultures and three used other criteria developed by the investigators. In the five studies that utilised strict criteria for evaluating sputum specimens, the adequacy of the specimens for culture ranged from 22% to 42%, and the most commonly isolated organisms were Streptococcus pneumoniae (in 4–16% of cultures), Haemophilus influenzae (0–10%), Moraxella catarrhalis (0–5%), Gram-negative bacilli (0–12%) and S. aureus (1–4%).[32–36] In the remaining studies that used no criteria or modified criteria for assessing sputum adequacy, S. pneumoniae was isolated in 0–30% of cultures, H. influenzae in 0–19%, M. catarrhalis in 0–5%, Gram-negative bacilli in 3–55% and S. aureus in 0–27%.
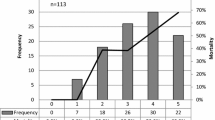
Loeb et al.[37] prospectively studied lower respiratory tract infections among residents of five nursing homes in Toronto, Ontario, Canada using standard bacterial culture methods, serology and culture for respiratory viruses (influenza, parainfluenza, respiratory syncytial virus and adenovirus), and serology for Chlamydia pneumoniae and Mycoplasma pneumoniae. In this study the investigators were able to obtain adequate sputum specimens for culture in only 24 (9%) of 272 episodes of lower respiratory tract infection; the organisms isolated were S. pneumoniae (n = 1), H. influenzae (n = 3), S. aureus (n = 3), and K. pneumoniae (n = 1). C. pneumoniae was identified in three episodes and respiratory viruses in 60 episodes. The investigators did not specifically define the aetiological agents in the 113 residents who had pneumonia. Nevertheless, these findings suggested that viruses may play a greater role in causing NHAP than previously recognised. Gauerke et al.[38] found that in 99 residents of a Veterans’ long-term care facility with pneumonia, only 14 sputum samples were found to be free of potential oropharyngeal contamination on Gram stain. Of these 14, one grew S. pneumoniae, four grew H. influenzae, one grew P. aeruginosa and eight grew only ‘normal oral flora’.
2.2 Studies in Intubated Residents with Pneumonia (‘Severe Pneumonia’)
A small group of patients (<2%) with NHAP develop acute respiratory failure requiring intubation and mechanical ventilation (so-called ‘severe pneumonia’). In a prospective study[39] of severe pneumonia in 47 nursing home residents the most common organisms isolated using invasive methods and quantitative cultures were S. aureus (29%), S. pneumoniae (9%), enteric Gram-negative bacilli (12%) and P. aeruginosa (4%). In another study[40] of 95 nursing home residents admitted to one intensive care unit, 54 (57%) had positive cultures using invasive methods and both aerobic and anaerobic cultures and 41 (43%) of study participants had no aetiological agent identified. Of the 67 organisms isolated in the 54 culture-positive patients, the most common were Gram-negative bacilli (49%), anaerobic bacteria (16%), S. aureus (12%) and S. pneumoniae (7%). The findings of these two studies[39,40] suggest that aerobic Gram-negative bacilli and S. aureus are the most common cause of severe NHAP requiring mechanical ventilation.
2.3 Summary
In nursing home residents with pneumonia who are not intubated (i.e. >95% of patients with this infection), sputum samples are infrequently obtained for culture and when they are obtained, only a minority of the samples are suitable for culture because of contamination by oropharyngeal flora. When only those sputum samples that show no evidence of contamination by oropharyngeal flora are cultured, Gram-negative bacilli and S. aureus are infrequently isolated. The most commonly isolated potential pathogens are H. influenzae and S. pneumoniae; C. pneumoniae and M. pneumoniae are rarely identified when specifically sought. In contrast, in residents with severe NHAP requiring mechanical ventilation, Gram-negative bacilli and S. aureus appear to predominate as the causative agents.
