Abstract
Phosphorus control remains a relevant clinical problem in dialysis patients. With age, however, serum phosphorus level decreases significantly because of a spontaneous decrease in protein intake. Older patients usually need lower doses of phosphorus binders. Nevertheless, hyperphosphataemia is observed in a quarter of patients aged >65 years.
Phosphorus retention is related to an imbalance between phosphorus intake and removal by dialysis, and is usually aggravated when vitamin D analogues are employed. Hyperphosphataemia induces secondary hyperparathyroidism and the development of osteitis fibrosa. Recent publications describe an association between phosphorus retention and increased calcium and phosphorus product (Ca2+ × P), with significant progression of tissue calcification and higher mortality risk.
Dietary intervention, phosphorus removal during dialysis and phosphorus binders are current methods for the management of hyperphosphataemia. However, the phosphorus removed by standard haemodialysis is insufficient to achieve a neutral phosphorus balance when protein intake is >50 g/day. Additional protein restriction may impose the risk of a negative protein balance. More frequent dialysis may help to control resistant hyperphosphataemia.
Phosphorus binders constitute the mainstay of serum phosphorus level control in end-stage renal disease patients. Aluminium-based phosphorus binders, associated with toxic effects, have largely been substituted by calcium-based phosphorus binders. 0However, widespread use of calcium-based phosphorus binders has evidenced the frequent appearance of hypercalcaemia and long-term progressive cardiovascular calcification. Sevelamer, a relatively new phosphorus binder, has proved efficacious in lowering serum phosphorus and parathyroid hormone (PTH) levels without inducing hypercalcaemia. Furthermore, several investigators have reported that sevelamer may prevent progression of coronary calcification. However, its efficacy in severe cases of hyperphosphataemia remains to be confirmed in large series.
There are no specific guidelines for phosphorus control in the elderly. Until more information is available, levels of mineral metabolites should be targeted in the same range as those recommended for the general population on dialysis (calcium 8.7–10.2 mg/dL, phosphorus 3.5–5.5 mg/dL and Ca2+ × P 50–55 mg2/dL2). PTH values over 120 ng/L help to avoid adynamic bone disease. Since elderly patients have a higher incidence of adynamic bone (which buffers less calcium) and vascular calcification, sevelamer should be the phosphorus binder of choice in this population; but sevelamer is costly and its long-term efficacy has not been definitively validated. Patients with low normal levels of calcium may receive calcium-based phosphorus binders with little risk. Patients with low values of PTH and high normal calcium should receive sevelamer. Tailored combinations of calcium-based phosphorus binders and sevelamer should be considered, and calcium dialysate concentration adjusted accordingly.





Similar content being viewed by others
References
US Renal Data System. USRDS 2002 annual data report. Bethesda (MD): National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2002
Krishnan M, Lok CE, Jassal SV. Epidemiology and demographic aspects of treated end-stage renal disease in the elderly. Semin Dial 2002 Apr; 15(2): 79–83
