Abstract
In Duchenne muscular dystrophy (DMD) patients and the mdx mouse model of DMD, chronic activation of the classical nuclear factor-κB (NF-κB) pathway contributes to the pathogenesis that causes degeneration of muscle fibers, inflammation and fibrosis. Prior studies demonstrate that inhibition of inhibitor of κB kinase (IKK)-mediated NF-κB activation using l-isomer NF-κB essential modulator (NEMO)-binding domain (NBD) peptide-based approaches reduce muscle pathology in the mdx mouse. For our studies, the NBD peptide is synthesized as a fusion peptide with an eight-lysine (8K) protein transduction domain to facilitate intracellular delivery. We hypothesized that the d-isoform peptide could have a greater effect than the naturally occurring l-isoform peptide due to the longer persistence of the d-isoform peptide in vivo. In this study, we compared systemic treatment with low (1 mg/kg) and high (10 mg/kg) doses of l- and d-isomer 8K-wild-type-NBD peptide in mdx mice. Treatment with both l- or d-isoform 8K-wild-type-NBD peptide resulted in decreased activation of NF-κB and improved histology in skeletal muscle of the mdx mouse. However, we observed kidney toxicity (characterized by proteinuria), increased serum creatinine, activation of NF-κB and pathological changes in kidney cortex that were most severe with treatment with the d-isoform of 8K-wild-type-NBD peptide. The observed toxicity was also seen in normal mice.
Similar content being viewed by others
Introduction
Duchenne muscular dystrophy (DMD) is a genetic form of muscle degeneration caused by the absence of the 427 kDa cytoskeletal protein dystrophin (1,2). Clinically, patients with DMD are confined to a wheelchair for mobility by their early teen years and succumb to the disease by their second or third decade of life, usually due to cardiorespiratory failure (3). The only currently recommended pharmaceutical treatment to slow muscle degeneration in DMD is glucocorticoids that inhibit inflammation and promote muscle protein synthesis (4–6), which leaves a clear need for further therapy development for DMD. Dystrophin localizes to the cytoplasmic face of the sarcolemma (i) to provide a structural link between intracellular F-actin and extracellular laminin through the dystrophinassociated protein complex (DAPC) (7,8), and (ii) to bind cellular signaling molecules such as nitric oxide synthase (9,10). In the absence of dystrophin, the DAPC is lost, leading to membrane instability, inflammation, degeneration of muscle fibers and eventual necrosis and replacement of muscle fibers with connective and adipose tissue (11).
The absence of the dystrophin protein in the muscle of patients with DMD and in the mdx mouse leads to the activation of pathogenic signaling pathways in striated muscle tissue. Central among mechanisms of chronic inflammation is the activation of the transcription factor nuclear factor-κB (NF-κB). Elevated levels of NF-κB are observed in dystrophic tissues (12–17), resulting in upregulation of proinflammatory cytokines (18–21).
NF-κB is composed of subunit dimers sequestered in the cytoplasm by the inhibitor protein, IκB. In the classical pathway of NF-κB activation, the inhibitor of κB kinase (IKK) complex phosphorylates the IκB inhibitor protein, leading to its ubiquitination and degradation. The nuclear localization signal of the NF-κB dimer is unmasked and, once free from the IκB inhibitor protein and the NF-κB dimer, it rapidly translocates to the nucleus of the cell and activates proinflammatory cytokine expression (21,22).
The demonstration of proof-of-principle that inhibition of the classical pathway of NF-κB could provide therapeutic benefit in patients with DMD was achieved by showing improved dystrophic muscle histopathology in dystrophin-deficient mdx mice haploinsufficient for the NF-κB p65 subunit compared with mdx control animals (12). Toward clinical translation, peptide-mediated treatments were developed to inhibit NF-κB activation by interfering with the formation of the IKK complex. The IKK complex consists of α and β catalytic subunits that are bound by a regulatory γ subunit, also called the NF-κB essential modulator (NEMO) (23). The NEMO-binding domain (NBD) peptide consists of the protein-binding domain of the IKKβ subunit for the IKKγ subunit of the IKK complex. Once bound, the NBD peptide prevents association of the IKK complex, inhibiting the catalytic activity required for the phosphorylation of the IκB inhibitor protein, thus inhibiting NF-κB activation (24).
In previous studies in the mdx mouse, systemic administration of the NBD peptide fused to a protein transduction domain (PTD) peptide comprised of 8K residues showed improvement in limb and diaphragm skeletal muscle pathology and function (12,17,25). To date, only l-isoform peptides have been tested in the muscular dystrophy model. We hypothesized that d-isoform peptides would have greater therapeutic potential due to their longer bioavailability in vivo (26–29). We therefore directly compared an all-l-isoform 8K-NBD peptide with an all-d-isoform 8K-NBD peptide. Despite pathological improvements in dystrophic muscle with d-8K-wild-type-NBD peptide, kidney toxicity was observed.
Materials and Methods
PTD-NBD Peptides and Mice
Peptides containing the 8K PTD peptide fused to either a wild type or mutated NBD peptide were synthesized at the Peptide Synthesis Facility (University of Pittsburgh, Pittsburgh, PA, USA). Both l- and d-isoforms of the 8K-wild-type-NBD peptide that were used for this study had the amino acid sequence: KKKKKKKK-GG-TALDASALQTE, with the PTD bridged to the NBD peptide with a diglycine spacer. For both l- and d-isoforms of the 8K-mutant-NBD peptides, two tryptophan amino acids (underlined) were substituted for two of the alanine residues in the NBD portion of the 8K-NBD peptide: KKKKKKKK-GG-TALDWSWLQTE. Lyophilized peptide stocks were resuspended in sterile, distilled water to a concentration of 40 mmol/L.
