Abstract
Linezolid is an oxazolidinone, a new class of antibacterial with a unique mechanism of action, namely inhibition of the formation of a functional 70S initiation complex in the 50S bacterial ribosomal subunit. Linezolid is highly active against multidrug-resistant Gram-positive cocci, including meticillin-resistant Staphylococcus aureus (MRSA), vancomycin-intermediate and vancomycinresistant S. aureus, and vancomycin-resistant enterococci; its spectrum of activity also includes some anaerobic bacteria.
Linezolid has been studied in several randomized controlled trials for the treatment of patients with community-acquired and nosocomial pneumonia, skin and soft tissue infections (SSTIs), urinary tract infections and bacteraemia. The available evidence suggests that linezolid is at least as effective as vancomycin for patients with nosocomial pneumonia, and there are some retrospective analyses supporting its superiority in comparison with vancomycin for MRSA nosocomial pneumonia, including ventilator-associated pneumonia. Linezolid is more effective than glycopeptides, macrolides and β-lactams for SSTIs. The limited available data for the treatment of patients with bacteraemia suggest that it may be a better treatment option than vancomycin and β-lactams for these patients, but questions have arisen regarding patients with catheter-related bacteraemias.
Compared with other antibacterials, linezolid is associated with a greater frequency of adverse events, mainly nausea, vomiting, diarrhoea and headaches. Thrombocytopenia also occurs more frequently in patients taking linezolid but there is no increased frequency of anaemia. Other adverse events potentially related to linezolid therapy include fungal infections (moniliasis), hypertension and serotonin-like syndrome, tongue discolouration and taste alterations, dizziness, insomnia, rash and Clostridium difficile-related diarrhoea. The majority of adverse events develop after prolonged administration (i.e. >2 weeks) and subside shortly after discontinuation of linezolid. Peripheral or optic neuropathy, another possible adverse effect, is associated with an even longer duration of treatment (3–6 months).
In conclusion, linezolid is an important treatment option for the treatment of patients with multidrug-resistant, Gram-positive bacterial infections. However, in order to reduce the possibility of development of resistance and preserve its activity, the use of linezolid should be restricted to treatment of patients with infections associated with high morbidity and mortality, particularly those caused by multidrug-resistant bacteria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Linezolid, a drug that belongs to a new class of antibacterials called oxazolidinones, inhibits bacterial growth by binding to the bacterial 23S ribosomal RNA of the 50S subunit and blocking formation of a functional 70S initiation complex, which is essential for the bacterial translation process.[1–3] This mechanism of action is not found in any other class of antibacterials currently used for the treatment of Gram-positive infections. Therefore, it has been argued that resistance to linezolid (both cross- and de novo resistance) may be unlikely to develop.[4,5]
Linezolid is active against a variety of Grampositive cocci, including staphylococci, streptococci and enterococci[6] Multidrug-resistant strains of the aforementioned cocci (i.e. meticillin-(MRSA) and vancomycin-resistant Staphylococcus aureus (VRSA), vancomycin-resistant Enterococcus faecium and E. faecalis (VRE), and penicillin-resistant Streptococcus pneumoniae) are also susceptible to this antibacterial.[6] Linezolid is bacteriostatic against staphylococci and enterococci, and bactericidal against streptococci. It is also active against anaerobic bacteria including Clostridium perfringens, C. difficile, Peptostreptococcus spp., Bacteroides fragilis, Fusobacterium nucleatum and F. meningosepticum. Finally, it shows limited activity against Moraxella catarrhalis and Haemophilus influenzae.[6]
Linezolid is administered orally or intravenously at a dosage of 600 mg twice daily.[7] With this schedule of administration, a 24-hour area under the plasma concentration-time curve over minimal inhibitory concentration (AUC/MIC) ratio of 50 : 100 is achieved, which is usually associated with clinical effectiveness in the treatment of patients with infections due to susceptible bacteria.[8] Specifically, having achieved this pharmacodynamic goal, linezolid 600 mg twice daily in humans would be successful against organisms with MICs of up to 2–4 μg/mL.[8] Linezolid is 100% bioavailable after oral administration, and the times to peak plasma concentration are 1 and 2 hours after single- and multiple-dose administration, respectively.[9,10] Linezolid exhibits good penetration in the lungs,[11] skin,[12] muscles,[13] cerebrospinal fluid[14] and bones.[15] Its plasma protein binding is approximately 31 % (which is concentration independent).[16] Its half-life is 5.5 hours[17] and it is eliminated through the kidneys and gastrointestinal tract either as the administered form or as metabolites.[18,19]
Linezolid was released to the market in 2000. Its primary indications include treatment of patients with complicated and uncomplicated skin and soft tissue infections (SSTIs), community-acquired pneumonia (CAP) and nosocomial pneumonia, and infections caused by VRE.[7] Linezolid has also been used to treat other infections caused by Gram-positive cocci, including endocarditis, urinary tract infections, bacteraemia, infections of the CNS, osteomyelitis, infections in neutropenic patients, and tuberculosis caused by multidrug-resistant mycobacteria.
Linezolid is one of the newly available antibacterials that were added to those used traditionally for the treatment of serious Gram-positive infections, i.e. vancomycin and teicoplanin for multidrug-resistant Gram-positive cocci, and broad-spectrum β-lactams, cotrimoxazole (trimethoprim/sulfamethoxazole), clindamycin, aminoglycosides or fluoroquinolones for susceptible micro-organisms. Other new treatment options approved for such infections include quinupristin/dalfopristin, tigecycline and daptomycin, while telavancin, dalbavancin and ceftobiprole have also shown promising results.
1. Benefit Assessment: Comparison with Alternative Treatment Options
1.1 Overview of the Available Evidence from Randomized Controlled Trials
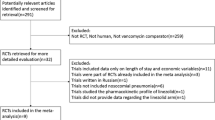
Several randomized controlled trials (RCTs) have been conducted thus far comparing linezolid with another antibacterial for the treatment of patients with Gram-positive infections (table I);[20–38] in an additional RCT, two different doses of linezolid were compared.[39] The majority of these RCTs enrolled patients with different types of infections, including SSTIs, pneumonia (both CAP and hospital-acquired pneumonia), urinary tract infections and bacteraemia.