Block GA, Port FK. Re-evaluation of risks associated with hyperphosphatemia and hyperparathyroidism in dialysis patients: recommendations for a change in management. Am J Kidney Dis 2000 Jun; 35(6): 1226–37
Block GA, Hulbert-Shearon TE, Levin NW, et al. Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: a national study. Am J Kidney Dis 1998; 31: 607–17
Okechukwu CN, Lopes AA, Stack AG, et al. Impact of years of dialysis therapy on mortality risk and the characteristics of longer term dialysis survivors. Am J Kidney Dis 2002; 39: 533–8
Rufino M, García S, Alvarez A, et al. Heart valve calcifications in adult hemodialysis patients and it’s relation with CaxPO4 product, left ventricular mass and diabetes. Kidney Int 2003; 63Suppl. 85: S115–118
Goodman WG, Goldin J, Kuizon BD, et al. Coronary artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med 2000 May 18; 342(20): 1478–83
Parfitt AM, Kleerekoper M. The divalent ion homeostatic system, physiology and metabolism of calcium, phosphorus, magnesium and bone. In: Maxwell MH, Kleeman CR, editors. Clinical disorders of fluid and electrolite metabolism. New York: McGraw-Hill Book Co, 1980: 269–398
Lowrie EG, Lew NL. Death risk in hemodialysis patients: the predictive value of commonly measured variables and an evaluation of death rate differences between facilities. Am J Kidney Dis 1990; 15: 458–82
Lorenzo V, Martin M, Rufino M, et al. Protein intake, control of serum phosphorus and relatively low levels of parathyroid hormone in elderly hemodialysis patients. Am J Kidney Dis 2001; 37: 1260–6
Lorenzo V, de Bonis E, Rufino M, et al. Caloric rather than protein deficiency predominates in stable chronic hemodialysis patients. Nephrol Dial Transplant 1995; 10: 1885–9
Seidell J, Flegal K. Assessing obesity: classification and epidemiology. Br Med Bull 1997; 53: 238–52
WHO. Energy and protein requirements. Geneva: World Hearth Organization, 1985. Report of a joint FAO/WHO/UNO expert consultation. Tech Rep Ser No. 724
Toigo G, Aparicio M, Attman PO, et al. Expert working group report on nutrition in adult patients with renal insufficiency (Pt 2). Clin Nutr 2000; 19: 281–91
National Kidney Foundation. NKF-DOQI clinical practice guidelines for nutrition in chronic renal failure. Am J Kidney Dis 2000; 35Suppl. 2: S1–140
Rufino M, de Bonis E, Martin M, et al. Is it possible to control hyperphosphatemia with diet, without inducing protein malnutrition? Nephrol Dial Transplant 1998; 13Suppl. 3: 65–7
Calvo MS, Park YK. Changing phosphorus content of the US diet: potential for adverse effects on bone. J Nutr 1996 Apr; 126 (4 Suppl.): 1168–1180S
Lim VS, Flanigan MJ, Fangman J. Effect of hematocrit on solute removal during high efficiency hemodialysis. Kidney Int 1990 Jun; 37(6): 1557–62
Chauveau P, Poignet JL, Kuno T, et al. Phosphate removal rate: a comparative study of five high-flux dialysers. Nephrol Dial Transplant 1991; 6Suppl. 2: 114–5
Ramirez A, Emmett M, White M, et al. The absorption of dietary phosphorus and calcium in hemodialysis patients. Kidney Int 1986; 30: 753–9
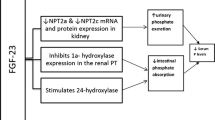
Brown AJ. Vitamin D analogues. Am J Kidney Dis 1998; 32Suppl. 2: S35–39
Rodriguez M, Almaden Y, Hernández A, et al. Effect of phosphate on the parathyroid gland: direct and indirect? Curr Opin Nephrol Hypertens 1996; 5: 321–8
Torres A, Lorenzo V, Hernández D, et al. Bone disease in predialysis, hemodialysis and CAPD patients: evidence of a better bone response to PTH. Kidney Int 1995; 47: 1434–42