Mice were purchased from The Jackson Laboratory (Bar Harbor, ME, USA) and housed in a pathogen-free room within the Biomedical Science Tower-South Animal Facility at the University of Pittsburgh with food and water provided ad libitum. l- or d-8K-wild-type-NBD peptides were administered in vivo to male or female dystrophic, C57BL/10ScSn-Dmdmdx/J (mdx) or normal, C57BL/6J (C57) mice, beginning at 28 d of age and continuing for 4 wks with treatments of three intraperitoneal (i.p.) injections per week (Monday, Wednesday and Friday) at either a peptide to body weight dosage of 1 mg/kg (low dose) or 10 mg/kg (high dose). The l- or d-8K-mutant-NBD peptides were administered to mdx or C57 mice at a dose of 10 mg/kg. Age-matched untreated or saline-treated mdx and C57 mice were used as controls. Urine samples were collected at multiple intervals during the studies. Following 4 wks of saline or 8K-NBD peptide treatments, mice were euthanized to collect muscles, kidneys and blood. The quadriceps muscle was used for these studies. All animal studies were approved by the University of Pittsburgh Institutional Animal Care and Use Committee (IACUC).
Electrophoretic Mobility Shift Assay
Electrophoretic mobility shift assays (EMSA) were performed as described previously (17). For quadriceps muscles, a 25 to 30 mg frozen piece of tissue was pulverized in liquid nitrogen by mortar and pestle. For kidneys, a 20-mg section of kidney cortex was processed in the same manner as muscle. Nuclear protein was extracted using the NE-PER Nuclear and Cytoplasmic Extraction Reagents (Fisher Scientific) and multiple dilutions in duplicate were assayed for protein content using the BCA Protein Assay Kit (Fisher Scientific). Nuclear extracts of quadriceps muscle (30 µg) or kidney cortex (10 µg) were incubated with 5× Gel Shift Buffer (Promega), followed by incubation with an α-32P-deoxycytodine triphosphate (32P-dCTP)-radiolabeled, double-stranded DNA probe containing the NF-κB binding sequence) (32P-dCTP, MP Biomedicals). For the NF-κB probe, two oligonucleotides were annealed and the overhang was filled in with 32P-dCTP using Klenow fragment (Life Technologies), as described previously (30). Samples were electrophoresed on a nondenaturing, 6% polyacrylamide gel at 300 V for approximately 90 min. Densitometry of shifted-NF-κB bands were analyzed using ImageJ (NIH) software. Probe sequences for both oligonucleotides, with the NF-κB binding sequence underlined, are: NF-κB Oligo#1: 5′-CAGGGCTGGG GATTCCCCATCTCCACAGTTTCACT TC-3′; NF-κB Oligo#2: 5′-GAAGTGAAAC TGTGG-3′ (IDT, Inc.).
Kidney Analysis
Kidneys were harvested from untreated age-matched, saline-treated and l- and d-8K-wild-type-NBD peptide- and l- and d-8K-mutant-NBD peptide-treated mdx and C57 mice following 4 wks of treatment. Kidneys were washed in 1× PBS and digitally imaged. Following imaging, kidneys were processed for multiple applications, including: (1) bright-field histology, (2) transmission electron microscopy (TEM) and (3) nuclear extraction and detection of NF-κB activation by EMSA.
Urinalysis by SDS-PAGE
Urine samples were collected from age-matched untreated, saline-treated and l- and d-8K-wild-type-NBD peptide-and l- and d-8K-mutant-NBD peptidetreated mdx and C57 mice at multiple time points during the peptide injection regimen as specified in the Results section. Urine samples were stored at −80°C until analysis. A 7.5 µL urine sample from each animal at specific time points in the study was electrophoresed on a 4% stacking/10% resolving SDS-PAGE gel, followed by whole-gel protein staining using Coomassie Blue gel staining reagent (45% methanol, 10% glacial acetic acid, 0.25% Coomassie Blue R-250). Coomassie Blue-stained gels were imaged on an Odyssey CLx Infrared Imaging System, utilizing the 700-nm channel (LI-COR Biosciences). The albumin band was confirmed by immunoblotting with a 1:1000 diluted goat anti-mouse albumin antibody (Bethyl Laboratories Inc.), followed by a 1:30,000 diluted IRDye 800CW goat anti-mouse IgG (H + L) conjugated secondary antibody (LI-COR Biosciences). Urine protein bands were either quantified by densitometry using ImageJ software or individual protein bands were counted in each gel lane to compare levels of urinary protein excretion.
Serum Creatinine Analysis
Blood samples were harvested from mdx and C57 mice treated with saline, l- and d-8K-wild-type-NBD peptides or l- and d-8K-mutant-NBD peptides, via cardiac puncture immediately following euthanization. Following a clotting step, blood samples were centrifuged at 8,000g to harvest serum for biochemical analysis. Serum samples from salinetreated and l- and d-8K-wild-type-NBD peptide- and l- and d-8K-mutant-NBD peptide-treated mdx and C57 mice were analyzed using the Creatinine (serum) Colorimetric Assay Kit (Cayman Chemical), according to the manufacturer’s instructions.
Bright-Field Histology
For bright-field histological analysis of skeletal muscle tissue, 10-µm cryosections of quadriceps tissues were stained either with hematoxylin and eosin (H&E) to observe morphological characteristics or with an Alexa Fluor 488 anti-mouse IgG antibody to assess levels of necrosis or with embryonic myosin heavy chain (eMyHC) to measure levels of regenerating muscle tissue as described previously (17). For bright-field histological analysis of the kidney, one half of one kidney was stored in 10% buffered formalin, paraffin embedded and sectioned at 3 to 4 µm. Sections were stained with H&E and periodic acid-Schiff (PAS) and Masson trichrome. All kidney histology was performed by the UPMC Presbyterian Hospital Pathology Department Histology Laboratory (Pittsburgh, PA, USA). Images were taken at 200× magnification.
