Abstract
Applications of polyurethanes (PUs) depend on several physicochemical factors due to the presence of varied monomers involving several ratios. The present study aimed to synthesize various chitosan/heparin-inserted PUs to examine the addition effect on the mechanical and biological properties of the PU-based polymeric material. The PUs were synthesized from unmodified castor oil and isophorone diisocyanate, including chitosan and heparin as fillers. The FTIR, thermal, and mechanical characterization of materials with and without fillers exhibited properties that can be considered within the accepted values. In addition, considering the non-cytotoxicity and antibacterial activity, these synthesized polymers can be exploited as biomaterials. The results also showed that these PUs offer a competitive advantage over other materials since the observed good mechanical and biological properties were found to be within the optimal range for the biomaterial design to myocardial or vascular tissue engineering.
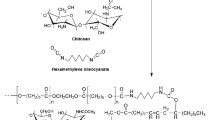
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many studies on vascular grafts have been conducted in the past few decades as a possible approach to redeveloping different biomedical devices [1]. Vascular implants must have specific properties such as high breakage resistance and flexibility. It is also important to have high biocompatibility between the implant and the surrounding tissue. Some problems presented by grafts or vascular implants are low compatibility with the tissues or blood flow alteration leading to adverse cellular responses and generating unwanted inflammation [2]. In addition, thrombus formation, hyperplasia, and thrombogenesis are other failure causes of vascular grafts [3]. For this reason, current materials are designed to improve the adhesion, proliferation, and phenotype preservation of endothelial cells in vascular implants [4]. Therefore, various materials are studied to be employed as vascular grafts, e.g., replacing large-diameter arteries using polytetrafluoroethylene, polyurethane, and polyethylene terephthalate [1, 5]. These polymers have been used for vascular grafts due to their good mechanical properties, durability, and convenient production [6]. However, these polymers have some disadvantages, such as the high susceptibility to generate thrombosis, neointimal hyperplasia, and infection [7]. Materials such as polylactic acid, polycaprolactone, and poly(lactic-co-glycolic acid), are also used as biomaterials for vascular grafts, but they lack elasticity and do not recover after deformation [5].
Polyurethanes (PUs) are well-known to be characterized by being biocompatible [8]. For this reason, they are used in biomedical applications as materials for treating cardiovascular diseases, bone and cartilage implants, controlled drug administration, and tissue engineering, among others [9]. The PU properties depend on the monomer type used in the synthesis, such as polyol, diisocyanate, or additives [10]. Polyols possess two or more hydroxyl functional groups [10], while isocyanates are highly reactive compounds with the NCO functional group, constituting the PU’s hard segment [11]. Among the additives used in PU synthesis are catalysts, cross-linkers, and fillers [10]. The starting materials of PUs are mainly derived from fossil feedstock [12]. In this regard, recent-year research has been focused on finding alternatives to petrochemical-derived monomers, mainly due to economic and environmental reasons [13, 14]. Thus, the interest has turned to explore components from plant sources such as their oils. The primary component type of plant oils is triglycerides, which are glycerol esters with three long-chain fatty acids, having variable composition depending on the oil source [15]. This makes them an attractive raw material for synthesizing polymeric materials due to their low toxicity and production and processing costs [16]. Castor (Ricinus communis) oil is a noteworthy raw material among plant oils because of its renewability, low cost, easy availability, non-edibility, and low viscosity [17]. The occurred triglycerides in castor oil are characterized by one, two, or more unsaturations and hydroxyl (or polyol) groups [18], whose most abundant hydroxylated fatty acid is ricinoleic acid (> 70%) [19]. These features add chemical advantages as suitable raw materials to be incorporated directly into the synthesis and modify the mechanical properties of the PU-derived material. [15]
Some studies have focused on varying the PU cross-linking density by adding natural polymers such as alginate, starch, and heparin, among others, to improve their biocompatibility properties [14, 20]. In this regard, various naturally-occurring macromolecules have performed well in wound healing. This fact rationalizes how chitosan (Ch), a natural copolymer derived from chitin, has been used to design biomaterials because it has antibacterial properties and can be used in hemostatic applications [21]. The functional groups of chitosan can even be modified to make them compatible with different biocompatible pharmaceutical molecules [21] since the biomaterial performance is generally affected if it enters contact with blood due to the activation of various reactive mechanisms that can generate serious adverse clinical events. These events include thrombosis and thromboembolic complications due to platelet activation and the coagulation cascade, complement system activation, and inflammation. In this regard, unmodified and modified chitosan-derived materials have exhibited good blood compatibility. [22, 23]