A meta-analysis of 12 RCTs[23–26,28–34,38] involving 6093 patients has been reported.[40] This metaanalysis found that all-cause mortality was similar between patients receiving linezolid and comparator antibacterials (glycopeptides and β-lactams) [odds ratio (OR) 0.97; 95% CI 0.79,1.19]. Linezolid treatment resulted in resolution or improvement of symptoms of infection in 86.3% of patients, compared with 81.9% of patients treated with comparator antibacterials. Overall, linezolid was more effective in this respect than comparator antibacterials for the treatment of patients with Gram-positive infections in both intention-to-treat (ITT) [OR = 1.23; 95% CI 1.06, 1.42] and clinically evaluable (OR = 1.41; 95% CI 1.11, 1.81) populations. When data from blinded RCTs only were pooled, linezolid was not more effective than the comparator antibacterials (OR =1.14; 95% CI 0.95, 1.38). Conversely, when data from non-blinded RCTs only were pooled, linezolid was more effective than the comparators (OR = 1.35; 95% CI 1.08, 1.68). Linezolid was more effective than glycopeptides (OR = 1.51; 95% 1.03, 2.22) for all infections combined but not more effective than vancomycin (OR = 1.44; 95% CI 0.90, 2.30) or β-lactams (OR = 1.34; 95% CI 0.99, 1.81).[40]
Sub-analyses were conducted according to the site of infection. In patients with SSTIs, linezolid treatment resolved or improved symptoms of infection in 90.3% of patients, while treatment with glycopeptides and β-lactams was successful in 85.7% of patients.[40] Linezolid was more effective in this respect than all comparator antibacterials (OR = 1.67; 95% CI 1.31,2.53), glycopeptides (OR = 2.24; 95% CI 1.12, 4.48) and β-lactams (OR = 1.37; 95% CI 1.00, 1.88). In patients with bacteraemia, linezolid was successful in 81.3% of patients in contrast to 66.4% treated with comparator antibacterials (OR = 2.07; 95% CI 1.13, 3.78). It should be noted that the majority of these bacteraemias were secondary to other infections. Finally, in patients with pneumonia due to Gram-positive infections, linezolid was as effective as comparator antibacterials (74.9% vs 74.8%, respectively; OR = 1.03; 95% CI 0.75, 1.42). There was also no difference between antibacterials when only patients with nosocomial pneumonia were analysed (OR = 1.05; 95% CI 0.75, 1.46). Because of a lack of available data, no further analysis was performed regarding patients with ventilator-associated pneumonia).[40]
In the microbiologically evaluable population, linezolid was associated with better resolution or improvement of symptoms than all comparator antibacterials combined (OR = 1.34; 95% CI 1.05, 1.72), glycopeptides (OR = 1.49; 95% CI 1.11,1.99) and vancomycin alone (OR = 1.41; 95% CI 1.01, 1.98); however, there was no difference in this respect between linezolid and β-lactams (OR = 1.06; 95% CI 0.67, 1.68).[40] In addition, linezolid was associated with higher eradication rates for S. aureus than all comparator antibacterials (OR = 1.81; 95% CI 1.40, 2.34) and glycopeptides (OR = 2.08; 95% CI 1.51, 2.86), but was not associated with higher eradication rates for MRSA (OR = 1.69; 95% CI 0.84, 3.41) or MRSA strains isolated from patients with nosocomial pneumonia (OR = 1.26; 95% CI 0.54, 2.96). Finally, there was no difference in eradication of enterococcal species (OR = 0.95; 95% CI 0.33, 2.73) or streptococcal species (OR = 0.97; 95% CI 0.55, 1.72).[40]
Although meta-analyses are useful for synthesizing results of different studies, they also have limitations, such as the lack of individual patient data or the lack of extractable disaggregated data, which should always be taken into account. Therefore, several issues that have been raised in individual RCTs or post hoc analyses of them, which were designed to compare the effectiveness of linezolid with that of other antibacterials for the treatment of patients with Gram-positive infections, are discussed in the following sections.
1.2 Community-Acquired Pneumonia
Although linezolid is not highly active against all causative pathogens of CAP, such as atypical pathogens, which are responsible for approximately 30% of pneumonia cases,[41] and H. influenzae,[6] it has been compared with ceftriaxone (1 g twice daily) followed by cefpodoxime (200 mg twice daily) for the treatment of patients with CAP who required hospitalization in an open-label RCT that enrolled 747 patients.[35] S. pneumoniae was the predominantly isolated pathogen (73% of patients), followed by S. aureus (22%), H. influenzae (12%) and M. catarrhalis (4%); several patients with polymicrobial CAP were enrolled. Linezolid was associated with greater resolution or improvement of symptoms of infection than ceftriaxone/cefpodoxime in the ITT population (83.0% vs 76.4%, respectively; p = 0.04) but not in the clinically evaluable (90.8% vs 88.6%, respectively) population of hospitalized patients with CAP. Similar effectiveness was reported for microbiologically evaluable patients in the two groups (89.9% vs 87.1%, respectively). These data suggest that linezolid should not be considered a first-line choice for patients with CAP, given the availability of effective older antibacterials for this infection.
1.3 Nosocomial Pneumonia
Two double-blind, multicentre RCTs with similar designs conducted by the same group of investigators have been conducted to study the effectiveness and safety of linezolid for the treatment of patients with Gram-positive nosocomial pneumonia, [31,34] In both RCTS, linezolid 600 mg every 12 hours was compared with vancomycin 1 g every 12 hours; aztreonam was added in both groups but discontinued if no Gram-negative bacteria were identified. In the first RCT, 396 patients comprised the ITT population;[34] in the second RCT, 623 patients received at least one dose of study medication.[31] A dropout rate of approximately 50% was reported for both RCTs. Baseline characteristics (including age, sex, race, Acute Physiology and Chronic Health Evaluation [APACHE] II score, need for ventilator support and days on ventilator before enrolment to the RCTs, chest radiograph and microbiological findings) and treatment duration were similar between the compared treatment groups in both RCTs, except that a more frequent multilobar involvement was found in patients treated with linezolid in one of the RCTs.[31] A pathogen was isolated in 43% of patients in the RCT by Rubinstein et al.[34] and 61% of patients in the RCT by Wunderink et al.[31] Gram-positive cocci were isolated from 45% of these patients in both RCTs, and patients with H. influenzae pneumonia were incorporated into this group. S. aureus was the most frequently isolated pathogen in both RCTs.
Linezolid and vancomycin were equally effective in resolving or improving the symptoms of nosocomial pneumonia in the clinically evaluable population (66% and 68% for linezolid-treated patients, and 68% and 65% for vancomycin-treated patients, for the two RCTs, respectively).[31,34] Although lower, the clinical success rates for the ITT populations were also similar between the compared antibacterials in both RCTs. Microbiological success was not significantly different between linezolid and vancomycin (62% and 68% for linezolid, and 52% and 73% for vancomycin, for the two RCTs, respectively). Eradication rates of all Gram-positive cocci were also similar. Finally, mortality was not different between the compared antibacterials in both RCTs (approximately 20% in both groups of patients in both RCTs). In addition, Rubinstein et al.[34] reported that the majority of these deaths in both groups of patients occurred during the follow-up period and “were attributed to the progression or complications of the severe underlying comorbidity”.
Pathogens were isolated from a total of 607 patients enrolled in these two RCTs.[31–34] Among them, 339 patients had nosocomial pneumonia due to S. aureus, and 160 patients had MRSA pneumonia. These patients were included in a retrospective analysis.[42] None of these isolates was resistant to vancomycin; in fact, 90% had an MIC <1 μ/mL. Linezolid was as effective as vancomycin for the treatment of patients (ITT population) with S. aureus pneumonia (51.5% vs 43.4%, respectively), but was associated with significantly greater treatment success than vancomycin in patients with MRSA pneumonia (59.0% vs 35.5%, respectively; p < 0.01). In addition, Kaplan-Meier analysis for mortality showed that linezolid was associated with non-significantly better survival than vancomycin in patients with S. aureus nosocomial pneumonia (78.0% vs 69.8%, respectively), and significantly better survival than vancomycin in the MRSA subset (80% vs 63.5%, respectively; p = 0.03). Linezolid administration was not among the predictors of clinical cure among patients with MRSA nosocomial pneumonia in the performed logistic regression analysis; however, it was a significant predictor of survival in all patients and in the subset of patients with MRSA nosocomial pneumonia.