Transmission Electron Microscopy
For electron microscopy studies, 1-mm3 cubes of tissue were excised from the kidney cortex of saline-treated and l- and d-8K-wild-type-NBD peptide- and l- and d-8K-mutant-NBD peptide-treated mdx mice and stored in Karnovsky fixative (2.5% gluteraldehyde, 2% paraformaldehyde in cacodylate buffer) and postfixed in 1% osmium tetroxide. The tissue was dehydrated through a series of ethanol changes, soaked in propylene oxide, then embedded in Epon plastic resin and cured overnight at 60° C. Thick sections (1 µm) were cut with a diamond knife using a Reichert Ultracut S ultramicrotome, stained with toluidine blue and imaged at 400× magnification. One plastic block was selected for thin sectioning. The plastic block was trimmed with a razor blade and thin sectioned using a diamond knife, cutting sections at 85-nm thickness. The sections were stained with uranyl acetate and lead citrate, and examined under a Philips 208 transmission electron microscope, and imaged at 60 kV. Digital images were captured by an AMT digital camera. For electron microscopy, representative images, taken at multiple magnifications (2200×, 2800×, 5600×), were utilized to observe any potential ultrastructural abnormalities in kidney cortex as a result of 8K-NBD peptide-mediated therapy upon comparison with saline-treated controls. All electron microscopy was performed by the UPMC Presbyterian Hospital Pathology Department Electron Microscopy Laboratory (Pittsburgh, PA).
Statistics
For statistical comparison, a one-way analysis of variance (ANOVA) was utilized. All data is presented as values ± standard error of the mean (s.e.m.). Statistical significance was specified for p < 0.05. The number of animals for each analysis is noted in each figure.
All supplementary materials are available online at https://doi.org/www.molmed.org .
Results
l- and d-8K-Wild-type-NBD Peptide-Mediated Therapy Reduced NF-κB Activation in Muscle Cells in mdx Limb Muscle In Vivo
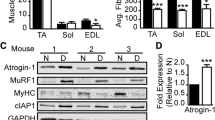
Examination by EMSA of nuclear extracts from quadriceps muscles of mdx mice treated with high-dose l- and d-8K-wild-type-NBD peptides showed decreased activation of the classical NF-κB signaling pathway. In contrast, treatment with l- and d-8K-mutant-NBD peptides or saline did not decrease pathological activation of NF-κB (Figure 1A). We performed densitometric analysis of low-and high-dose l- and d-8K-wild-type-NBD peptide-treated mdx mice, compared with untreated age-matched controls and observed that NF-κB activation was significantly reduced in mdx mice treated with the l-8K-wild-type-NBD peptide at low dose (n = 9; 29.2%; p = 0.019) and high dose (n = 8; 32.3%; p < 0.001) and in mdx mice treated with d-8K-wild-type-NBD peptide at low dose (n = 7; 27.3%; p = 0.013) and high dose (n = 7; 35.4%; p < 0.001).
EMSA analysis of NF-κB activation and immunohistochemical analysis of 8K-NBD peptide-treated mdx mice in vivo. Representative results of EMSA determination of levels of NF-κB activation in nuclear extracts from quadriceps muscles of mdx mice treated with 8K-NBD peptides in vivo are shown (A). Histochemical staining (H&E; left panels) and immunohistochemical analysis of necrosis (mouse IgG; middle panels) and regeneration (embryonic myosin heavy chain; right panels) of 10 µm sections of quadriceps muscle tissue from mdx mice treated with saline (B–D), d-8K-wild-type-NBD peptide (E–G) and d-8K-mutant-NBD peptide (H–J). wt, Wild type; mut, mutant. Scale bar, 100 µm.
Treatment with d-8K-Wild-type-NBD Peptides Improved Skeletal Muscle Histopathology of mdx Mice Similar to Treatment with l-8K-Wild-type-NBD Peptides
Quadriceps muscle showed decreased necrosis and increased regeneration in mdx mice that were treated with 4 wks of high-dose d-8K-wild-type-NBD peptide therapy in comparison to mdx mice that were treated with either d-8K-mutant-NBD peptide or saline control (Figures 1B–J). In a quantitative study comparing 4 wks of treatment of mdx mice (n = 8 mice per group) with either d- or l-isoform 8K-NBD peptide at low dose or high dose, the following results were obtained in comparison with untreated mdx mice collected in parallel. The average reduction in area of necrosis observed with d-8K-NBD peptide treatment was 32.7% for low dose and 55.0% for high dose. In comparison, l-8K-NBD peptide treatment reduced the area of necrosis by 50.5% for low dose and 39.6% for high dose. Treatment with d-8K-NBD peptide therapy resulted in an increased level of regeneration of 153.3% (p = 0.041) for low dose and 24.4% (not significant) for high dose. In comparison, l-8K-NBD peptide therapy resulted in an increased level of regeneration of 120.0% (p = 0.046) for low dose and 77.8% (not significant) for high dose.
Treatment with d-8K-Wild-type-NBD Peptide Caused Gross Pathological Changes to Kidney
All mdx and C57 mice treated with high-dose d-8K-wild-type-NBD peptide had gross alterations in kidney structure showing lighter color compared with control kidneys and some appeared enlarged, with variation in coloring and formation of cysts (Figure 2 and Supplementary Figure 1). Kidneys from highdose d-8K-mutant-NBD peptide-treated mice were lighter in color than controls, but appeared less abnormal grossly than kidneys harvested from high-dose d-8K-wild-type-NBD peptide-treated mice. Kidneys harvested from mdx and C57 mice treated with low- and high-dose l-8K-wild-type-NBD, high-dose l-8K-mutant-NBD (low-dose l-8K-mutant-NBD peptide not tested), or low-dose d-8K-wild-type-NBD appeared normal without gross abnormalities (Figure 2 and Supplementary Figure 1). Gross examination of spleen and liver tissues from l- or d-8K-wild-type-NBD or l- and d-8K-mutant-NBD peptide-treated mdx mice appeared normal with no differences compared with controls (data not shown).