Sherrard DJ, Hercz G, Pei Y, et al. The spectrum of bone disease in ESRD, an evolving disorder. Kidney Int 1993 Feb; 43(2): 436–42
Malluche H, Faugere MC. Risk of adynamic bone disease in dialyzed patients. Kidney Int 1992; 42Suppl. 38: S62–67
Fournier A, Yverneau PH, Hue P, et al. Adynamic bone disease in patients with uremia. Curr Opin Nephrol Hypertens 1996; 3: 396–410
Coco M, Rush H. Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis 2000; 36(6): 1115–21
Braun J, Oldendorf M, Moshage W, et al. Electron beam computed tomography in the evaluation of cardiac calcifications in chronic dialysis patients. Am J Kidney Dis 1996; 27: 394–401
Llach F. The evolving pattern of calciphylaxis: therapeutic considerations. Nephrol Dial Transplant 2001 Mar; 16(3): 448–51
Ahmed S, O’Neill KD, Hood AF, et al. Calciphylaxis is associated with hyperphosphatemia and increased osteopontin expression by vascular smooth muscle cells. Am J Kidney Dis 2001 Jun; 37(6): 1267–76
Narang R, Ridout D, Nonis C, et al. Serum calcium, phosphorus, and albumin levels in relation to angiographic severity of coronary artery disease. Int J Cardiol 1997; 60: 73–9
Slatopolsky E, Rutherford WE, Rosenbaum R, et al. Hyperphosphatemia. Clin Nephrol 1977; 7: 138–46
Ribeiro S, Ramos A, Brandao A, et al. Cardiac valve calcification in haemodialysis patients: role of calcium-phosphate metabolism. Nephrol Dial Transplant 1998; 13: 2037–40
Andress DL. New therapies raise new issues for lowering parathyroid hormone levels in uremic patients. Semin Dial 1999; 12: 282–4
Kates DM, Andress DL. Control of hyperphosphatemia in renal failure: role of aluminum. Semin Dial 1996; 9: 310–5
Eknoyan G, Levin A, Levin NW. Bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 2003; 42 (4 Suppl. 3): 1–201
Hou SH, Zhao J, Ellman CF, et al. Calcium and phosphate fluxes during hemodialysis with low calcium dialysate. Am J Kidney Dis 1991; 18: 217–24
Delmez JA, Slatopolsky E. Hyperphosphatemia: its consequences and treatment in patients with chronic renal disease. Am J Kidney Dis 1992; 19(4): 303–17
Buoncristiani U. Fifteen years of clinical experience with daily haemodialysis. Nephrol Dial Transplant 1998; 13Suppl. 6: 148–51
Mucsi I, Hercz G, Uldall R, et al. Control of serum phosphate without any phosphate binders in patients treated with nocturnal hemodialysis. Kidney Int 1998; 53(5): 1399–401
Sheikh MS, Maguire JA, Emmett M, et al. Reduction of dietary phosphorus absorption by phosphorus binders: a theoretical, in vitro, and in vivo study. J Clin Invest 1989; 83(1): 66–73
Hercz D, Coburn J. Prevention of phosphate retention and hyperphosphatemia in uremia. Kidney Int 1987; 32: S215–20
Slatopolsky E, Brown A, Dusso A. Role of phosphorus in the pathogenesis of secondary hyperparathyroidism. Am J Kidney Dis 2001 Jan; 37Suppl. 2: S54–57
Emmett M, Sirmon MD, Kirkpatrick WG, et al. Calcium acetate control of serum phosphorus in hemodialysis patients. Am J Kidney Dis 1991; 17: 544–50
Ring T, Nielsen C, Andersen SP, et al. Calcium acetate versus calcium carbonate as phophorus binders in patients on chronic haemodialysis. Nephrol Dial Transplant 1993; 8: 341–6
Coburn JW, Mische MG, Goodman WG, et al. Calcium citrate markedly enhances aluminium absorption from aluminum hydroxide. Am J Kidney Dis 1991; 17: 708–11
Birck R, Zimmermann E, Wassmer S, et al. Calcium ketoglutarate versus calcium acetate for treatment of hyperphosphataemia in patients on maintenance haemodialysis: a crossover study. Nephrol Dial Transplant 1999; 14: 1475–9