Data regarding ventilator-associated pneumonia were not reported in these two publications.[31,34] However, a retrospective analysis of the combined data from these two RCTs, which included 544 patients with ventilator-associated pneumonia, was performed.[43] Among these patients, 264 had a confirmed Gram-positive ventilator-associated pneumonia. Linezolid was associated with a higher, statistically non-significant, clinical cure rate compared with vancomycin in all ventilator-associated pneumonia patients (45.4% vs 36.7%, respectively) and in ventilator-associated pneumonia patients with S. aureus infections (48.9% vs 35.2%, respectively). Clinical cure rates significantly favoured linezolid compared with vancomycin in the Grampositive (53.7% vs 37.7%, respectively; p = 0.02) and MRSA (62.2% vs 21.2%, respectively; p = 0.001) subsets. Logistical regression analysis showed that linezolid was an independent predictor of clinical cure for all patients, patients with Grampositive ventilator-associated pneumonia, and patients with MRSA ventilator-associated pneumonia. Kaplan-Meier survival rates favoured linezolid versus vancomycin in the MRSA subset (84.1% vs 61.7%, respectively; p = 0.02). On the other hand, Kaplan-Meier survival rates were similar for linezolid versus vancomycin therapy in all patients with ventilator-associated pneumonia (79.1% vs 73.7%, respectively), the Gram-positive subset (80.6% vs 70.8%, respectively), and the S. aureus subset (78.2% vs 70.3%, respectively). Logistical regression showed that linezolid was an independent predictor of survival for all patients, patients with Gram-positive cocci ventilator-associated pneumonia and patients with MRSA ventilator-associated pneumonia.
1.4 Complicated Skin and Soft Tissue Infections (SSTIs)
The most recently published study of linezolid for complicated SSTIs was a double-blind, multicentre RCT that compared linezolid 600 mg twice daily with dalbavancin 1 g on day 1 and 500 mg on day 8.[22] Patients were randomized in a 2 : 1 ratio. A total of 854 patients comprised the ITT population. Approximately 23% of patients were not clinically evaluable at the test-of-cure visit. MRSA was the predominantly isolated micro-organism. Linezolid and dalbavancin were equally effective for the treatment of patients with SSTIs (91.2% vs 88.9%, respectively). This was also true for patients with MRSA SSTIs (89% vs 91%, respectively). No differences between treatment groups were reported for patients with specific infections (abscess, cellulitis, surgical wound infections and burns).[22]
In another open-label, multicentre RCT, linezolid 600 mg twice daily was compared with vancomycin 1 g twice daily, followed by a semisynthetic penicillin when a susceptible strain was isolated.[24] In addition, 37% of linezolid-treated patients and 39% of vancomycin-treated patients also received antibacterials against Gram-negative bacilli. A total of 1200 patients were enrolled in the study, and 1180 comprised the ITT population. Approximately 25% of the ITT population was not considered clinically evaluable. Although the response rate was very high for both regimens, linezolid was more effective than vancomycin for the treatment of patients with SSTIs at the test-of-cure visit (94.4% vs 90.4%, respectively; p = 0.023). The same was true for the microbiologically evaluable population (94.5% vs 89.7%, respectively; p = 0.022). Linezolid was also more effective for the treatment of patients with major abscesses (98.3% vs 91.1%, respectively; p = 0.026) but not for patients with cellulitis or infected surgical wounds. Finally, linezolid was more effective than vancomycin for patients with MRSA SSTIs (88.6% vs 66.9%, respectively; p < 0.001), but not for patients with meticillin-susceptible S. aureus (84.9% vs 75.3%, respectively; p = 0.09) or S. pyogenes SSTIs (86.7% vs 94.4%, respectively). Despite the higher cure rates and the earlier change to oral therapy, linezolid was administered for a longer period of time than vancomycin (11.8 ± 4.9 days vs 10.9 ± 5.3 days, respectively; p = 0.004). In a sub-analysis of this RCT, patients with surgical wound infections were further evaluated.[44] In this analysis, linezolid was as effective as vancomycin in the clinically evaluable population but more effective than vancomycin in the microbiologically evaluable population (84% vs 58%, respectively; p = 0.0073) and in patients with MRSA infections (87% vs 48%, respectively; p = 0.0022).
In a double-blind, multicentre RCT, linezolid 600 mg twice daily was compared with oxacillin 2 g four times daily followed by dicloxacillin 500 mg four times daily for the treatment of patients with complicated SSTIs.[38] Patients with MRSA strains were excluded from this RCT. A total of 823 patients were enrolled in the trial and 819 received at least one dose of the compared antibacterials. A large number of dropouts were reported; 600 patients comprised the clinically evaluable population and 294 the microbiologically évaluable population. S. aureus was the most commonly isolated pathogen (140 in linezolid patients and 143 in oxacillin/ dicloxacillin patients). Streptococcal spp. were the second most prevalent isolates (S. pyogenes in 41 linezolid patients and 46 oxacillin/dicloxacillin patients, and S. agalactiae in 10 linezolid patients and 12 oxacillin/dicloxacillin patients). The effectiveness of both regimens was low in the ITT population (69.8% vs 64.9%, respectively). Linezolid was as effective as penicillins in the clinically evaluable population (88.6% vs 85.8%, respectively) and the microbiologically evaluable population (88.1% vs 86.1%, respectively). Eradication rates were also similar for all groups of isolated Gram-positive cocci.
1.5 Diabetic Foot Infections
Although the majority of the RCTs that studied the effectiveness of linezolid for the treatment of patients with SSTIs also included patients with diabetes mellitus, none of them specifically reported the outcomes for diabetic foot infections.[26] An open-label, multicentre RCT was designed to study the comparative effectiveness of linezolid 600 mg twice daily and aminopenicillins (sulbactam/ampicillin 1.5–3 g four times daily and amoxicillin/ clavulanic acid 625 mg three times daily or 1 g twice daily) for the treatment of diabetic foot infections.[26] Aztreonam could be added in cases of Gram-negative infection in both groups and vancomycin in cases of MRSA infection in the aminopenicillins group. This was the only RCT that allowed enrolment of patients with concomitant osteomyelitis. A total of 371 patients were enrolled in the study; 361 comprised the ITT population. Patients were randomized in a 2 : 1 ratio. Linezolid was more effective — although not statistically significantly so — than aminopenicillins for all SSTIs combined (81% vs 71%, respectively). However, linezolid was more effective for the treatment of patients with infected ulcers (81% vs 68%, respectively; p = 0.018) and for patients without concomitant osteomyelitis (87% vs 72%, respectively; p = 0.003). There was no difference between the two regimens regarding treatment of patients with osteomyelitis (61% vs 69%, respectively). The clinical cure rates, by baseline pathogen, were similar for the two treatment groups, except that the rate of clinical cure was significantly higher among linezolid recipients infected with S. agalactiae. The number of MRSA-infected patients in both groups was small.
1.6 Meticillin-Resistant Staphylococcus aureus SSTIs
Sharpe et al.[23] reported their experience from an open-label, single-centre RCT that enrolled patients with MRSA SSTIs requiring surgical intervention. A total of 117 patients were enrolled in this RCT; 57 were excluded from the final analysis. In this study, linezolid 600 mg twice daily was compared with vancomycin 1 g twice daily. Vancomycin-treated patients were older than those treated with linezolid. Treatment duration was similar between the two treatment groups. Linezolid was more effective than vancomycin in this population (97% vs 43%, respectively; p = 0.015); in addition, fewer linezolidtreated patients required amputation (0% vs 23.3%, respectively; p = 0.011).