3. Pneumonia versus Pneumonitis
Nursing home residents are at considerable risk for gastric content aspiration into the lung and development of an acute inflammatory response (pneumonitis) that is initially noninfectious.[41,42] However, the factors that predispose to gastric content aspiration in nursing home residents (dysphagia, stroke, tube feeding) are the same as those that predispose to aspiration pneumonia.[9,42] In addition, the chemical inflammatory response in the lung that occurs after gastric content aspiration results in signs and symptoms identical to those of pneumonia.[42] The challenge for physicians is to distinguish between these two entities in the absence of diagnostic tests because aspiration pneumonitis in its initial stages is noninfectious and does not require antibacterial therapy.[42]
In the US, Mylotte and colleagues[43,44] have published studies in nursing home residents suggesting that clinical criteria may be useful for distinguishing between pneumonitis and pneumonia. In these studies, pneumonitis was identified more frequently than pneumonia when a careful history had been obtained to document gastric content aspiration. However, the clinical criteria for pneumonitis were associated with a misclassification rate of at least 10% in a prospective study, i.e. pneumonia was misclassified as pneumonitis.[44] Thus, these criteria cannot be recommended for general use at this time given this misclassification rate. Nevertheless, these studies suggest that there may be a substantial number of nursing home residents with a diagnosis of pneumonia who actually have pneumonitis and do not need antibacterial therapy. Of note is that in the study by El-Solh et al.[40] discussed in section 2.2, 43% of intubated residents with suspected pneumonia had negative cultures of lower respiratory tract secretions. One explanation for this finding is that some of these residents actually had gastric content aspiration and severe acute lung injury requiring mechanical ventilation or viral infection rather than bacterial infection.
4. Antibacterial Treatment
4.1 Factors to Consider Other than Selection of Antibacterials
Once the diagnosis of NHAP is suspected or established and there are no advance directives to the contrary, there are several issues to consider in addition to choosing a specific antibacterial regimen.
4.1.1 Hospitalisation Decision
Rates of hospitalisation for initial treatment of NHAP vary from 22% to 37%.[2,3,45] How physicians make the decision to hospitalise residents with pneumonia remains unclear. One study found that deterioration after regular hours or a respiratory rate >40 breaths per minute predicted transfer to hospital.[46] However, residents admitted to hospital tend to have a greater decline in functional status compared with those treated in the nursing home.[47] There is also evidence that there is no significant difference in case-fatality when NHAP is treated in the nursing home versus the hospital.[47,48] Hutt and Kramer[49] recommended hospitalisation if two or more of the following were present: oxygen saturation <90% on room air, systolic blood pressure <90mm Hg, respiratory rate >30 breaths per minute, necessity for 3L of oxygen per minute, ‘uncontrolled’ chronic lung disease, heart failure or diabetes mellitus, unarousable if previously conscious and new or increased agitation. In addition, these investigators recommended “serious consideration should be given to hospitalising [residents]” if inability to provide any one of the following applies: assessment of vital signs every 4 hours, laboratory access, parenteral hydration and two licenced nurses per shift. However, these recommendations have not been appropriately validated and, if adopted, it is likely that many more residents would be hospitalised than at the present time with no evidence of benefit.
Financial considerations may influence the decision to hospitalise residents with pneumonia. The cost of treatment of pneumonia in nursing homes in the US has been estimated to be $US485–575 per episode and this may not be fully reimbursed to the facility.[50] Since nursing homes in the US are not responsible for the cost of hospital care and may not be fully reimbursed for caring for residents with pneumonia in the facility, a facility has a financial incentive to transfer the resident to hospital for treatment. Physician availability also plays a role in that the hospitalisation decision is often made without the resident being evaluated by a physician at the bedside.[51] In this latter circumstance, family or resident preferences or pressure from facility staff may have a greater influence on the decision-making process than clinical factors.[52] The payer source for a resident also may influence the decision to hospitalise patients. For residents covered by Medicaid in the US, which utilises a prospective payment system, the extra costs incurred to manage pneumonia in the nursing home are not covered. In addition, facilities in many states receive payment while a Medicaid resident is in the hospital (bed-hold policy), which is another financial incentive for the facility to transfer residents. Medicare as a payer source and private pay residents also provide an incentive to transfer but not to as great an extent as Medicaid.[53] Facility ownership may also be a factor in the decision to transfer in the US. Konetzka et al.[53] found that residents with suspected pneumonia in not-for-profit facilities were hospitalised at half the rate of that seen in for-profit facilities.
Although the risks of hospitalisation (functional decline, emotional stress, skin breakdown) for nursing home residents clearly outweigh the benefits in many instances, family/resident preferences and financial incentives may be more important factors in the decision-making process. More studies are needed to determine which residents with pneumonia would definitely benefit from hospitalisation.
