Abstract
Although the number of clinically relevant drug-drug interactions (DDIs) is probably low, DDIs may be responsible for a substantial number of hospital admissions. In some countries, the pharmacist is responsible for preventing the use of unsafe or non-effective drug regimens. Specifically they should avoid the dispensing of combinations of drugs that may cause serious DDIs. In order to assess the determinants related to community pharmacies and associated with these dispensings, a systematic literature review was conducted. Medline and International Pharmaceutical Abstracts were searched for articles published in English between 1993 and 2003. Additional relevant articles were identified by screening the reference lists of relevant articles.
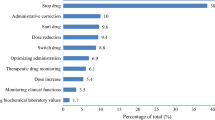
Seven papers were located. The determinants described in the literature were divided into three groups. The first group focussed on the relationship between the pharmacist and the prescriber. The number of prescribers is of importance as well as the number of dispensing pharmacies. Both a high number of primary care physicians and multiple dispensing pharmacies increased the risk of DDIs. The availability, quality and sensitivity of the medication surveillance software appeared to be a second important determinant. Both too many and too few signals increased the risk of dispensing interacting drugs. The third group of determinants was related to the pharmacist and pharmacy organisation. Signals from the surveillance program are usually judged first by technicians and subsequently managed by the pharmacist. Consequently, knowledge, instructions and supervision are important determinants. A fourth group of determinants was identified in literature assessing interventions by pharmacists, including interventions for DDIs. A higher workload was associated with lower intervention rates, which indicated a higher risk of dispensing interacting drugs.
The determinants identified in this review can be used to develop strategies to minimise patient harm resulting from DDIs. Further assessment of the relation between these determinants and the dispensing of DDIs and of the relation between DDI-associated dispensing and patient harm is recommended.



Similar content being viewed by others
References
Schalekamp T. Omgaan met geneesmiddeleninteracties. Geneesmiddelenbulletin 1997; 31(8): 87–94
Bergendal L, Friberg A, Schaffrath A. Potential drug-drug interactions in 5,125 mostly elderly out-patients in Gothenburg, Sweden. Pharm World Sci 1995; 17(5): 152–7
Linnarsson R. Drug interactions in primary health care: a retrospective database study and its implications for the design of a computerized decision support system. Scand J Prim Health Care 1993; 11(3): 181–6
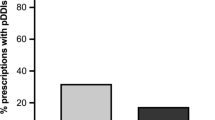
Merlo J, Liedholm H, Lindblad U, et al. Prescriptions with potential drug interactions dispensed at Swedish pharmacies in January 1999: cross sectional study. BMJ 2001; 323(7310): 427–8
Buurma H, de Smet PA, van den Hoff OP, et al. Nature, frequency and determinants of prescription modifications in Dutch community pharmacies. Br J Clin Pharmacol 2001; 52(1): 85–91
Caleo S, Benrimoj S, Collins D, et al. Clinical evaluation of community pharmacists’ interventions. Int J Pharm Pract 1996; (4): 221–7
Hawksworth GM, Corlett AJ, Wright DJ, et al. Clinical pharmacy interventions by community pharmacists during the dispensing process. Br J Clin Pharmacol 1999; 47(6): 695–700
Rupp MT, DeYoung M, Schondelmeyer SW. Prescribing problems and pharmacist interventions in community practice. Med Care 1992; 30(10): 926–40
Westein MP, Herings RM, Leufkens HG. Determinants of pharmacists’ interventions linked to prescription processing. Pharm World Sci 2001; 23(3): 98–101
Westerlund T, Almarsdottir AB, Melander A. Factors influencing the detection rate of drug-related problems in community pharmacy. Pharm World Sci 1999; 21(6): 245–50
Huic M, Mucolic V, Vrhovac B, et al. Adverse drug reactions resulting in hospital admission. Int J Clin Pharmacol Ther 1994; 32(12): 675–82
Jankel CA, Fitterman LK. Epidemiology of drug-drug interactions as a cause of hospital admissions. Drug Saf 1993; 9(1): 51–9
McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother 2002; 36(9): 1331–6
Peyriere H, Cassan S, Floutard E, et al. Adverse drug events associated with hospital admission. Ann Pharmacother 2003; 37(1): 5–11
Donabedian A. The seven pillars of quality. Arch Pathol Lab Med 1990; 114(11): 1115–8
Bates DW, Leape LL. Pharmacies and prevention of potentially fatal drug interactions. JAMA 1996; 275(14): 1086–7
Halkin H, Katzir I, Kurman I, et al. Preventing drug interactions by online prescription screening in community pharmacies and medical practices. Clin Pharmacol Ther 2001; 69(4): 260–5
Hazlet TK, Lee TA, Hansten PD, et al. Performance of community pharmacy drug interaction software. J Am Pharm Assoc 2001; 41(2): 200–4
Heijboer-Vinks IC. Kwaliteitszorg in de medicatiebewaking. Den Haag: KNMP/WINAp, 1998
Tamblyn RM, Huang A, Perreault R, Jacques A, Roy D, Hanley J, et al. The medical office of the 21st century (MOXXI): effectiveness of computerized decision-making support in reducing inappropriate prescribing in primary care. CMAJ 3 A.D. 2003; 169(6): 549–556
Tamblyn RM, McLeod PJ, Abrahamowicz M, et al. Do too many cooks spoil the broth?: multiple physician involvement in medical management of elderly patients and potentially inappropriate drug combinations. CMAJ 1996; 154(8): 1177–84
Cavuto NJ, Woosley RL, Sale M. Pharmacies and prevention of potentially fatal drug interactions. JAMA 1996; 275(14): 1086–7
Kraft KE, Dore FH. Computerized drug interactions programs: how reliable? [letter]. JAMA 1996; 275(14): 1087
Currie JD, Chrischilles EA, Kuehl AK, et al. Effect of a training program on community pharmacists’ detection of and intervention in drug-related problems. J Am Pharm Assoc 1997; NS37(2): 182–91
Armstrong EP, Denemark CR. How pharmacists respond to online, real-time DUR alerts. J Am Pharm Assoc 1998; 38(2): 149–54
van Mil JWF, Dudok van Heel MC, Boersma M, et al. Interventions and documentation for drug-related problems in Dutch community pharmacies. Am J Health Syst Pharm 2001; 58(15): 1428–31
Acknowledgements
We thank the following persons for their participation in the project group: Dirk M. Barends of the National Institute of Public Health and the Environment, Bilthoven, The Netherlands, and Riekert J. Bruinink and Nico B. Kylstra of the Inspectorate for Health Care, The Hague, The Netherlands.
We would also like to thank Henk Buurma of the SIR Institute for Pharmacy Practice Research, Leiden, The Netherlands/Utrecht University, Utrecht, The Netherlands, for his critical comments.
No sources of funding were used to assist in the preparation of this study. The authors have no conflicts of interest that are directly relevant to the content of this study
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Becker, M.L., Kallewaard, M., Caspers, P.W. et al. Potential Determinants of Drug-Drug Interaction Associated Dispensing in Community Pharmacies. Drug-Safety 28, 371–378 (2005). https://doi.org/10.2165/00002018-200528050-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200528050-00001