In another multicentre RCT that compared the effectiveness of linezolid 600 mg twice daily with vancomycin 1 g twice daily for known or suspected MRSA infection, 460 patients were enrolled; 224 of these patients had an MRSA infection.[33] SSTIs were the most common infections, followed by pneumonia, urinary tract infections and bacteraemia. In both the ITT and microbiologically evaluable populations, linezolid was as effective as vancomycin for the treatment of MRSA infections (ITT: 56.8% vs 55.0%, respectively; microbiologically evaluable population: 73.2% vs 73.1%, respectively).
Finally, in a recently published RCT in patients with MRSA infections in Japan, 151 patients comprised the ITT population.[20] Patients with nosocomial pneumonia, SSTIs and sepsis were included. At the end of treatment, linezolid was as effective as vancomycin in the microbiologically evaluable patients (62.9% vs 50.0%, respectively), but linezolid was associated with higher eradication rates than vancomycin (79.0% vs 30.0%, respectively; p < 0.001).
1.7 Vancomycin-Resistant Enterococcal Infections
In a non-comparative, non-randomized, compassionate-use programme, linezolid intravenous (IV) or oral (PO) 600 mg daily for adults, or 10 mg/kg three times daily for children or adults weighing <40 kg, was used for the treatment of patients with serious multidrug-resistant, Gram-positive infections.[45] A total of 796 patients were enrolled, from whom 490 VRE faecium strains were isolated, comprising 59.2% of the total isolates in the study. Overall, in patients with VRE faecium infections, the cure rate in the clinical evaluable population was 81.4%; 5.8% of patients had infections that failed to respond to therapy and 12.8% of patients had indeterminate outcomes. More specifically, the clinical cure rate according to infection site was as follows: urinary tract infections 92%; intra-abdominal infections 91.4%; SSTIs 79.3%; bacteraemia 78%; endocarditis 76.9%; bone infections 75%; and lower respiratory tract infections 75%. The microbiological success rate in patients with VRE faecium infection was 86.4%, failure occurred in 12.7%, and the outcome was indeterminate in 0.9%.
In a single-centre, pilot RCT, linezolid IV or PO 600 mg twice daily was compared with quinupristin/ dalfopristin IV 7.5 mg/kg three times daily for the treatment of VRE faecium infections in cancer patients.[27] Forty patients were enrolled in the trial. Over 90% of patients in both treatment groups had either primary or secondary bacteraemia. More critically ill patients and more patients with pneumonia were enrolled in the quinupristin/dalfopristin group; no other differences between the treatment groups were reported. Linezolid was more effective than quinupristin/dalfopristin for the treatment of Grampositive infections in cancer patients, but this difference was not statistically significant in both clinically (58% vs 43%, respectively) and microbiologically evaluable (90% vs 71%, respectively) populations. Infection-related mortality was similar in the two treatment groups (16% vs 10%, respectively); all-cause mortality was not reported. Relapse rate was not statistically different between the compared antibacterials (21% vs 10%, respectively).
The efficacy of linezolid in patients with VRE infections was assessed in a multicentre, double-blind RCT.[39] This RCT compared the effectiveness of two linezolid doses in the treatment of patients with VRE infections because at the initiation of the study no alternative choice of therapy was available. A total of 145 patients were randomized to treatment with linezolid IV or PO 600 mg twice daily or 200 mg twice daily. The urinary tract was the most frequent site of VRE infections, followed by SSTIs, bacteraemia of unknown origin, peritonitis, intraabdominal infection, catheter-related infection and pneumonia. The average duration of antibacterial administration was similar in the two groups (15.0 and 16.1 days in the 200 mg and 600 mg groups, respectively). Cure rates were not significantly different between the two groups for all infections combined in the ITT population (67% vs 52%, respectively), as well as at each infection site. However, the microbiological outcome in the clinically evaluable population at follow-up was superior for the linezolid 600 mg group compared with the linezolid 200 mg group (88% vs 62%, respectively; p = 0.007). Similarly, success rates favoured the higher linezolid-dose group in microbiologically evaluable patients (86% vs 59%, respectively; p = 0.015).
1.8 Paediatric Populations
The results of an open-label, multicentre RCT that enrolled patients aged ≤12 years with hospitalacquired, Gram-positive infections (pneumonia, SSTIs, bacteraemias or other infections) have been published.[29] In this RCT, linezolid 10 mg/kg three times daily was compared with vancomycin 10–15 mg/kg one to four times daily according to dosing recommendations. Patients were randomized in a 2: 1 ratio; 316 patients comprised the ITT population. The discontinuation rate was high (approximately 30%). S. aureus (including MRSA) and coagulase-negative staphylococci (including meticillin-resistant strains, MRCNS) were the most commonly isolated pathogens. Linezolid was as effective as vancomycin in both ITT (79.1% vs 74.1%, respectively) and clinically evaluable (89.3% vs 84.5%, respectively) populations. Clinical cure rates were also similar in the two groups when specific infections were considered. In addition, clinical cure rates were comparable between linezolid and vancomycin in neonates (84% vs 77%, respectively).[46] Treatment duration was similar in the two groups, but IV treatment was shorter in linezolid-treated patients. Success rates were also similar in the microbiologically evaluable population (88.2% vs 87.0%, respectively). Pathogen eradication rates were similarly high in both treatment groups for all isolated groups of pathogens, including MRSA and MRCNS.
Linezolid has also been evaluated in two additional cohort studies for the treatment of children with recurrent otitis media[47] and CAP.[48] Linezolid was found to be effective in these studies.
1.9 Other Infections
In addition to its approved indications, linezolid has been used for the treatment of several other infectious diseases, including bacteraemia,[40] infections of the neutropenic host,[21] endocarditis,[49] urinary tract infections,[33,45] bone and joint infections,[50–52] infections of the CNS[53] and tuberculosis. [54] The majority of data regarding these infections (except for bacteraemia and neutropenia) arises from retrospective case series and case reports in which linezolid was usually administered as a rescue drug. These reports support the use of linezolid as an alternative to already approved antibacterials for the treatment of patients with such infections when previous treatments have failed, administration of other antibacterials is prohibited because of allergic reactions or other adverse events, or when IV administration of antibacterials is not feasible or acceptable.
A preliminary analysis of data from an openlabel RCT that included 726 patients with catheterrelated bacteraemia and catheter-site infections has been released online by the US FDA.[55] In this RCT, patients treated with linezolid had a higher probability of death than patients treated with vancomycin (78/363 patients [21.5%] vs 58/363 patients [16.0%], respectively). Mortality in patients with Gram-positive infections did not differ according to the antibacterial administered. However, mortality was higher in patients receiving linezolid for Gram-negative infections alone (4/15 [26.7%] vs 1/ 11 [9.1%], respectively), for those with both Grampositive and Gram-negative infections (16/46 [34.8%] vs 7/39 [17.9%], respectively) and for those in whom no micro-organism was isolated.[55]
2. Risk Assessment
In addition to relatively common adverse events described for several, if not all, antibacterials, such as vomiting, diarrhoea and rash, linezolid administration has been associated with a series of serious adverse events. Of these, anaemia, leukopenia and thrombocytopenia are most common, but lactic acidosis, optic and peripheral neuropathy, convulsions and serotonin-like syndrome are also noteworthy. In general, these serious adverse events occur either after prolonged linezolid administration (>2 weeks of therapy for myelosuppression or neuropathy) or simultaneous administration with other drugs or foods (e.g. monoamine oxidase inhibitors, selective serotonin reuptake inhibitors and adrenergic drugs or tyramine-containing foods for the development of serotonin-like syndrome). These adverse effects subside after discontinuation of linezolid.