Kidney toxicity in mdx mice following treatment with 8K-NBD peptides. Kidneys were harvested from mdx mice treated for 4 wks with 10 mg/kg of l- and d-isomers of 8K-wild-type-NBD and 8K-mutant-NBD peptides. Representative whole-organ images of right and left (R/L) kidneys are shown from two representative mice from each treatment group. Nuclear extracts from isolated kidney cortex were assayed for levels of NF-κB activation by EMSA; representative images are shown in the far right panels. wt, Wild type; mut, mutant.
Treatment with d-8K-Wild-type-NBD Peptide Activated NF-κB in the Kidney Cortex
EMSA analysis of nuclear extracts of the kidney cortex from mdx or C57 mice treated with d-8K-wild-type-NBD peptide had increased levels of NF-κB activation (Figure 2 and Supplementary Figure 1). NF-κB activation remained at normal levels or was mildly elevated in the kidney cortex of l-8K-wild-type-NBD or l- or d-8K-mutant-NBD peptide-treated mdx (Figure 2) or C57 (Supplementary Figure 1) mice compared with saline-treated controls.
l- and d-8K-Wild-type-NBD Peptide-Mediated Therapy Induced Proteinuria
Baseline levels of urine protein from untreated, age-matched mdx mice were low (Figures 3A, B). At both early (after 1 wk of treatment) and late (after 4 wks of treatment) urine collection time points, we observed increased urine protein levels associated with 8K-wild-type-NBD peptide-mediated therapy (Figures 3A, B). At the early time point, urine samples from l-8K-wild-type-NBD peptide-treated mdx mice had a 2.5-fold increase at low dose and a 7.5-fold (p = 0.045) increase at high dose in the density of the 68-kDa albumin band compared with untreated mdx mice. At the late time point, urine samples from l-8K-wild-type-NBD peptide-treated mdx mice had a 1.4-fold increase at low dose and a 2.0-fold increase at high dose compared with untreated mdx mice. At the early time point for d-8K-wild-type-NBD peptide-treated mdx mice, urine samples had an increase in albumin of 3.4-fold at low dose and of 16.3-fold (p < 0.001) at high dose over control mdx mice. At the late time point, urine samples from d-8K-wild-type-NBD peptide-treated mdx mice had an increase in albumin of 1.9-fold at low dose and of 4.9-fold at high dose over untreated mdx mice (Figure 3B). Additionally, we found significantly lower levels of albuminuria at the late time point compared with the early time point collection in the high-dose, d-8K-wild-type-NBD peptide treatment group by SDS-PAGE gel-based urinalysis (p = 0.025) (Figure 3B). Specific analysis of albumin levels in urine samples by enzyme-linked immunosorbent assay (ELISA) (data not shown) confirmed elevated levels of albumin in l- and d-isomer 8K-wild-type-NBD peptide-treated mdx mice in early and late urine collections, which correlated with the SDS-PAGE gel-based urinalysis assay shown. We also quantified the total number of protein bands observed by gel electrophoresis of urine samples (Figure 3C). The high-dose d-8K-wild-type-NBD peptide-treated mdx mice had a significantly increased number of protein bands, which was greater than the number of protein bands observed for low-dose d-8K-wild-type-NBD peptide or either low- or highdose l-8K-wild-type-NBD peptide (Figure 3C). To further analyze the effect of high-dose d-8K-wild-type-NBD peptide-induced proteinuria during the first week of 8K-NBD peptide-mediated therapy for mdx mice, urine was collected before, 30 min after and 24 h after each of the first 3 d-8K-wild-type-NBD peptide injections. Mice injected with 1, 2 or 3 peptide injections revealed increased urine protein 30 min and 24 h after the first injection of peptide and this proteinuria was further increased and remained persistently present after the second and third d-8K-wild-type-NBD peptide injections (Figure 3D). Additionally, the pattern of 8K-NBD peptide-induced proteinuria was similar in dystrophic mdx and normal C57 mice; the d-8K-wild-type-NBD peptide caused the highest levels of proteinuria in both mouse strains (Supplementary Figures 2A-B).
Urinalysis from untreated and 8K-NBD peptide-treated mdx mice at multiple time points. Urine samples (7.5 µL) were electrophoresed on a 10% resolving SDS-PAGE gel followed by visualization of separated proteins by Coomassie Blue R-250 staining. Representative urine samples collected after 1 wk of treatment (early urinalysis) and after 4 wks of treatment (final urinalysis) are shown in (A). Immunoblotting for albumin in mouse urine using an anti-mouse albumin antibody is shown in the far right lane of (A), confirming presence of the 68-kDa albumin protein in urine. Densitometric measurements of the 68-kDa albumin band present in all urine samples (see arrow in (A)) is shown in (B) as average band density ± standard error. In (B), an asterisk (*) indicates a significant difference between early urinalysis groups compared with untreated mdx (white bars); two asterisks (**) indicate a significant difference between late urinalysis groups compared with untreated mdx mice (black bars) and § indicates a significant difference between early and late treatment samples in specified treatment groups (p < 0.05). To represent relative amounts and timing of proteinuria in 8K-NBD peptide-treated mdx mice, the total number of protein bands after SDS-PAGE electrophoresis of urine samples from each mouse in the study was quantified and the data is presented as the average number of protein bands present in the gel ± standard error (C). In (C), an asterisk (*) indicates the 8K-NBD peptide treatment group is significantly different than untreated mdx(p < 0.05). In (D), 10 µL urine samples, collected from mdx mice prior to, and 30 min and 24 h after 1, 2 or 3 high-dose, d-8K-wild-type-NBD peptide injections were electrophoresed and stained as in (A) to show early onset of severe proteinuria in this treatment group. Age-matched mdx mice served as the untreated mdx group. n = number of animals per group.
l- and d-8K-Wild-type-NBD Peptide-Mediated Therapy Induced Elevations in Serum Creatinine
In saline-treated mdx and C57 mice, we detected low levels of serum creatinine with 20.8 ± 3.3 µmol/L for mdx and 16.2 ± 3.3 µmol/L for C57 (Figure 4). Elevated levels of serum creatinine were detected in mdx (55.5 ± 19.6 mmol/L) and C57 (44.0 ± 16.4 mmol/L) mice treated with l-8K-wild-type-NBD peptides, while significantly increased serum creatinine levels were detected in mdx (46.3 ± 6.5 µmol/L; p = 0.039) and C57 (71.7 ± 3.3 µmol/L; p = 0.004) mice treated with d-8K-wild-type-NBD peptide. Mdx and C57 mice treated with l- and d-8K-mutant-NBD peptides had slightly elevated serum creatinine compared with saline-treated controls, but the differences were not significant (Figure 4).