4.1.2 Initial Route of Administration (Oral versus Parenteral) of Antibacterials if Treated in the Nursing Home
In the US, parenterally administered antibacterials (usually via intramuscular injection) are prescribed for the initial treatment of NHAP in 16–44% of episodes treated in the nursing home.[2,3,45] In one study,[45] there was no significant difference in case-fatality rate between those treated with an oral versus a parenteral agent initially for NHAP in the nursing home. However, no factors could be identified that were predictive of initial parenteral therapy of NHAP in the nursing home.[45] The decision-making process whereby physicians decide to initiate treatment of NHAP with a parenteral agent in the nursing home needs to be clarified as well as the efficacy of parenteral therapy versus oral therapy.
4.1.3 Timing of Switching from Parenteral to Oral Antibacterial Therapy
It has been recommended that the timing of switching to an oral antibacterial agent from a parenteral agent in the treatment of CAP should be based on specific criteria for achieving clinical stability.[54] In a study of treatment of NHAP,[45] 75% of residents prescribed a parenteral antibacterial as initial therapy for pneumonia in the nursing home received this therapy for ≤3 days, whereas those treated in the hospital received intravenous antibacterial therapy for a median of 5 days. Based on these findings, it has been suggested that residents should be assessed for switching to an oral agent beginning on day 2 of parenteral therapy if treated in the nursing home and on day 3 if treated in hospital.[45]
4.1.4 Duration of Treatment
There are no clinical trials that assess the duration of treatment of NHAP. However, one study has provided some insight into this issue following a retrospective evaluation of treatment of NHAP in the nursing home or hospital.[45] The 75% percentile for duration of therapy was 10 days for residents treated in the nursing home, whereas if treatment was initiated in the hospital the 75th percentile for duration of treatment was 14 days. Recently, some experts have suggested that the duration of therapy for CAP need be no longer than 5 days in many cases.[55] Whether such recommendations apply to NHAP remains to be determined but it is likely that they will apply in many cases.
4.1.5 Volume Depletion
Fever and tachypnoea associated with NHAP may result in considerable insensible water loss; furthermore, oral fluid intake may be decreased secondary to delirium or decreased ability to swallow. This may result in considerable volume depletion that may not be readily appreciated clinically. Therefore, an objective assessment of the hydration status of a resident with pneumonia should be considered, for example, measuring the serum blood urea nitrogen concentration. Because intravenous administration of fluids is often not available in the nursing home setting, other methods such as clysis[56] should be considered.
4.1.6 Oxygen Supplementation
Nursing home residents with pneumonia or pneumonitis may have significant hypoxaemia that may not be readily appreciated at the bedside at times. Measurement of oxygen saturation by pulse oximetry should be carried out on all residents with pneumonia managed in the hospital or nursing home. Most residents with pneumonia or pneumonitis will require oxygen supplementation as part of the initial management. The goal of oxygen therapy should be to maintain oxygen saturation at >92% if possible.
4.2 Choosing an Antibacterial Regimen
4.2.1 Clinical Trials
There are no clinical trials for the treatment of NHAP on which to base the choice of an antibacterial regimen for this infection. The lack of trials has been a continual problem for expert panels developing treatment guidelines that include the management of NHAP. Consequently, guideline recommendations regarding antibacterial treatment of NHAP reviewed in the next two sections are based on the expertise and biases of the members of the panels responsible for the recommendations.
4.2.2 Guideline Recommendations
Antibacterial Treatment in the Nursing Home
Two guidelines provide recommendations for the treatment of NHAP in the nursing home setting and are listed in table I. The Canadian[15] and US[17] guidelines make similar recommendations for treatment. The regimens recommended are based on the assumption that S. pneumoniae and H. influenzae are the most common aetiological agents of NHAP. A fluoroquinolone (gatifloxacin, levofloxacin or moxifloxacin) may be the preferred antibacterial agent because it also has activity against all of the important ‘atypical’ pathogens and Enterobacteriaceae that may cause NHAP, it requires only one dose daily, and it is well tolerated. On the other hand, amoxicillin/clavulanic acid plus a macrolide has similar activity to a fluoroquinolone (although resistance of Enterobacteriaceae to amoxicillin/clavulanic acid is increasing and this regimen consists of two drugs given several times each day). Dosage adjustments may also be necessary when prescribing fluoroquinolones and β-lactams to the elderly because of decreased renal function.