Several articles investigating the development of adverse events probably or possibly associated with linezolid administration have been published. In a meta-analysis conducted by our team in which 12 RCTs were included,[40] we found that linezolid was associated with more adverse events than glycopeptides or β-lactams, but this finding did not reach statistical significance (OR = 1.40; 95% CI 0.95, 2.05). Headaches, diarrhoea, nausea and vomiting of mild to moderate severity were the most commonly reported adverse events. The number of patients who had to be withdrawn from the RCTs because of development of adverse events was equal for those receiving linezolid compared with those receiving glycopeptides or β-lactams (OR = 0.91; 95% CI 0.42, 1.96). There was no difference between the compared treatment groups for development of anaemia (OR = 1.43; 95% CI 0.74, 2.75), but linezolid was associated with significantly more episodes of thrombocytopenia (OR = 11.72; 95% CI 3.66, 37.57).
A pooled analysis that included seven RCTs was published in 2003.[56] This meta-analysis was restricted to the assessment of the safety and tolerability of linezolid in comparison with other antibacterials (vancomycin, β-lactams and macrolides). Overall, linezolid was associated with more adverse events than comparator antibacterials (21.7% vs 15.7%, respectively; p = 0.001). However, there was no difference between the compared antibacterials in serious adverse events (11.4% vs 10.6%, respectively) or in patients discontinuing the studied antibacterials because of adverse events (2.4% vs 1.9%, respectively). The most common drug-related adverse events associated with both linezolid and comparator agents were diarrhoea (4.3 and 3.2%, respectively; p = 0.074), nausea (3.4 and 2.3%, respectively; p = 0.036) and headache (2.2 and 1.3%, respectively; p = 0.047). Other potentially drugrelated adverse events that were reported in >0.1% but <1% of linezolid-treated patients included abdominal pain, chills, fatigue, fungal infections (moniliasis), localized pain, increase in ALT levels, hypertension, dyspepsia, glossitis, stomatitis, tongue discolouration, eosinophilia, thrombocytopenia, dizziness, insomnia, paraesthesia, pruritus and rash. The rates of C. difficile-related complications were similar between linezolid and comparator agents. C. difficile was reported in 0.2% of linezolid-treated patients and 0.4% of comparator drug-treated patients. Analyses[56] showed essentially no difference between linezolid and comparator antibacterials in the cumulative percentage of patients with outlying haemoglobin, neutrophil or platelet counts over the first 14 days of therapy. However, with longer treatment durations, there appeared to be a small increased risk of decreased platelet counts in linezolid-treated patients compared with the risk for the comparator group, but the difference was not statistically significant.
Linezolid-related haematological adverse effects may not increase in patients receiving chemotherapy for haematological malignancies. An RCT conducted in neutropenic patients, in whom the most common diagnosis was haematological malignancy and treatment was expected to continue for 10–28 days, indicated that myelosuppression is no more likely to occur in patients receiving linezolid than in those receiving vancomycin.[21]
Lactic acidosis has also been reported with the use of linezolid. In reported cases, patients experienced repeated episodes of nausea and vomiting [57,58] Convulsions have also been reported: in some of these cases, a history of seizures or risk factors for seizures was present.[7]
The association between duration of linezolid administration and development of drug-related adverse events was more evident when the drug was used to treat infections that require prolonged antimicrobial administration. In such cases (i.e. treatment of endocarditis,[49] bone and joint infections[52] and tuberculosis[54]) adverse events were reported to be several-fold higher than in patients with pneumonia or SSTIs. Therefore, complete blood counts once a week are required when linezolid is administered for >2 weeks. Peripheral and optic neuropathy have also been reported in patients treated with linezolid. These adverse effects have occurred primarily in patients treated for longer than the maximum recommended duration of 28 days; indeed, in many of these patients, treatment durations of 3–6 months were employed.[59,60]
Finally, in a review that evaluated the development of adverse events after linezolid administration in children, the authors reported that the most commonly observed adverse events were diarrhoea, vomiting and nausea.[61] However, none of these adverse events was more commonly reported in the linezolid group than in comparator antibacterial groups.[61]
3. Comments
The effectiveness of linezolid has been investigated in several studies. These have shown that linezolid is at least as effective as comparator antibacterials for the treatment of patients with both CAP and nosocomial pneumonia, and is better than comparators for the treatment of patients with SSTIs. In relation to CAP, we believe that the currently available evidence suggests that linezolid should not be used as first-line empirical treatment because it lacks activity against atypical pathogens and Gramnegative bacilli, which are common causes of this infection. In addition, several other treatment options are currently available that are highly effective for such patients.[62] Linezolid could be considered as a treatment option in cases of severe CAP but only in addition to β-lactams and/or fluoroquinolones.
On the other hand, use of linezolid for the treatment of nosocomial pneumonia should be considered more often. Several reasons may justify selection of this agent in this context. First, linezolid has a better pharmacokinetic and pharmacodynamic profile than vancomycin, the antibacterial that has been considered the drug of choice for suspected nosocomial pneumonia due to Gram-positive microorganisms. It has been suggested that the vancomycin concentration achieved in the lungs (after administration of the usual dosage of 1 g twice daily) is approximately 20% of that measured in plasma, resulting in a concentration below the MIC for the majority of susceptible pathogens.[11,63] In contrast, mean linezolid concentrations in lung tissue and epithelial lining fluid were reported to be higher than those in blood or plasma.[11,63] Second, vancomycin is usually coadministered with other antibacterials (e.g. aminoglycosides or β-lactams such as aztreonam) that may act as antagonists to it.[64] Third, use of vancomycin leads to cell death and the release of higher levels of exotoxins and other inflammation inducers to the circulation than linezolid, consequences that may increase the overall severity of the infection.[65] Finally, the other currently approved antibacterials for the treatment of Grampositive infections cannot be used for the treatment of nosocomial pneumonia. Daptomycin activity is inhibited in the lungs by pulmonary surfactant,[66] while quinupristin/dalfopristin has not been approved for the treatment of pneumonia although it has been shown to be as effective as vancomycin in an RCT.[67] Telavancin, ceftobiprole and tigecycline have been also evaluated in RCTs. Although all were equally effective to their comparator antibacterials in each RCT for the treatment of patients with nosocomial pneumonia, only telavancin was as effective as its comparator regimen for the treatment of patients with ventilator-associated pneumonia.[68–70]
Conversely, the currently available evidence, albeit debatable,[40,71–73] suggests that linezolid is probably more effective than vancomycin for the treatment of MRSA nosocomial pneumonia, including ventilator-associated pneumonia. However, there was no difference between the two drugs when all pneumonia patients were included in the analyses. Currently, Gram-positive cocci are the leading cause of nosocomial infections,[74–76] and the incidence of MRSA infections is increasing.[77,78] Therefore, the important question at this point is whether linezolid should replace vancomycin as the empirical treatment option in all patients with nosocomial pneumonia or should it be restricted to those who have several risk factors for MRSA nosocomial pneumonia and those who receive care in hospitals with high MRSA prevalence. In a recent systematic review of outcomes for patients with MRSA or other S. aureus ventilator-associated pneumonia, the authors concluded that the presence of meticillin resistance was associated with higher mortality. However, these authors also argued that there is probably no causal relationship between meticillin resistance and mortality, and that the higher mortality may have been attributable to confounders such as severity of underlying diseases, inadequacy of empirical treatment and duration of intensive care unit stay.[79]
Linezolid has been shown to be better than comparator antibacterials (β-lactams, glycopeptides and macrolides) for the treatment of patients with SSTIs.[40] However, the latter antibacterials were also highly effective for the treatment of SSTIs (90.3% success with linezolid vs 85.7% with comparator antibacterials).[40] Furthermore, the RCTs that studied the effectiveness of linezolid for SSTIs excluded patients with the most severe forms, such as gangrene, necrotizing fasciitis and concurrent osteomyelitis, and several of them included only patients with uncomplicated SSTIs (table I). Therefore, there is no good reason to use linezolid as a first-line treatment option for SSTIs and increase the possibility of development of resistance to an antibacterial that is valuable for more severe infections.