Biomaterial surfaces can be coated with different drug agents to improve blood compatibility and overcome such disadvantages [24]. For instance, heparin, cilostazol, dipyridamole, and acetylsalicylic acid, among others, have been loaded into vascular grafts to prevent blood clot formation [25]. Heparin is a highly sulfated glycosaminoglycan that contains sulfonic, sulfoamino, and carboxyl groups. Heparin (Hep) is a negatively charged polysaccharide that plays a vital role in various biological processes. This additive interacts with various proteins, hydrogels, and nanoparticles and exhibits properties such as anticoagulant activity and antiangiogenic and apoptotic effects. Heparin is also a component of the extracellular matrix of blood vessels and promotes endothelial cell growth in vitro. Therefore, heparin has become a candidate for biomedical applications. [26]
In this context, it is crucial to consider the biomaterial’s mechanical properties to meet the required features to be incorporated as a vascular implant component, despite the loads being typically lower than those used in other biomaterials, such as orthopedic implants [27]. Additionally, it is critical to evaluate biomaterial biocompatibility to protect users from potential biological risks arising from biomaterial implantation. Although PUs are generally biocompatible, as mentioned above, there are still some disadvantages, such as limited cell recognition and, therefore, low levels of cell adhesion and proliferation, thus affecting the natural healing response [28], which encourages to improve the PU features by using structural modifications and additives.
Therefore, there currently are insufficient materials with adequate mechanical and biological properties to design cardiovascular devices. Therefore, novel biocompatible materials for cardiovascular applications are highly required. In recent studies, we have synthesized and investigated the performance and biocompatibility of PUs (prepared with polyols obtained from modified castor oil) without fillers [8] and adding chitosan [29, 30], and both chitosan and polycaprolactone [31], which afforded relevant properties. Hence, as part of our research on developing other materials for biomedical applications, specifically cardiovascular, the present study aims to expand the knowledge on PU-based materials using other fillers. In this respect, we presented the preparation and the mechanical and biological characterization of novel PU-based films obtained from unmodified castor oil and employing different chitosan/heparin ratios as fillers to modify the PU cross-linking density. This characterization was oriented to look for suitable properties and select candidates for future biomedical applications in cardiovascular devices.
Results and discussion
Characterization of castor oil
Castor oil exhibited suitable physicochemical properties to be used as the polyol source for PU synthesis, such as refractive index (477), iodine index (86.1 cg/g), saponification number (178 mg KOH/g), hydroxyl number (163), and insoluble impurities (3.78% maximum) [32]. Additionally, since castor oil is mainly constituted of triglycerides, whose structure consists of a glycerin skeleton linked to three fatty acids through ester bonds, after triglyceride saponification, the FAME conversion leads to their detection by GC/EIMS and the adequate fatty acid composition determination [33]. Each component was identified by comparing the obtained mass spectra (Figure S1) and LRI values with those reported in the literature and the NIST library to provide the chemical composition listed in Table 1.
The most abundant compounds comprised those reported by other authors as the main components of castor oil. The chemical composition reported for castor oil mainly consists of ricinoleic acid, linoleic acid, oleic acid, and other (un)saturated fatty acids [34]. Elango et al. [35] converted castor oil components into the respective FAMEs to identify the main compounds employing GC/MS, which coincided with our results of this fatty acid-based characterization. Thus, ricinoleic, 8-hydroxyricinoleic, linolenic, and palmitic acids were identified as the main components in the test castor oil, comprising 95.2% abundance. In this sense, castor oil was characterized by a high abundance of ricinoleic acid (67%) and a hydroxylated derivative, i.e., 8-hydroxyricinoleic acid (23.3%) (Table 2). Ricinoleic acid is a common main component of castor oil, characterized as an unsaturated fatty acid with 18 carbons in its structure with a hydroxyl group (OH) at C12, whereas the 8-hydroxyricinoleic acid is not common, having an additional OH at C8. Other fatty acids that occurred in smaller quantities were oleic (1.06%), linoleic (3.61%), linolenic (0.87%), and palmitic acids (0.85%). These results also coincide with those reported by Ribeiro et al. [14], who reported that the chemical versatility of castor oil is related to the high concentrations of the fatty acid consisting of ricinoleic acid and derivatives (> 70%). Therefore, the main chemical properties of castor oil are rationalized by the presence of hydroxyl groups on fatty acid moieties, leading to an easy transformation of castor oil for different purposes [36]. In addition, the hydroxyl group of ricinoleic acid provides castor oil with unusual properties such as high viscosity, high density, and solubility in alcohol [33]. Regarding the synthesis of polyurethanes, the trihydroxy structure of ricinoleic acid-based triglycerides can lead to producing attractive, cross-linked urethane systems [36]. The present study then exploited these features to prepare the test castor oil–based PU films.