Antibacterial Treatment in the Hospital
Guideline recommendations for empirical antimicrobial therapy of NHAP in nursing home residents admitted to hospital for initial treatment are also listed in table I. Again, the Canadian[15] and US[17] guideline recommendations are quite similar. These two guideline recommendations do not consider resistant organisms (P. aeruginosa and methicillin-resistant S. aureus) to be major aetiological agents of NHAP. In contrast, the ATS/IDSA guideline[19] assumes that nursing home residence is a major risk factor for infection caused by these resistant organisms (a view based exclusively on findings in intubated residents in an ICU setting;[39,40] see section 2.2) and, therefore, the empirical treatment recommendation focuses specifically on these pathogens. The regimen recommended by the ATS/IDSA guideline clearly is appropriate for the small percentage of cases of NHAP requiring mechanical ventilation. However, there is no evidence that this broad-spectrum regimen is more efficacious than the regimens recommended by the Canadian[15] or US[17] guidelines for residents with NHAP requiring hospitalisation who are not intubated/ventilated.
4.2.3 Factors Affecting Selection of Antibacterials
Several clinical factors, when present, may be predictive of antibacterial resistance and impact on antibacterial choice for NHAP. Vanderkooi et al.[57] prospectively studied 3339 patients with invasive pneumococcal infections in Toronto, Ontario, Canada from 1995 to 2002 and found that infection with fluoroquinolone-resistant strains was significantly associated with prior treatment with a fluoroquinolone and current residence in a nursing home. Similarly, prior treatment with co-trimoxazole (trimethoprim-sulphamethoxazole), azithromycin or clarithromycin was predictive of pneumococcal infections resistant to these agents. Therefore, when considering a fluoroquinolone, macrolide or co-trimoxazole for initial treatment of NHAP, physicians need to determine if any of these agents have been recently (within the prior 3 months) prescribed to an individual patient. A history of recent hospitalisation (in the past 3 months) or of colonisation with a resistant organism, for example, methicillin-resistant S. aureus or quinolone-resistant Gram-negative bacilli, at any body site increases the risk that this organism may be the causative agent of NHAP and needs to be considered when choosing an empirical regimen.
Recently, there has been evidence that combination antibacterial therapy may be more efficacious than single-agent therapy for CAP. Gleason et al.[58] found that the combination of a second- or third-generation cephalosporin plus a macrolide or a fluoroquinolone alone was associated with a significantly lower 30-day mortality compared with the reference regimen (non-pseudomonal third-generation cephalosporin) in the treatment of elderly patients hospitalised with CAP. Furthermore, this study included nursing home residents with pneumonia. A potential explanation for the additional benefit of the combination regimen or a fluoroquinolone alone is the immunomodulating characteristics of macrolides and fluoroquinolones.[59,60] To date, there are no clinical trials that have tested the hypothesis that a combination regimen that includes a macrolide or a fluoroquinolone alone is superior to a single agent such as a second- or third-generation cephalosporin alone in the treatment of CAP or NHAP.
4.2.4 Factors Impacting on Treatment Outcome
Two large retrospective cohort studies[21,61] of outcomes for elderly patients hospitalised with CAP have included nursing home residents in the study population. Meehan et al.[21] retrospectively reviewed the quality of care of 14 069 Medicare patients ≥65 years of age hospitalised with CAP, 23.4% of whom were nursing home residents, and found an association between time of antibacterial administration after arrival at the hospital (within 8 hours) and improved hospital survival. Houck et al.[61] performed a retrospective study of 13 711 Medicare patients (20.7% nursing home residents) hospitalised with CAP with no prehospital antibacterial treatment and found that antibacterial administration within 4 hours of arrival at the hospital was associated with significant reductions in hospital mortality (point estimate 15%) and 30-day mortality (point estimate 15%). Although nursing home residents with pneumonia were included in these studies, the applicability of the findings to that specific population is unclear at this point.