Bro S, Rasmussen RA, Handberg J, et al. Randomized crossover study comparing the phosphate-binding efficacy of calcium ketoglutarate versus calcium carbonate in patients on chronic hemodialysis. Am J Kidney Dis 1998; 2: 257–62
Meric F, Yap P, Bia MJ. Etiology of hypercalcemia in hemodialysis patients on calcium carbonate therapy. Am J Kidney Dis 1990; 16: 459–64
Guerin AP, London GM, Marchais SJ, et al. Arterial stiffening and vascular calcifications in end-stage renal disease. Nephrol Dial Transplant 2000 Jul; 15(7): 1014–21
Blacher J, Guerin AP, Pannier B, et al. Arterial calcifications, arterial stiffness, and cardiovascular risk in end-stage renal disease. Hypertension 2001 Oct; 38(4): 938–42
Salusky IB, Foley J, Nelson P, et al. Aluminum accumulation during treatment with aluminum hydroxide and dialysis in children and young adults with chronic renal disease. N Engl J Med 1991 Feb 21; 324(8): 527–31
Parkinson IS, Ward MK, Feest TG, et al. Fracturing dialysis osteodystrophy and dialysis encephalopathy: an epidemiological survey. Lancet 1979 Feb 24; I(8113): 406–9
Platts MM, Goode GC, Hislop JS. Composition of the domestic water supply and the incidence of fractures and encephalopathy in patients on home dialysis. BMJ 1977 Sep 10; 2(6088): 657–60
Oe PL, Lips P, van der Meulen J, et al. Long-term use of magnesium hydroxide as a phosphate binder in patients on hemodialysis. Clin Nephrol 1987; 28: 180–5
O’Donovan R, Baldwin D, Hammer M, et al. Substitution of aluminium salts by magnesium salts in control of dialysis hyperphosphataemia. Lancet 1986; I: 880–2
Delmez JA, Kelber J, Norword KY, et al. Magnesium carbonate as a phosphorus binder: a prospective, controlled, crossover study. Kidney Int 1996; 49: 163–7
Hergesell O, Ritz E. Stabilized polynuclear iron hydroxide is an efficient oral phosphate binder in uraemic patients. Nephrol Dial Transplant 1999; 14: 863–7
Weaver CM, Schulze DG, Peck LW, et al. Phosphate-binding capacity of ferrihydrite versus calcium acetate in rats. Am J Kidney Dis 1999; 34: 324–7
Spengler K, Follmann H, Boos KS, et al. Cross-linked iron dextran is an efficient oral phosphate binder in the rat. Nephrol Dial Transplant 1996; 11: 808–12
Plone MA, Petersen JS, Rosenbaum DP, et al. Sevelamer, a phosphate-binding polymer, is a non-absorbed compound. Clin Pharmacokinet 2002; 41(7): 517–23
Burke SK, Slatopolsky EA, Goldberg DI. RenaGel, a novel calcium- and aluminium-free phosphate binder, inhibits phosphate absorption in normal volunteers. Nephrol Dial Transplant 1997; 12(8): 1640–4
Slatopolsky EA, Burke SK, Dillon MA. RenaGel, a nonabsorbed calcium and aluminum free phosphate binder, lowers serum phosphorus and parathyroid hormone. Kidney Int 1999; 55: 299–307
Chertow GM, Burke SK, Lazarus JM, et al. Poly[allylamine hydrochloride] (RenaGel): a noncalcemic phosphate binder for the treatment of hyperphosphatemia in chronic renal failure. Am J Kidney Dis 1997 Jan; 29(1): 66–71
Goldberg DI, Dillon MA, Slatopolsky EA, et al. Effect of RenaGel, a non-absorbed, calcium- and aluminium-free phosphate binder, on serum phosphorus, calcium, and intact parathyroid hormone in end-stage renal disease patients. Nephrol Dial Transplant 1998 Sep; 13(9): 2303–10
Chertow G, Dillon M, Burke S, et al. A randomized trial of sevelamer hydrochloride (Renagel) with and without supplemental calcium: strategies for the control of hyperphosphataemia and hyperparathyroidism in hemodialysis patients. Clin Nephrol 1999; 51: 18–26