Serum creatinine levels in mdx and C57 mice following treatment with 8K-NBD peptides. Serum samples from mice treated for 4 wks with saline or 10 mg/kg of l- or d-isomers of 8K-wild-type-NBD and 8K-mutant-NBD peptides three times weekly were analyzed for levels of creatinine. Data is presented as µmol/L serum creatinine and individual data points, shown by black diamonds, represent each animal analyzed and average data is shown by white diamonds. An asterisk (*) indicates the 8K-NBD peptide treatment group is significantly different than saline-treated mdx group (p < 0.05). Two asterisks (**) indicate the 8K-NBD peptide treatment group is significantly different than saline-treated C57 group (p < 0.05). wt, Wild type; mut, mutant.
d-8K-Wild-type-NBD and d-8K-Mutant-NBD Peptide Treatment Caused Histological Changes in Mouse Kidney Cortex
Normal histology of the kidney cortex was observed in saline-treated mdx mice as determined by histological staining with H&E, PAS and toluidine blue (Figures 5A–C). Additionally, normal morphological characteristics of the kidney cortex were observed in mdx mice treated with high-dose l-8K-wild-type-NBD peptide (Figures 5D–F) and high-dose l-8K-mutant-NBD peptide (Figures 5G–I). Loss of the microvillus brush border of proximal tubules in the kidney cortex was detected by PAS staining of sections of kidney cortex of mdx mice treated with the high-dose d-8K-wild-type-NBD peptide and, to a lesser extent, in kidney cortex of high-dose d-8K-mutant-NBD peptide-treated mice (see black arrows in Figures 5K, N). As demonstrated by H&E staining, mdx mice treated with d-8K-wild-type-NBD, developed nonnecrotic, dilated or “flattened” tubules, interstitial lymphocyte infiltration and a general disorganization of the kidney cortex (Figure 5J). Mice treated with d-8K-mutant-NBD had some dilated vessels, lymphocytes and disorganization of the kidney cortex, but less than observed in the d-8K-wild-type-NBD treatment group (Figure 5M). Large deposits of protein absorption droplets were detected in the proximal tubules of the kidney cortex in mice treated with d-8K-wild-type-NBD and to a lesser extent in mdx mice treated with d-8K-mutant-NBD peptide (see white arrows in Figures 5L, O). Masson trichrome staining did not reveal any regions of fibrosis within the kidney cortex of any mouse in this study (data not shown). We observed histological results in kidney cortex of C57 treated mice that were similar to mdx mice (data not shown).
Bright-field histological analysis of the kidney cortex from mdx mice treated with 8K-NBD peptides. Kidneys were harvested from mice treated for 4 wks with saline or 10 mg/kg of l- or d-isomers of 8K-wild-type-NBD and 8K-mutant-NBD peptides three times weekly. After paraffin-embedding and sectioning at 3 to 4 µm, tissues were stained with H&E (A,D,G,J,M), and periodic acid-Schiff (PAS) (B,E,H,K,N). Plastic sections cut at 1 µm were stained with toluidine blue (C,F,I,L,O). H&E and PAS images are 200× magnification and toluidine blue images are 400× magnification. Black arrows in sections stained with PAS mark the brush border of proximal tubules. White arrows in sections stained with toluidine blue show protein absorption droplets in proximal tubules. Sale bars, 100 µm.
d-8K-Wild-type-NBD and d-8K-Mutant-NBD Peptide Treatment Caused Ultrastructural Changes in the Mouse Kidney Cortex
Kidney cortex samples from saline-treated, high-dose l-8K-wild-type-NBD peptide-treated and high-dose l-8K-mutant-NBD peptide-treated mdx mice appeared normal with no evidence of kidney disease when examined by transmission electron microscopy (Figures 6A–I). Ultrastructural changes in kidneys of mdx mice treated with high-dose d-8K-wild-type-NBD peptide (Figures 6J–L) or d-8K-mutant-NBD peptide (Figures 6M–O) were observed in comparison to saline-treated control animals. Mice treated with high-dose d-8K-wild-type-NBD peptide developed lysosomal inclusions in the proximal tubules of the kidney cortex, as shown by large, electron-dense structures (Figures 6J, K). To a lesser extent, mdx mice treated with high-dose d-8K-mutant-NBD peptide had evidence of lysosomal inclusions in the proximal tubules of the kidney cortex as well (Figures 6M, N). In all treatment groups, glomeruli, mitochondria, red blood cells, podocyte foot processes and regions of the medulla had normal morphology (Figures 6C, F, I, L, O).
Transmission electron microscopy of kidney cortex samples from mdx mice treated with 8K-NBD peptides. Kidneys were harvested from mice treated three times weekly for 4 wks with saline (A-C), or 10 mg/kg of l-8K-wild-type-NBD (D-F), l-8K-mutant-NBD (G-I), d-8K-wild-type-NBD (J-L), or d-8K-mutant-NBD (M-O) peptides and processed for electron microscopy. Left panels (A,D,G,J,M) show a 2200× magnification, middle panels (B,E,H,K,N) show a 5600× magnification and the far right panels (C,F,I,L,O) show a 2800× magnification.