Finally, the limited available evidence from RCTs suggests that linezolid is more effective than comparator antibacterials for the treatment of patients with Gram-positive bacteraemia[40] but not for patients with MRSA bacteraemia.[80] These RCTs did not enrol patients with catheter-related bloodstream infections; rather, patients in these trials had bacteraemias of unknown origin or secondary to other infections. The FDA has released a report file suggesting that linezolid administration is associated with higher mortality than vancomycin in patients with catheter-related blood stream infections; the main difference was observed in patients with Gram-negative bacteremia.[55] The FDA committee was not prepared to make any recommendation regarding use of linezolid in the treatment of catheter-related bacteraemias until further analysis of the data had been completed.
There are limited options available for treatment of patients with VRE infections. Clinical suspicion for VRE infection is probably the only unchallengeable reason for empirical use of linezolid as a firstline antibacterial choice. The lack of comparative data for infections such as endocarditis or osteomyelitis do not allow us to proceed to recommendations regarding use of linezolid in such patients, although several associations have already incorporated use of this drug into their guidelines.[62,81]
Although linezolid has been associated with more adverse events than comparator antibacterials, these were mild to moderate in severity, mainly involved nausea, vomiting, diarrhoea or headache, subsided early after drug discontinuation and were never associated with the death of patients in RCTs. However, physicians should always remember the association between duration of linezolid administration and development of serious adverse events, and monitor complete blood counts at least once a week. In addition, there is evidence that although optic neuropathy usually subsides after discontinuation of linezolid administration, peripheral neuropathy may persist.[82] Therefore, close surveillance is warranted when longer treatment duration (>28 days) with linezolid, mainly for off-label indications, is employed.
4. Conclusion
Linezolid is an important, effective and relatively safe treatment option for the treatment of Grampositive infections. It has a favourable pharmacokinetic profile and surveillance programmes have shown that is highly active against multidrug-resistant, Gram-positive cocci. Its unique mechanism of action suggests that resistance is relatively unlikely to develop, but unwise and uncontrolled prescription will definitely lead to resistant micro-organisms. In order to preserve the role of linezolid in current therapeutics, its use should be limited to specific patient populations (VRE infections, hospitals with high prevalence of MRSA, patients with several risk factors for multi-drug resistant Gram-positive pathogens) and after consideration of data from relevant antimicrobial resistance surveillance studies and hospital infection control programmes.
References
Dresser LD, Rybak MJ. The pharmacologic and bacteriologic properties of oxazolidinones, a new class of synthetic antimicrobials. Pharmacotherapy 1998; 18(3): 456–62
Noskin GA, Siddiqui F, Stosor V, et al. In vitro activities of linezolid against important gram-positive bacterial pathogens including vancomycin-resistant enterococci. Antimicrob Agents Chemother 1999; 43(8): 2059–62
Lin AH, Murray RW, Vidmar TJ, et al. The oxazolidinone eperezolid binds to the 50S ribosomal subunit and competes with binding of chloramphenicol and lincomycin. Antimicrob Agents Chemother 1997; 41(10): 2127–31
Shinabarger DL, Marotti KR, Murray RW, et al. Mechanism of action of oxazolidinones: effects of linezolid and eperezolid on translation reactions. Antimicrob Agents Chemother 1997; 41(10): 2132–6
Zurenko GE, Yagi BH, Schaadt RD, et al. In vitro activities of U-100592 and U-100766, novel oxazolidinone antibacterial agents. Antimicrob Agents Chemother 1996; 40(4): 839–45
Perry CM, Jarvis B. Linezolid: a review of its use in the management of serious Gram-positive infections. Pediatr Drugs 2003; 5(6): 419–29
Zyvox® [package insert]. New York (NY); Pfizer Inc.; 2007 [online]. Available from URL: http://www.pfizer.com/pfizer/download/uspi_zyxox.pdf [Accessed on 2007 Jul 15]
Andes D, van Ogtrop ML, Peng J, et al. In vivo pharmacodynamics of a new oxazolidinone (linezolid). Antimicrob Agents Chemother 2002; 46(11): 3484–9
Stalker DJ, Jungbluth GL. Clinical pharmacokinetics of linezolid, a novel oxazolidinone antibacterial. Clin Pharmacokinet 2003; 42(13): 1129–40
Stalker DJ, Jungbluth GL, Hopkins NK, et al. Pharmacokinetics and tolerance of single- and multiple-dose oral or intravenous linezolid, an oxazolidinone antibiotic, in healthy volunteers. J Antimicrob Chemother 2003; 51(5): 1239–46
Conte Jr JE, Golden JA, Kipps J, et al. Intrapulmonary pharmacokinetics of linezolid. Antimicrob Agents Chemother 2002; 46(5): 1475–80
Stevens DL, Dotter B, Madaras-Kelly K. A review of linezolid: the first oxazolidinone antibiotic. Expert Rev Anti Infect Ther 2004; 2(1): 51–9
Lovering AM, Zhang J, Bannister GC, et al. Penetration of linezolid into bone, fat, muscle and haematoma of patients undergoing routine hip replacement. J Antimicrob Chemother 2002; 50(1): 73–7
Sabbatani S, Manfredi R, Frank G, et al. Linezolid in the treatment of severe central nervous system infections resistant to recommended antimicrobial compounds. Infez Med 2005; 13(2): 112–9
Rana B, Butcher I, Grigoris P, et al. Linezolid penetration into osteo-articular tissues. J Antimicrob Chemother 2002; 50(5): 747–50
Buerger C, Plock N, Dehghanyar P, et al. Pharmacokinetics of unbound linezolid in plasma and tissue interstitium of critically ill patients after multiple dosing using microdialysis. Antimicrob Agents Chemother 2006; 50(7): 2455–63
French G. Safety and tolerability of linezolid. J Antimicrob Chemother 2003; 51 Suppl. 2: ii45–53
Slatter JG, Stalker DJ, Feenstra KL, et al. Pharmacokinetics, metabolism, and excretion of linezolid following an oral dose of [(14)C] linezolid to healthy human subjects. Drug Metab Dispos 2001; 29(8): 1136–45
Macgowan AP. Pharmacokinetic and pharmacodynamic profile of linezolid in healthy volunteers and patients with Grampositive infections. J Antimicrob Chemother 2003; 51 Suppl. 2: ii17–25
Kohno S, Yamaguchi K, Aikawa N, et al. Linezolid versus vancomycin for the treatment of infections caused by methicillin-resistant Staphylococcus aureus in Japan. J Antimicrob Chemother 2007; 60: 1361–9