Chertow GM, Burke SK, Dillon MA, et al. Long-term effects of sevelamer hydrochloride on the calcium x phosphorus product and the lipid profile of hemodialysis patients. Nephrol Dial Transplant 1999; 14: 2907–14
Chertow GM, Burke SK, Raggi P. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patient. Treat to Goal Working Group. Kidney Int 2002; 62: 245–52
Bleyer AJ, Burke SK, Dillon M, et al. A comparison of the calcium free phosphate binder sevelamer hydrochloride with calcium acetate in the treatment of hyperphosphatemia in hemodialysis patients. Am J Kidney Dis 1999; 33: 694–701
Lacy C, editor. Drug information handbook. 11th ed. Hudson (OH): Lexi-Comp, Inc., 2003
Nola CH, Qunibi W. How should hyperphosphatemia be managed in dialysis patients? Seminars in Dialysis 2002; 15(5): 324–6
Mclntyre CW, Patel V, Taylor GS, et al. A prospective study of combination therapy for hyperphosphataemia with calcium-containing phosphate binders and sevelamer in hypercalcaemic haemodialysis patients. Nephrol Dial Transplant 2002 Sep; 17(9): 1643–8
Braunlin W, Zhorov E, Guo A, et al. Bile acid binding to sevelamer HC1. Kidney Int 2002 Aug; 62(2): 611–9
Graff L, Burnel D. A possible non-aluminum oral phosphate binder: a comparative study on dietary phosphorus absorption. Res Commun Mol Pathol Pharmacol 1995; 89: 373–88
Hutchinson AJ. Calcitriol, lanthanum carbonate and other phosphate binders in the management of renal osteodystrophy. Perit Dial Int 1999; 19Suppl. 2: S408–412
Joy MS, Hladik GA, Finn WF. Safety of an investigational phosphate binder (lanthanum carbonate) in hemodialysis patients [abstract]. J Am Soc Nephrol 1999; 10: A1327
Finn WF, Joy MS, Hladik GA. Results of a randomized dose-ranging, placebo controlled study of lanthanum carbonate for reduction of serum phosphate in chronic renal failure patients receiving hemodialysis [abstract]. J Am Soc Nephrol 1999; 10: A1317
Behets GJ, Dams G, Damment S, et al. An assessment of the effects of lanthanum on bone in a chronic renal failure (CRF) rat model [abstract]. American Society of Nephrology Annual Meeting; 2001 Oct 12–15; San Francisco, A3862
Joy MS, Finn WF, on behalf of the LAM-302 Study Group. Randomized, double-blind, placebo-controlled, dose-titration, phase III study assessing the efficacy and tolerability of lanthanum carbonate: a new phosphate binder for the treatment of hyperphosphatemia. Am J Kidney Dis 2003 Jul; 42(1): 96–107
Hutchison AJ. The novel, non-aluminum, non-calcium phosphate binder, lanthanum carbonate (Fosrenol™), is an effective treatment for hyperphosphataemia and has a good safety profile [abstract]. American Society of Nephrology Annual Meeting; 2002 Nov 1–4; Philadelphia
D’Haese PC, Spasovski GB, Sikole A, et al. A multicenter study on the effects of lanthanum carbonate (Fosrenol) and calcium carbonate on renal bone disease in dialysis patients. Kidney Int Suppl 2003 Jun; 85: S73–78
Lindberg JS, Moe SM, Goodman WG, et al. The calcimimetic AMG 073 reduces parathyroid hormone and calcium x phosphorus in secondary hyperparathyroidism. Kidney Int 2003 Jan; 63(1): 248–54
Acknowledgements
The authors wish to make known that they do not have any source of funding or formal association with the pharmaceutical industry.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sellares, V.L., Ramírez, A.T. Management of Hyperphosphataemia in Dialysis Patients. Drugs Aging 21, 153–165 (2004). https://doi.org/10.2165/00002512-200421030-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002512-200421030-00002