4.3 Clinical Pathway for NHAP
In a preliminary study in the US, Hutt et al.[62] found evidence that specific processes of care in the nursing home setting were associated with better outcomes in residents with pneumonia. Based on this experience, Hutt and Kramer,[49] using a modified Delphi approach, developed a guideline for the management of NHAP based on the consensus opinion of a multispecialty panel. The guideline had 25 recommendations that included criteria for the initial evaluation of residents with respiratory symptoms by nursing staff, criteria for hospitalisation, and antibacterial treatment recommendations based on published guidelines. A major focus of this guideline was the early administration of antibacterials in the nursing home whether the resident was transferred to the hospital or treated in the nursing home. There was no literature support for some of the recommendations, for example, that complete nursing assessment and physician contact should be completed within 2 hours of symptom onset, and little support for other recommendations, for example, the criteria for hospitalisation. The authors of the guideline recognised these limitations and stated that many recommendations were based primarily on ‘common sense’ and ‘expert consensus’, although they still labeled the guideline ‘evidence-based’. In a subsequent pilot study of a strategy for implementation of this guideline there was only modest improvement in compliance with guideline recommendations.[63]
The guideline proposed by Hutt and Kramer[49] is an attempt to develop standards of care for nursing home residents with pneumonia in the US that can be used to assess quality of care. Although the investigators are to be commended for their effort, the lack of evidence-based support for many of the recommendations makes the guideline less likely to be adopted. This guideline will need further revision and validation before it can be recommended for general use. In particular, it will need to be rigorously demonstrated that the guideline recommendations are true measures of quality of care and have an impact on outcome.
4.4 Withholding Antibacterial Treatment in Residents with Advanced Dementia
Infection, and, in particular, pneumonia, is a common terminal event in nursing home residents with advanced dementia.[64–66] Severity of dementia is an independent predictor of both short- (1-week; 28% mortality) and long- (3-month; 50% mortality) term mortality in NHAP after adjusting for multiple confounding factors including administration or non-administration of antibacterial therapy.[67] Given the high mortality of pneumonia in the late stages of dementia, the benefit of aggressive therapy with antibacterials, intravenous hydration and other interventions has been questioned.[68] It appears that pneumonia is often not considered to be a terminal event in those with advanced dementia and this results in aggressive treatment, including hospitalisation. Hospitalisation for treatment of pneumonia in patients with advanced dementia imposes more burdens on residents, including the need for some type of physical restraints to avoid removal of intravenous catheters, blood drawing and performing other diagnostic tests. It has been suggested that prolonging the life of someone with advanced dementia and pneumonia by administering antibacterial therapy serves only to expose the person to the continuing deterioration of his or her dementia.[69] Van der Steen et al.[70] found that care for nursing home residents with lower respiratory tract infection and dementia was more aggressive in the US than in The Netherlands regardless of the severity of dementia. In The Netherlands, antibacterial treatment was withheld in 23% of nursing home residents with pneumonia and severe dementia, and hospitalisation for treatment was rare.[71] This difference in management of NHAP in the severely demented nursing home resident reflects differences in the attitudes of physicians and families to the use of aggressive interventions in this group of people as well as the fact that in The Netherlands, unlike the US, the physician is ultimately responsible for decision-making in consultation with the family.[69] In the US, family/resident preferences take precedence in the decision to treat pneumonia and to hospitalise.
A concern in withholding antibacterial therapy for NHAP is the degree of suffering that may occur compared with when treatment is prescribed. However, van der Steen et al.[72] found that there was no difference in level of discomfort in those dying with pneumonia treated with antibacterials compared with those not receiving antibacterials. Among the residents who survived and were not treated, the level of discomfort that occurred at the onset of the pneumonia declined rapidly and returned to baseline levels within 1 week in most cases. Interestingly, although the level of discomfort in survivors treated with antibacterials tended to be lower at all time intervals, including 2 weeks prior to the onset of pneumonia, the proportionate change in level of discomfort from baseline to onset of pneumonia was the same whether or not antibacterial therapy was prescribed. Overall, it is evident from these studies that pneumonia causes significant discomfort in the demented nursing home resident whether or not antibacterials are prescribed.
When pneumonia occurs in a nursing home resident with advanced dementia, consideration needs to be given as to whether or not curative (antibacterial) therapy is appropriate. Curative treatment may lead to resolution of the pneumonia but usually there is no impact on the mental or physical status of the resident. As emphasised by van der Steen et al.,[70] optimal care of NHAP includes “prudent consideration of curative treatment, treatment to relieve discomfort, and supportive treatment in view of expected and desirable outcomes.”