Discussion
The present study explores the efficacy and toxicity of a novel systemic therapy with NBD peptides synthesized with all-d isoform amino acids in the mdx mouse model of DMD. We confirm that blocking classical NF-κB signaling in dys-trophic muscle tissue of the mdx mouse model by systemic administration of 8K-NBD peptides improves muscle histopathology as shown by a reduction in necrosis and an increase in regeneration of skeletal muscle fibers (12,17,25). We directly compared the l-isoform with the d-isoform of 8K-NBD peptide at two doses. d-isoform peptides have greater resistance to degradation in comparison to peptides comprised of naturally occurring l-isoform amino acids (26–29). In this study, we showed that the pathological activation of NF-κB signaling in mdx mouse skeletal muscle is reduced by either low- or high-dose 8K-NBD peptide composed of either l- or d-isoform amino acids. Our observation of gross kidney pathology and proteinuria with d-8K-wild-type-NBD peptide treatment led us to perform additional studies with l- and d-isomer mutant NBD peptides. The d-isomer, wild-type-NBD peptide treatment appeared to be the most toxic to the kidney with a lower level of toxicity observed with treatment with the d-isomer, mutant NBD peptide. Kidney toxicity ranged from subtle to not observed with treatment with the l-isoform of either 8K-wild-type-NBD peptide or 8K-mutant-NBD peptide. The kidney toxicity in normal C57 mice treated with l- and d-isomers of 8K-wild-type-NBD and 8K-mutant-NBD peptides followed a similar pattern to that observed in mdx mice.
The relationship of necrosis and regeneration in dystrophic skeletal muscle is interdependent and complex. We found enhanced regeneration of muscle fibers in d-isoform 8K-NBD peptide-treated mdx muscle, similar to what was previously published with treatment with l-isoform 8K-NBD peptides (12,17). The decrease in muscle fiber necrosis observed in the setting of enhanced regeneration in either d- or l-isoform 8K-NBD peptide-treated mdx muscle suggests that 8K-NBD treatment directly enhances muscle fiber regeneration.
Peptide treatment regimens of three injections per week beginning at approximately 4 wks of age and continuing for 4 wks were assessed in this study to coincide with the most active phase of muscle degeneration and regeneration in hind limb skeletal muscle of the mdx mouse (31). Interestingly, it was recently shown that inhibition of TNF receptorassociated factor 6 (TRAF6), an upstream NF-κB pathway molecule, improved mdx histopathology in young mice, however, mice with long-term inhibition of TRAF6 developed necrosis and fibrosis in muscle (32). Since none of our studies exceed 7 wks of treatment with NBD peptides, we have not tested the effect of long-term NBD peptide treatment in mdx mice.
While previous PTD-NBD peptide studies have focused on the ability of the NBD peptide to block NF-κB activation and improve dystrophic muscle histopathology in skeletal muscle, this is the first study to address potential renal toxicity of NBD peptide-mediated therapy. Previous in vivo studies of the biodistribution of l-isoform PTD-peptides show localization to kidneys 8 h after intraperitoneal injection (33) and studies examining d-isoform PTD-peptides in vivo revealed high levels of transduction in the kidney beginning at 1 h after systemic administration, with levels still detected at 24-h postinjection (34).
In the present study, we observed gross structural alteration of kidneys in both mdx and C57 mice following treatment with high dose of d-8K-wild-type-NBD peptide and, to a lesser extent, d-8K-mutant-NBD peptide. Microscopic examination of PAS-stained kidney cortex regions from high-dose d-8K-wild-type-NBD peptide-treated mice revealed damage to the microvillus brush border of many proximal tubules. In the highdose d-8K-mutant-NBD peptide-treated mice, we only observed a few disruptions of the microvillus brush border. H&E-stained sections revealed a general disorganization of the kidney cortex in mice treated with d-8K-wild-type-NBD and d-8K-mutant-NBD peptides, with d-8K-wild-type-NBD peptide-treated mice exhibiting greater disorganization, in addition to dilated tubules and interstitial lymphocyte infiltration. Ultrastructural analysis of the kidney cortex from d-8K-wild-type-NBD peptide and d-8K-mutant-NBD peptide-treated mdx mice revealed lysosomal inclusions in proximal tubules, while examination of glomeruli, red blood cells, mitochondria, capillaries and podocytes appeared unaffected. Comparison of the levels of observed toxicity in mice treated with d-8K-wild-type-NBD peptide and the d-8K-mutant-NBD peptide, suggests that contributions to renal toxicity can be attributed to both the d-isoform nature of the peptides and the wild-type NF-κB inhibitory peptide sequence.
Nuclear extracts of isolated kidney cortex tissue were analyzed by EMSA to assess activation of the classical NF-κB signaling pathway. In contrast to a decrease in the activation of NF-κB signaling that we observed in skeletal muscle of l- and d-8K-wild-type-NBD peptide-treated mice, there was increased activation of NF-κB signaling in kidney cortex of mice treated with d-8K-wild-type-NBD peptide and d-8K-mutant-NBD peptide, but not in mice treated with l-8K-wild-type-NBD peptide, l-8K-mutant-NBD peptide or saline. Previous in vitro studies have shown induction of the NF-κB signaling pathway in proximal tubule epithelial cells in the presence of bovine serum albumin (BSA) (35,36) or human serum albumin (HSA) (37,38), in a dose-dependent manner by EMSA. We detected elevated levels of albumin in urine from d-8K-wild-type-NBD peptide-treated mdx mice in conjunction with increases in NF-κB activation in nuclear extracts of kidney cortex. These results suggest that the kidney toxicity observed in d-8K-wild-type-NBD peptide-treated mdx mice may lead to proteinuria, which then activates the classical NF-κB signaling pathway in kidney tissue. Since the wild-type NBD peptide would be expected to block this activation, one can speculate that increases in NF-κB signaling would be even more prominent if the peptide causing renal toxicity did not include the NBD sequence. However, after examination of mice treated with d-8K-mutant-NBD peptide, there was a much lower level of kidney toxicity detected, in comparison to mice treated with d-8K-wild-type-NBD peptide. Therefore, it appears that the wild-type NBD peptide sequence significantly contributes to the pathogenic potential of the therapy.