Jaksic B, Martinelli G, Perez-Oteyza J, et al. Efficacy and safety of linezolid compared with vancomycin in a randomized, double-blind study of febrile neutropenic patients with cancer. Clin Infect Dis 2006; 42: 597–607
Jauregui LE, Babazadeh S, Seltzer E, et al. Randomized, double-blind comparison of once-weekly dalbavancin versus twicedaily linezolid therapy for the treatment of complicated skin and skin structure infections. Clin Infect Dis 2005; 41: 1407–15
Sharpe JN, Shively EH, Polk Jr HC. Clinical and economic outcomes of oral linezolid versus intravenous vancomycin in the treatment of MRSA-complicated, lower-extremity skin and soft-tissue infections caused by methicillin-resistant Staphylococcus aureus. Am J Surg 2005; 189(4): 425–8
Weigelt J, Itani K, Stevens D, et al. Linezolid versus vancomycin in treatment of complicated skin and soft tissue infections. Antimicrob Agents Chemother 2005; 49(6): 2260–6
Cepeda JA, Whitehouse T, Cooper B. Linezolid versus teicoplanin in the treatment of Gram-positive infections in the critically ill: a randomized, double-blind, multicentre study. J Antimicrob Chemother 2004; 53(2): 345–55
Lipsky BA, Itani K, Norden C. Treating foot infections in diabetic patients: a randomized, multicenter, open-label trial of linezolid versus ampicillin-sulbactam/amoxicillin-clavulanate. Clin Infect Dis 2004; 38(1): 17–24
Raad I, Hachem R, Hanna H, et al. Prospective, randomized study comparing quinupristin-dalfopristin with linezolid in the treatment of vancomycin-resistant Enterococcus faecium infections. J Antimicrob Chemother 2004; 53(4): 646–9
Wilcox M, Nathwani D, Dryden M. Linezolid compared with teicoplanin for the treatment of suspected or proven Grampositive infections. J Antimicrob Chemother 2004; 53(2): 335–44
Kaplan SL, Deville JG, Yogev R, et al. Linezolid versus vancomycin for treatment of resistant Gram-positive infections in children. Pediatr Infect Dis J 2003; 22(8): 677–86
Wible K, Tregnaghi M, Brass J, et al. Linezolid versus cefadroxil in the treatment of skin and skin structure infections in children. Pediatr Infect Dis J 2003; 22(4): 315–23
Wunderink RG, Cammarata SK, Oliphant TH, et al. Continuation of a randomized, double-blind, multicenter study of linezolid versus vancomycin in the treatment of patients with nosocomial pneumonia. Linezolid Nosocomial Pneumonia Study Group. Clin Ther 2003; 25(3): 980–92
San Pedro GS, Cammarata SK, Oliphant TH, et al. Linezolid versus ceftriaxone/cefpodoxime in patients hospitalized for the treatment of Streptococcus pneumoniae pneumonia. Linezolid Community-Acquired Pneumonia Study Group. Scand J Infect Dis 2002; 34(10): 720–8 767
Stevens DL, Herr D, Lampiris H, et al. Linezolid versus vancomycin for the treatment of methicillin-resistant Staphylococcus aureus infections. Clin Infect Dis 2002; 34(11): 1481–90
Rubinstein E, Cammarata S, Oliphant T, et al. Linezolid (PNU-100766) versus vancomycin in the treatment of hospitalized patients with nosocomial pneumonia: a randomized, double-blind, multicenter study. Linezolid Nosocomial Pneumonia Study Group. Clin Infect Dis 2001; 32(3): 402–12
Cammarata SK, Bermudez M, Golin V, et al. Comparison of linezolid versus ceftriaxone/cefpodoxime in the treatment of hospitalized community-acquired pneumonia [abstract no. 80.008]. In: Program and abstracts of the 9th International Congress on Infectious Diseases, Buenos Aires; International Society of Infectious Diseases; 2000 Apr 10–13, Boston (MA)
Cammarata SK, Schueman LK, Timm JA, et al. Oral linezolid in the treatment of community-acquired pneumonia: a phase III trial [abstract no. E73]. In: Program and abstracts of the American Thoracic Society, Toronto; American Thoracic Society; 2000 May 5–10, New York, 654
Duvall SE, Seas C, Bruss JB, et al. Comparison of linezolid to oral clarithromycin in the treatment of uncomplicated skin infections: results from a multinational phase III trial [abstract no. 80.005]. In: Program and abstracts of the 9th International Congress on Infectious Diseases, Buenos Aires; International Society of Infectious Diseases; 2000 Apr 10–13, Boston (MA), 181
Stevens DL, Smith LG, Bruss JB, et al. Randomized comparison of linezolid (PNU-100766) versus oxacillin-dicloxacillin for treatment of complicated skin and soft tissue infections. Antimicrob Agents Chemother 2000; 44(12): 3408–13
Hartman CS, Leach TS, Kaja RW, et al. Linezolid in the treatment of vancomycin-resistant Enterococcus: a dose comparative, multicenter phase III trial [abstract no. 2235]. In: 40th Interscience Conference on Antimicrobial Agents and Chemotherapy, Toronto; American Society for Microbiology; 2000 Sep 17–20, Washington (DC), 488
Falagas ME, Siempos II, Vardakas KZ. Linezolid versus a glycopeptide or β-lactam for treatment of Gram-positive bacterial infections: a meta-analysis of randomized controlled trials. Lancet Infect Dis 2008; 8(1): 53–66
Arnold FW, Summersgill JT, Lajoie AS, et al. A worldwide perspective of atypical pathogens in community-acquired pneumonia. Community-Acquired Pneumonia Organization (CAPO) investigators. Am J Respir Crit Care Med 2007; 175(10): 1086–93
Wunderink RG, Rello J, Cammarata SK, et al. Linezolid vs vancomycin: analysis of two double-blind studies of patients with methicillin-resistant Staphylococcus aureus nosocomial pneumonia. Chest 2003; 124: 1789–97
Kollef MH, Rello J, Cammarata SK, et al. Clinical cure and survival in Gram-positive ventilator-associated pneumonia: retrospective analysis of two double-blind studies comparing linezolid with vancomycin. Intensive Care Med 2004; 30: 388–94
Weigelt J, Kaafarani HM, Itani KM, et al. Linezolid eradicates MRSA better than vancomycin from surgical-site infections. Am J Surg 2004; 188(6): 760–6
Birmingham MC, Rayner CR, Meagher AK, et al. Linezolid for the treatment of multidrug-resistant, gram-positive infections: experience from a compassionate-use program. Clin Infect Dis 2003; 36: 159–68
Deville JG, Adler S, Azimi PH, et al. Linezolid versus vancomycin in the treatment of known or suspected resistant grampositive infections in neonates. Pediatr Infect Dis J 2003; 22 (9 Suppl.): S158–63
Fleishaker DL, Anderson DC, Bruss JB, et al. Clinical efficacy of linezolid (LZD) in the treatment of otitis media [abstract no.65]. In: Abstracts of the 38th Annual Meeting of the Infectious Diseases Society of America, New Orleans; Infectious Diseases Society of America; 2000 Sep 7–10; Alexandria (VA): 31, 224
Kaplan SL, Patterson L, Edwards KM, et al. Linezolid for the treatment of community-acquired pneumonia in hospitalized children. Linezolid Pediatric Pneumonia Study Group. Pediatr Infect Dis J 2001; 20: 488–94