5. Conclusions
The optimum management protocol for NHAP remains undetermined. The uncertainty regarding management relates to the inability to identify the aetiological agent of NHAP, a situation that is confounded by oropharyngeal colonisation by Gram-negative aerobic bacilli and S. aureus as well as a lack of clinical trials. In the US, the majority of episodes of NHAP appear to be managed in the nursing home setting and the factors that influence hospitalisation for initial treatment remain nebulous (although clinical and financial issues may be important). Currently, a fluoroquinolone (gatifloxacin, levofloxacin, or moxifloxacin) appears to be the most reasonable empirical regimen for NHAP treated in the nursing home or hospital because of its ease of administration, activity against most common aetiological agents of NHAP and excellent overall safety profile. However, there is the caveat that recent antibacterial therapy prior to pneumonia, recent hospitalisation or a history of colonisation with resistant organisms may alter that choice in some cases. For the small percentage (<2%) of cases of NHAP with severe respiratory failure that requires mechanical ventilation, Gram-negative bacilli, including P. aeruginosa and S. aureus, appear to be the most common pathogens and empirical therapy should be directed at these pathogens. Duration of therapy has not been studied for NHAP but most episodes should be successfully treated with 7 days of therapy. Future studies of NHAP should focus on applying molecular methods to identify causative agents, determining the optimum duration of therapy, distinguishing between pneumonitis and pneumonia and evaluating whether to withhold antibacterial therapy in some residents with advanced dementia and pneumonia.
References
Mylotte JM. Nursing home-acquired pneumonia. Clin Infect Dis 2002; 35: 1205–11
Muder RR. Pneumonia in residents of long-term care facilities: epidemiology, etiology, management, and prevention. Am J Med 1998; 105: 319–30
Medina-Walpole AM, Katz PR. Nursing home-acquired pneumonia. J Am Geriatr Soc 1999; 47: 1005–15
Marrie TJ. Pneumonia in the long-term care facility. Infect Control Hosp Epidemiol 2002; 23: 159–64
Loeb M. Pneumonia in older persons. Clin Infect Dis 2003; 37: 1336–9
Janssens JP, Drause KH. Pneumonia in the very old. Lancet Infect Dis 2004; 4(2): 112–24
Coleman PR. Pneumonia in the long-term care setting: etiology, management, and prevention. J Gerontol Nurs 2004; 30(4): 14–23
Furman CD, Rayner AV, Tobin EP. Pneumonia in older residents of long-term care facilities. Am Fam Phys 2004; 70(8): 1495–500
Kaikawada M, Iwamoto T, Takasaki M. Aspiration and infection in the elderly: epidemiology, diagnosis, and management. Drugs Aging 2005; 22(2): 115–30
Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997; 336: 243–50
Zimmer JG, Hall WJ. NHAP: avoiding the hospital. J Am Geriatr Soc 1997; 45: 380–1
The British Thoracic Society. Guidelines for the management of community-acquired pneumonia in adults admitted to the hospital. Br J Hosp Med 1993; 49: 346–50
Niederman MS, Bass JB, Campbell GD, et al. Guidelines for the initial management of adults with community-acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy. Am J Respir Crit Care Med 1993; 148: 1418–26
Bartlett JG, Breiman RF, Mandell LA, et al. Community-acquired pneumonia in adults: guidelines for management. Clin Infect Dis 1998; 26: 811–38
Mandell LA, Marrie TJ, Grosman RF, et al. Canadian guidelines for the initial management of community-acquired pneumonia: an evidence-based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. Clin Infect Dis 2000; 31: 383–421
Niederman MS, Mandell LA, Anzueto A, et al. Guidelines for the management of adults with community-acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med 2001; 163: 1730–54
Mandell LA, Bartlett JG, Dowell SF, et al. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis 2003; 37: 1405–33
Fein AM. Pneumonia in the elderly: overview of diagnostic and therapeutic approaches. Clin Infect Dis 1999; 28: 726–9
American Thoracic Society and Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 2005; 171: 388–416