Conclusion
We postulate that the kidney toxicity and increased NF-κB activation in response to the d-8K-wild-type-NBD peptide treatments may have been compounded by the increased half-life of the d-isoform peptide. d-isoform peptides, a non-naturally occurring form, may have accumulated to high levels in the proximal tubules of the kidney cortex of both mdx and C57 mice during treatment. A study examining levels of the amino acid d-serine in rats determined that high levels of d-serine can be nephrotoxic (39). Our 8K-NBD peptide constructs in this study contain a single serine amino acid in the NBD peptidebinding domain. The potential build up to nephrotoxic levels of d-serine in the kidneys of mice receiving a d-isoform peptide may account for a component of the observed toxicity. Additionally, proteinuric renal diseases have been shown to upregulate the NF-κB signaling pathway (40). Protein overload of the proximal tubules leads to the release of cytokines and chemokines that ultimately lead to inflammation and fibrosis of the tubular interstitium (41,42). It is unclear whether the observed proteinuria is glomerular or tubular in origin, however, albuminuria observed in early urinalysis samples of d-8K-wild-type-NBD peptide-treated mice would indicate a glomerular proteinuria. In the late urinalysis samples from the same mice, we no longer observed albuminuria, but rather, we observed a greater number of lower molecular weight proteins present in urine, which is evidence of tubular proteinuria. We postulate that early in the treatment regimen, glomerular damage led to the observed proteinuria/albuminuria of the d-8K-wild-type-NBD peptide and d-8K-mutant-NBD peptidetreated mice. We further suggest that the ultrastructural detection of lysosomal inclusions in the proximal tubules of the d-8K-wild-type-NBD peptide and d-8K-mutant-NBD peptide-treated mice may relate to the observed proteinuria following the full treatment regimen.
The goal of this study was to explore the therapeutic utility of a novel d-isoform of the 8K-NBD peptide whose l-isoform demonstrated efficacy in amelioration of dystrophic myopathy in the mdx mouse model of DMD (12,17,25). While the d-isoform of the 8K-wild-type-NBD peptide provided equivalent ability to decrease NF-κB activation in skeletal muscle compared with the l-isoform, its effects in the kidney revealed toxicity at a level not seen with the l-isoform 8K-wild-type-NBD peptide. Our finding of toxicity in both the mdx muscular dystrophy mouse model and normal mice suggest that future NBD peptide-based studies should focus on strategies other than the use of d-isoform peptides.
Disclosure
The authors take full responsibility for the contents of this manuscript, which do not represent the views of the Department of Veterans Affairs or the U.S. Government.
References
Hoffman EP, Brown RH, Kunkel LM. (1987) Dystrophin: the protein product of the Duchene muscular dystrophy locus. Biotechnology. 24:457–66.
Koenig M, Monaco AP, Kunkel LM. (1988) The complete sequence of dystrophin predicts a rod-shaped cytoskeletal protein. Cell. 53:219–28.
Bushby K, et al. (2010) Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and pharmacological and psychosocial management. Lancet Neurol. 9:77–93.
Angelini C, Peterle E. (2012) Old and new therapeutic developments in steroid treatment in Duchenne muscular dystrophy. Acta Myol. 31:9–15.
Biggar WD, Gingras M, Fehlings DL, Harris VA, Steele CA. (2001) Deflazacort treatment of Duchenne muscular dystrophy. J. Pediatr. 138:45–50.
Drachman DB, Toyka KV, Myer E. (1974) Prednisone in Duchenne muscular dystrophy. Lancet. 2:1409–12.
Ervasti JM, Campbell KP. (1991) Membrane organization of the dystrophin-glycoprotein complex. Cell. 66:1121–31.
Ervasti JM, Campbell KP. (1993) A role for the dystrophin-glycoprotein complex as a transmembrane linker between laminin and actin. J. Cell Biol. 122:809–23.
Brenman JE, Chao DS, Xia H, Aldape K, Bredt DS. (1995) Nitric oxide synthase complexed with dystrophin and absent from skeletal muscle sarcolemma in Duchenne muscular dystrophy. Cell. 82:743–52.
Lai Y, et al. (2009) Dystrophins carrying spectrinlike repeats 16 and 17 anchor nNOS to the sarcolemma and enhance exercise performance in a mouse model of muscular dystrophy. J. Clin. Invest. 119:624–35.
Ervasti JM, Campbell KP. (1993) Dystrophin-associated glycoproteins: their possible roles in the pathogenesis of Duchenne muscular dystrophy. Mol. Cell. Biol. Hum Dis Ser. 3:139–66.
Acharyya S, et al. (2007) Interplay of IKK/NF-kappaB signaling in macrophages and myofibers promotes muscle degeneration in Duchenne muscular dystrophy. J. Clin. Invest. 117:889–901.
Kumar A, Boriek AM. (2003) Mechanical stress activates the nuclear factor-kappaB pathway in skeletal muscle fibers: a possible role in Duchenne muscular dystrophy. FASEB J. 17:386–96.
Messina S, et al. (2006) Lipid peroxidation inhibition blunts nuclear factor-kappaB activation, reduces skeletal muscle degeneration, and enhances muscle function in mdx mice. Am. J. Pathol. 168:918–26.
Messina S, et al. (2006) Nuclear factor kappa-B blockade reduces skeletal muscle degeneration and enhances muscle function in Mdx mice. Exp. Neurol. 198:234–41.
Monici MC, Aguennouz M, Mazzeo A, Messina C, Vita G. (2003) Activation of nuclear factor-kappaB in inflammatory myopathies and Duchenne muscular dystrophy. Neurology. 60:993–7.
Reay DP, et al. (2011) Systemic delivery of NEMO binding domain/IKKgamma inhibitory peptide to young mdx mice improves dystrophic skeletal muscle histopathology. Neurobiol. Dis. 43:598–608.