Falagas ME, Manta KG, Ntziora F, et al. Linezolid for the treatment of patients with endocarditis: a review of the published evidence. J Antimicrob Chemother 2006; 58: 273–80
Senneville E, Legout L, Valette M, et al. Effectiveness and tolerability of prolonged linezolid treatment for chronic osteomyelitis: a retrospective study. Clin Ther 2006; 28(8): 1155–63
Harwood PJ, Talbot C, Dimoutsos M, et al. Early experience with linezolid for infections in orthopaedics. Injury 2006; 37(9): 818–26
Falagas ME, Siempos II, Papagelopoulos PJ, et al. Linezolid for the treatment of adults with bone and joint infections. Int J Antimicrob Agents 2007; 29(3): 233–9
Ntziora F, Falagas ME. Linezolid for the treatment of patients with CNS infection. Ann Pharmacother 2007; 41: 296–308
Ntziora F, Falagas ME. Linezolid for the treatment of patients with mycobacterial infection: a systematic review. Int J Tuberc Lung Dis 2007; 11(6): 606–11
US FDA. FDA alert: information for health care professionals regarding linezolid [online]. Available from URL: http://www.fda.gov/cder/dr~g/InfoSheets/HCP/linezolidHCP.pdf [Accessed 2007 Mar 22]
Rubinstein E, Isturiz R, Standiford HC, et al. Worldwide assessment of linezolid’s clinical safety and tolerability: comparatorcontrolled phase III studies. Antimicrob Agents Chemother 2003; 47(6): 1824–31
Kopterides P, Papadomichelakis E, Armaganidis A. Linezolid use associated with lactic acidosis. Scand J Infect Dis 2005; 37(2): 153–4
Narita M, Tsuji BT, Yu VL. Linezolid-associated peripheral and optic neuropathy, lactic acidosis, and serotonin syndrome. Pharmacotherapy 2007; 27(8): 1189–97
Corallo CE, Pauli AE. Linezolid-induced neuropathy [letter]. Med J Aust 2002; 177: 332
Lee E, Burger S, Shah J, et al. Linezolid-associated toxic optic neuropathy: a report of 2 cases. Clin Infect Dis 2003; 37:1389–91
Saiman L, Goldfarb J, Kaplan SA, et al. Safety and tolerability of linezolid in children. Pediatr Infect Dis J 2003; 22(9): S193–200
Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007; 44 Suppl. 2: S27–72
Honeybourne D, Tobin C, Jevons G, et al. Intrapulmonary penetration of linezolid. J Antimicrob Chemother 2003 Jun; 51(6): 1431–4
Ioanas M, Lode H. Linezolid in VAP by MRSA: a better choice? Intensive Care Med 2004; 30: 343–6
Micek ST, Dunne M, Kollef MH. Pleuropulmonary complications of Panton-Valentine leukocidin-positive community-acquired 768 quired methicillin-resistant Staphylococcus aureus: importance of treatment with antimicrobials inhibiting exotoxin production. Chest 2005; 128(4): 2732–8
Silverman JA, Mortin LI, Vanpraagh AD, et al. Inhibition of daptomycin by pulmonary surfactant: in vitro modelling and clinical impact. J Infect Dis 2005; 191(12): 2149–52
Fagon J, Patrick H, Haas DW, et al. Treatment of Gram-positive nosocomial pneumonia: prospective randomized comparison of quinupristin/dalfopristin versus vancomycin. Nosocomial Pneumonia Group. Am J Respir Crit Care Med 2000; 161: 753–62
Effectiveness of ceftobiprole for the treatment of patients with hospital-acquired pneumonia [online]. Available from URL: http://www.sys-con.com/read/440454.htm [Accessed on 2008 Feb 12]
Effectiveness of ceftobiprole for the treatment of patients with hospital-acquired pneumonia [online]. Available from URL: http://www.redorbit.com/news/health/1170950/theravance_announces_positive_topline_results_in_phase_3_telavancin_hospitalacquired/index.html [Accessed 2008 Feb 12]
Maroko R, Cooper A, Dukart G, et al. Results of phase 3 study comparing a tigecycline (TGC) regimen with an imipenem/ cilastatin (IMI) regimen in treatment of patients (pts) with hospital-acquired pneumonia (HAP) [abstract no. L730]. In: Program and abstracts of the 47th International Congress on Antimicrobial Agents and Chemotherapy; 2007 Sep 17–20, Chicago (IL)
Powers JH, Ross DB, Lin D, et al. Linezolid and vancomycin for methicillin-resistant Staphylococcus aureus nosocomial pneumonia: the subtleties of subgroup analyses. Chest 2004; 126(1): 314–5
Kalil AC, Puumala SE, Stoner J. Unresolved questions with the use of linezolid vs vancomycin for nosocomial pneumonia. Chest 2004; 125(6): 2370–1
Vardakas KZ, Ntziora F, Falagas ME. Linezolid: effectiveness and safety for approved and off-label indications. Expert Opin Pharmacother 2007; 8(14): 2381–400
Diekema DJ, Pfaller MA, Schmitz FJ, et al. Survey of infections due to Staphylococcus species: frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacific region for the SENTRY Antimicrobial Surveillance Program, 1997–1999. SENTRY Participants Group. Clin Infect Dis 2001; 32 Suppl. 2: SI 14–32
Richards MJ, Edwards JR, Culver DH, et al. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect Control Hosp Epidemiol 2000; 21(8): 510–5
Vincent JL, Bihari DJ, Suter PM, et al. The prevalence of nosocomial infection in intensive care units in Europe: results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC International Advisory Committee. JAMA 1995; 274(8): 639–44
Doern GV, Jones RN, Pfaller MA, et al. Bacterial pathogens isolated from patients with skin and soft tissue infections: frequency of occurrence and antimicrobial susceptibility patterns from the SENTRY Antimicrobial Surveillance Program (United States and Canada, 1997). SENTRY Study Group (North America). Diagn Microbiol Infect Dis 1999; 34(1): 65–72
Rennie RP, Jones RN, Mutnick AH, et al. Occurrence and antimicrobial susceptibility patterns of pathogens isolated from skin and soft tissue infections: report from the SENTRY Antimicrobial Surveillance Program (United States and Canada, 2000). SENTRY Program Study Group (North America). Diagn Microbiol Infect Dis 2003; 45(4): 287–93
Athanassa Z, Siempos II, Falagas ME. Impact of methicillin resistance on the mortality of S. aureus VAP: a systematic review. Eur Respir J 2008 Mar; 31(3): 625–32
Shorr AF, Kunkel MJ, Kollef M. Linezolid versus vancomycin for Staphylococcus aureus bacteraemia: pooled analysis of randomized studies. J Antimicrob Chemother 2005; 56(5): 923–9
Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications. A statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation 2005; 111: e394–434
Bressler AM, Zimmer SM, Gilmore JL, et al. Peripheral neuropathy associated with prolonged use of linezolid. Lancet Infect Dis 2004; 4(8): 528–31
Acknowledgements
No sources of funding were used to assist in the preparation of this review. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Falagas, M.E., Vardakas, K.Z. Benefit-Risk Assessment of Linezolid for Serious Gram-Positive Bacterial Infections. Drug-Safety 31, 753–768 (2008). https://doi.org/10.2165/00002018-200831090-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200831090-00004