Marrie TJ, Blanchard W. A comparison of nursing home-acquired pneumonia patients with patients with community-acquired pneumonia and nursing home patients without pneumonia. J Am Geriatr Soc 1997; 45: 50–5
Meehan TP, Fine MJ, Krumholz HM, et al. Quality of care, process, and outcomes in elderly patients with pneumonia. JAMA 1997; 278: 2080–4
Lim WS, Macfarlane JT. A prospective comparison of nursing home acquired pneumonia with community acquired pneumonia. Eur Respir J 2001; 18: 362–8
Neill AM, Martin IR, Weir R, et al. Community acquired pneumonia: aetiology and usefulness of severity criteria on admission. Thorax 1996; 51: 1010–6
Valenti WM, Trudell RG, Bentley DW. Factors predisposing to oropharyngeal colonization with Gram-negative bacilli in the aged. N Engl J Med 1978; 298: 1108–11
Nicolle LE, McLeod J, McIntyre M, et al. Significance of pharyngeal colonization with aerobic Gram-negative bacilli in elderly institutionalized men. Age Aging 1986; 15: 47–52
Muder RR, Brennen C, Wagener M, et al. Methicillin-resistant staphylococcal carriage and infection in a long-term care facility. Ann Intern Med 1991; 114: 107–12
Verghese A, Berk SL. Bacterial pneumonia in the elderly. Medicine (Baltimore) 1983; 62(5): 271–85
Bentley DW, Bradley S, High K, et al. Practice guideline for evaluation of fever and infection in long-term care facilities. Clin Infect Dis 2000; 31: 640–53
Medina-Walpole AM, McCormick WC. Provider practice patterns in nursing home-acquired pneumonia. J Am Geriatr Soc 1998; 46: 187–96
Mylotte JM, Naughton B, Saludades C, et al. Validation and application of the pneumonia prognosis index to nursing home residents with pneumonia. J Am Geriatr Soc 1998; 46: 1538–44
Murray PR, Washington JA. Microscopic and bacteriologic analysis of expectorated sputum. Mayo Clin Proc 1975; 50: 339–44
Marrie TJ, Durant H, Kwan C. Nursing home-acquired pneumonia: a case-control study. J Am Geriatr Soc 1986; 34: 697–702
Peterson PK, Stein D, Guay DRP, et al. Prospective study of lower respiratory tract infections in an extended-care nursing home program: potential role of oral ciprofloxacin. Am J Med 1988; 85: 164–71
Marrie TJ, Durant H, Yates L. Community-acquired pneumonia requiring hospitalization: 5-year prospective study. Rev Infect Dis 1989; 11: 586–99
Hirata-Dulas CAI, Stein DJ, Guay DRP, et al. A randomized study of ciprofloxacin versus ceftriaxone in the treatment of nursing home-acquired lower respiratory tract infections. J Am Geriatr Soc 1991; 39: 979–85
Drinka PJ, Gauerke C, Voeks S, et al. Pneumonia in a nursing home. J Gen Intern Med 1994; 9: 650–2
Loeb M, McGeer A, McArthur M, et al. Risk factors for pneumonia and other lower respiratory tract infections in elderly residents of long-term care facilities. Arch Intern Med 1999; 159: 2058–64
Gauerke C, Drinka P, Faulks JT, et al. Sputum bacteriology in nursing home pneumonia: a retrospective study. J Am Med Dir Assoc 2001; 2: 285–8
El-Solh AA, Sikka P, Ramadan F, et al. Etiology of severe pneumonia in the very elderly. Am J Respir Crit Care Med 2001; 163: 635–51
El-Solh AA, Pietrantoni C, Bhat A, et al. Microbiology of severe aspiration pneumonia in institutionalized elderly. Am J Respir Crit Care Med 2003; 167: 1650–4
Pick N, McDonald A, Bennett NN, et al. Pulmonary aspiration in a long-term care setting: clinical and laboratory observations and an analysis of risk factors. J Am Geriatr Soc 1996; 44: 763–8
Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med 2001; 344: 665–71
Mylotte JM, Goodnough S, Naughton BJ. Pneumonia versus pneumonitis in nursing home residents: diagnosis and management. J Am Geriatr Soc 2003; 51: 17–23
Mylotte JM, Gould M. Pneumonia versus aspiration pneumonitis in nursing home residents: prospective application of a clinical algorithm. J Am Geriatr Soc 2005; 53: 755–61
Naughton BJ, Mylotte JM. Treatment guideline for nursing home-acquired pneumonia based on community practice. J Am Geriatr Soc 2000; 48: 82–8
Fried TR, Gillick MR, Lipsitz LA. Whether to transfer? Factors associated with hospitalization and outcome of elderly longterm care patients with pneumonia. J Gen Intern Med 1995; 10: 246–50
Fried TR, Gillick MR, Lipsitz LA. Short-term functional outcomes of long-term care residents with pneumonia treated with and without hospital transfer. J Am Geriatr Soc 1997; 45: 302–6