Abdel-Salam E, Abdel-Meguid I, Korraa SS. (2009) Markers of degeneration and regeneration in Duchenne muscular dystrophy. Acta Myol. 28:94–100.
De PL, et al. (2012) Increased muscle expression of interleukin-17 in Duchenne muscular dystrophy. Neurology. 78:1309–14.
Messina S, et al. (2011) Activation of NF-kappaB pathway in Duchenne muscular dystrophy: relation to age. Acta Myol. 30:16–23.
Pahl HL. (1999) Activators and target genes of Rel/NF-kappaB transcription factors. Oncogene. 18:6853–66.
Gilmore TD. (2006) Introduction to NF-kappaB: players, pathways, perspectives. Oncogene. 25:6680–4.
May MJ, Marienfeld RB, Ghosh S. (2002) Characterization of the Ikappa B-kinase NEMO binding domain. J. Biol. Chem. 277:45992–6000.
May MJ, et al. (2000) Selective inhibition of NF-kappaB activation by a peptide that blocks the interaction of NEMO with the IkappaB kinase complex. Science. 289:1550–4.
Peterson JM, et al. (2011) Peptide-based inhibition of NF-kappaB rescues diaphragm muscle contractile dysfunction in a murine model of Duchenne muscular dystrophy. Mol. Med. 17:508–15.
Bessalle R, Kapitkovsky A, Gorea A, Shalit I, Fridkin M. (1990) All-D-magainin: chirality, antimicrobial activity and proteolytic resistance. FEBS Lett. 274:151–5.
Hamamoto K, Kida Y, Zhang Y, Shimizu T, Kuwano K. (2002) Antimicrobial activity and stability to proteolysis of small linear cationic peptides with D-amino acid substitutions. Microbiol. Immunol. 46:741–9.
Hong SY, Oh JE, Lee KH. (1999) Effect of D-amino acid substitution on the stability, the secondary structure, and the activity of membraneactive peptide. Biochem. Pharmacol. 58:1775–80.
Tugyi R, et al. (2005) Partial D-amino acid substitution: Improved enzymatic stability and preserved Ab recognition of a MUC2 epitope peptide. Proc. Natl. Acad. Sci. U. S. A. 102:413–8.
Guttridge DC, Albanese C, Reuther JY, Pestell RG, Baldwin AS Jr. (1999) NF-kappaB controls cell growth and differentiation through transcriptional regulation of cyclin D1. Mol. Cell. Biol. 19:5785–99.
De LA, Pierno S, Liantonio A, Conte CD. (2002) Pre-clinical trials in Duchenne dystrophy: what animal models can tell us about potential drug effectiveness. Neuromuscul. Disord. 12 Suppl 1:S142–6.
Hindi SM, Sato S, Choi Y, Kumar A. (2014) Distinct roles of TRAF6 at early and late stages of muscle pathology in the mdx model of Duchenne muscular dystrophy. Hum. Mol. Genet. 23:1492–505.
Schwarze SR, Ho A, Vocero-Akbani A, Dowdy SF. (1999) In vivo protein transduction: delivery of a biologically active protein into the mouse. Science. 285:1569–72.
Pujals S, Sabido E, Tarrago T, Giralt E. (2007) All-D proline-rich cell-penetrating peptides: a preliminary in vivo internalization study. Biochem. Soc. Trans. 35:794–6.
Wang Y, Rangan GK, Tay YC, Wang Y, Harris DC. (1999) Induction of monocyte chemoattractant protein-1 by albumin is mediated by nuclear factor kappaB in proximal tubule cells. J. Am. Soc. Nephrol. 10:1204–13.
Zoja C, et al. (1998) Protein overload stimulates RANTES production by proximal tubular cells depending on NF-kappa B activation. Kidney Int. 53:1608–15.
Morigi M, et al. (2002) Protein overload-induced NF-kappaB activation in proximal tubular cells requires H(2)O(2) through a PKC-dependent pathway. J. Am. Soc. Nephrol. 13:1179–89.
Tang S, et al. (2003) Albumin stimulates interleukin-8 expression in proximal tubular epithelial cells in vitro and in vivo. J. Clin. Invest. 111:515–27.
Krug AW, Volker K, Dantzler WH, Silbernagl S. (2007) Why is D-serine nephrotoxic and alphaaminoisobutyric acid protective? Am. J. Physiol Renal Physiol. 293: F382–90.
Sanz AB, et al. (2010) NF-kappaB in renal inflammation. J. Am. Soc. Nephrol. 21:1254–62.
Zoja C, Benigni A, Remuzzi G. (1999) Protein overload activates proximal tubular cells to release vasoactive and inflammatory mediators. Exp Nephrol. 7:420–428.
Zoja C, Morigi M, Remuzzi G. (2003) Proteinuria and phenotypic change of proximal tubular cells. J. Am. Soc. Nephrol. 14 Suppl 1:S36–41.
Acknowledgments
This work was supported in part by by the Kidney Imaging Core of the Pittsburgh Center for Kidney Research (NIH grant P30-DK079307). In addition, some of the transmission electron microscopy equipment used in this study was funded by grant # 1S10RR019003-01. The work was funded by the Department of Veterans Affairs (VA) Medical Center Merit Review Grant and departmental funds (PRC). We would like to thank Katie Clark and the UPMC Presbyterian Hospital Pathology Department Electron Microscopy Laboratory for their contributions to this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, and provide a link to the Creative Commons license. You do not have permission under this license to share adapted material derived from this article or parts of it.
The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this license, visit (https://doi.org/creativecommons.org/licenses/by-nc-nd/4.0/)
About this article
Cite this article
Reay, D.P., Bastacky, S.I., Wack, K.E. et al. d-Amino Acid Substitution of Peptide-Mediated NF-κB Suppression in mdx Mice Preserves Therapeutic Benefit in Skeletal Muscle, but Causes Kidney Toxicity. Mol Med 21, 442–452 (2015). https://doi.org/10.2119/molmed.2013.00141
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.2119/molmed.2013.00141