Characterization of castor oil–based PU films
FTIR-based characterization of castor oil–based PUs
The PU synthesis from castor oil and isophorone diisocyanate without catalysts followed our standardized procedure [8, 29, 30]. Chitosan and heparin were then added in the solid state as fillers to form PU/Ch/Hep composites, which are linked through hydrogen bond interactions, and, consequently, they are considered physical cross-linkers [13]. Therefore, they did not intervene in the PU synthesis, so covalent bonds were not expected to be formed between PU and fillers. Hence, after PU synthesis, twelve prepared film materials corresponding to castor oil-based PUs were initially characterized by FTIR analysis. Figure 1(a) shows the FTIR spectra of those materials based on PUs prepared from castor oil and isophorone diisocyanate with and without fillers (chitosan and heparin). A band was observed at 3341 cm−1 that corresponds to the N–H absorption generated by the urethane bond formation [16, 37]. Furthermore, two bands at 2925 cm−1 and 2853 cm−1 corresponded to the CH2 symmetric and asymmetric stretching, coinciding with the FTIR spectra reported for biobased polyurethanes using canola oil as the polyol source [38]. A peak is absent at 2270 cm−1, typical for the diisocyanate N=C=O group, which means that the NCO group was entirely converted into PU [39], which was confirmed by the band observed at 1704 cm−1 corresponding to the urethane stretching (‒C=O) [37]. The 1527 cm−1 band was due to the N‒H bending of ‒HNCOO‒ group [40], and the 1232 cm−1 band is the characteristic absorption of the urethane group [16]. These bands were found to be different from the FTIR spectra of the neat castor oil as starting material and the neat chitosan and neat heparin as fillers (Figures S2, S3), which indicate the adequate preparation of the PU-based film materials. In addition, chitosan and heparin do not have any impact on the FTIR data of the synthesized PUs by their role as fillers (i.e., physical cross-linkers) on using low loads (< 3% and < 0.1%, respectively, Table 3).
(a) FTIR spectra of castor oil-based polyurethanes (PUs). Ch = chitosan; Hep = Heparin; PU-Ch0-Hep0 = PU without fillers; PU-Ch3-Hep0.1 = PU with fillers (Ch at 3%w/w; Hep at 0.1% w/w), according to Table 1. (b) Tensile strength of castor oil–based polyurethanes (PUs). Data are expressed as the mean ± SD (n = 3). Bars with different lowercase letters (a, b, c) indicate significant differences according to the Tukey test (p < 0.05) between the test materials without and with fillers (different w/w percentages of chitosan (Ch) and heparin (Hep) based on the information in Table 1).
Mechanical properties of castor oil–based PUs
The design of biomaterials with optimized mechanical properties, combined with techniques to improve biocompatibility, is an essential requisite for biomedical applications. Such an aim was intended through the PU synthesis from polyol-derived castor oil and adding heparin and chitosan as fillers since the optimized biomaterials should model the mechanical and signaling features of native tissues. The mechanical properties of castor oil–based PUs show maximum stress at 1.091 ± 0.004 MPa [Figs. 1(b) and S4], and the effect of adding commercial chitosan and heparin tends to decrease the maximum stress at 0.859 ± 0.062 MPa. The PU’s tensile strength values presented values close to 1.0 MPa, which coincided with the results of those PUs synthesized by Wang et al. [41] The mechanical properties are influenced by the hydrogen bonding given by strong polar groups like OH, COOH, etc. This bonding can increase the physical cross-linking density and make chain moving difficult [11]. In addition, according to Hiob et al. [42], the elastic modulus of native blood vessels has values ranging from 0.3 (e.g., for the human internal mammary artery) to 1.5 MPa (e.g., for the human saphenous vein). This range agrees with our results related to the PU elastic modulus by adding heparin and chitosan, which varied between 1.0 and 1.2 MPa. Similarly, the results of PUs are similar to those reported for thermoplastic polyurethanes synthesized with poly(lactic acid), whose values changed between 1.0 and 4.0 MPa. [25] From the findings described above, the prepared PUs fill such an elastic requirement to design cardiovascular devices.