Kruse RL, Mehr DR, Boles KE, et al. Does hospitalization impact survival after lower respiratory tract infection in nursing home residents? Med Care 2004; 42: 860–70
Hutt E, Kramer AM. Evidence-based guidelines for management of nursing home-acquired pneumonia. J Fam Pract 2002; 51: 709–16
Kruse RL, Boles KE, Mehr DR, et al. The cost of treating pneumonia in the nursing home setting. J Am Med Dir Assoc 2003; 4: 81–9
Brooks S, Harshaw G, Hasse L, et al. The physician decisionmaking process in transferring nursing home patients to the hospital. Arch Intern Med 1994; 154: 902–8
Cohen-Mansfield J, Lipson S. Medical staff’s decision-making process in the nursing home. J Gerontol A Biol Sci Med Sci 2003; 58: 271–8
Konetzka T, Spector W, Shaffer T. Effects of nursing home ownership type and resident payor source on hospitalization for suspected pneumonia. Med Care 2004; 42: 1001–8
Halm EA, Fine MJ, Marrie TJ, et al. Time to clinical stability in patients hospitalized with community-acquired pneumonia: implications for practice guidelines. JAMA 1998; 279: 1452–7
File TM, Niederman MS. Empirical therapy of community-acquired pneumonia. Infect Dis Clin North Am 2004; 18: 993–1016
Dasgupta M, Boinns MA, Rochon PA. Subcutaneous fluid infusion in a long term care setting. J Am Geriatr Soc 2000; 48: 795–9
Vanderkooi OG, Low DE, Green K, et al. Predicting antimicrobial resistance in invasive pneumococcal disease. Clin Infect Dis 2005; 40: 1288–97
Gleason PP, Meehan TP, Fine JM, et al. Associations between initial antimicrobial therapy and medical outcomes for hospitalized elderly patients with pneumonia. Arch Intern Med 1999; 159: 2562–72
Giamarellos-Bourboulis EJ, Adamis T, Laoutaris G, et al. Immunomodulatory clarithromycin treatment of experimental sepsis and acute pyelonephritis caused by multidrug-resistant Pseudomonas aeruginosa. Antimicrob Agents Chemother 2004; 48: 93–9
Choi J-H, Song M-J, Kim S-H, et al. Effect of moxifloxacin on production of proinflammatory cytokines from human peripheral blood mononuclear cells. Antimicrob Agents Chemother 2003; 47: 3704–7
Houck PM, Bratzler DW, Nsa W, et al. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med 2004; 164: 637–44
Hutt E, Frederickson EB, Ecord M, et al. Processes of care predict survival following nursing home-acquired pneumonia. J Clin Outcomes Manag 2002; 9: 249–56
Hutt E, Reznickova N, Morgenstern N, et al. Improving care for nursing home-acquired pneumonia in a managed care environment. Am J Manag Care 2004; 10: 681–6
Beard CM, Kokmen E, Sigler C, et al. Cause of death in Alzheimer’s disease. Ann Epidemiol 1996; 6: 195–200
Keene J, Hope T, Fairburn CG, et al. Death and dementia. Int J Geriatr Psychiatry 2001; 16: 969–74
Brandt HE, Deliens L, Ooms ME, et al. Symptoms, signs, problems, and diseases of terminally ill nursing home patients. Arch Intern Med 2005; 165: 314–20
van der Steen JT, Ooms ME, Mehr DR, et al. Severe dementia and adverse outcomes of nursing home-acquired pneumonia: evidence for medication by functional and pathophysiological decline. J Am Geriatr Soc 2002; 50: 439–48
Morrison RS, Siu AL. Survival in end-stage dementia following acute illness. JAMA 2000; 284: 47–52
Hertogh CMPM, Ribbe MW. Ethical aspects of medical decision-making in demented patients: a report from the Netherlands. Alzheimer Dis Assoc Disord 1996; 10: 11–9
van der Steen JT, Kruse RL, Ooms ME, et al. Treatment of nursing home residents with dementia and lower respiratory tract infection in the United States and the Netherlands: an ocean apart. J Am Geriatr Soc 2004; 52: 691–9
van der Steen JT, Ooms ME, Ader HJ, et al. Withholding antibiotic treatment in pneumonia patients with dementia. Arch Intern Med 2002; 162: 1753–60
van der Steen JT, Ooms ME, van der Wal G, et al. Pneumonia: the demented patient’s best friend? Discomfort after starting or withholding antibiotic treatment. J Am Geriatr Soc 2002; 50: 1681–8
Acknowledgements
No sources of funding were used to assist in the preparation of this review. The author has no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mylotte, J.M. Nursing Home-Acquired Pneumonia. Drugs Aging 23, 377–390 (2006). https://doi.org/10.2165/00002512-200623050-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002512-200623050-00002