On the other hand, elongation percentages were found to be close to 80% (Table 2), and the filler effect by chitosan and heparin decreased the percentage to ca. 70% [38]. Table 2 shows that the elongation percentage of the castor oil–based PUs was between 66.6 ± 7.2% and 91.0 ± 4.5%. Therefore, these materials can be proposed as suitable for designing cardiovascular devices considering the elongation percentages of human blood vessels between 10 and 105% [42]. These results are similar to those reported by a previous study on PUs prepared from polyol-containing canola oil, whose elongation percentage of the synthesized PUs, obtained from 90 mg/g of canola oil-derived polyol, was found to be ca. 70% [38]. Additionally, the thermal analysis determined if there is an interaction between the polymeric matrix and the fillers used for the synthesis. The thermal characterization was carried out in a thermogravimetric analyzer and differential scanning calorimetry (Table 2). Generally, the PU degradation mechanism is a complex heterogeneous process due to the different characteristics of its hard and soft segments and their interaction with each other. [43]
All synthesized PUs showed good thermal stability below 300 ºC. This finding coincided with those results for polymers synthesized with the castor oil-derived monomer to produce biodegradable ricinoleic acid–based unsaturated polyesters proposed as suitable materials for biomedical applications [44]. According to the results presented in Table 2 and Figure S5, it can be inferred that the filler use does not alter the characteristic thermal behavior of PUs. Thermogravimetric analysis showed a similar weight loss tendency for PUs synthesized with castor oil, which could be divided into three distinct stages. Data showed the beginning of each stage for the synthesized materials. Hard segments broke down first, followed by PU soft segments. Therefore, the first stage corresponded to the hard segment decomposition of the urethane and urea bonds (approx. 266 °C) [39]. The second stage was related to the ester cleavage from castor oil (approx. 350 °C) [43]. Finally, the third stage corresponded to the thermal degradation of the films due to the double bonds of the remaining fatty acids from castor oil (approx. 415 °C) [12]. In the DSC data of the castor oil–based PUs (Table 2), a single Tg was observed at low temperatures, indicating that the materials have a homogeneous structure. The previous fact was deduced considering that, at the glass transition temperatures, it is possible to identify the phase separation degree or compatibility between them [45]. In addition, no significant differences were observed between the different test filler concentrations, indicating that the chitosan and heparin acted as fillers and unaffected the thermal properties of the castor oil–based PUs, and involving Tg values ranging between − 9.2 and − 12.3 °C. A study focused on bio-based PU adhesives, including castor oil and cellulose acetate, found Tg values from − 16 to − 20 °C. The authors argued that the microphase compatibility provided the narrow difference of the polymeric matrices due to the increased urea bond production by modifying the materials’ synthetic route. [45]
Considering that the adhesion-based cell response is affected by the synthesized material properties, such as surface chemistry and topography [28], the PU morphology was then characterized by FESEM to determine if the prepared polymers presented homogeneity depending on the used fillers or, on the contrary, they formed aggregates on the polymeric matrix. The resulting micrographs of the castor oil–based PU films exhibited smooth and uniform surfaces and displayed consequently homogeneous morphology [Figs. 2(a), S6–S8]. This evidence indicated that the prepared films have a single phase, although internally trapped particles are limited to being detected, requiring other techniques such as TEM or AFM. However, some aggregates were observed on the film surface [Figs. 2(a1-2), S6, S7], credited to the remnants from the synthesis process or the respective material manipulation. Similar performance was observed for thermoplastic PU-based vascular grafts containing the antiplatelet drug dipyridamole, whose SEM images of those materials with 5% dipyridamole showed smooth surfaces with some aggregates [25]. Additionally, micro-cracks were also observed, which were attributed to the mold type used for the PU sheet curing process.
(a) FESEM micrographs of castor oil-based PUs at ETH = 2.00 kV, Mag = 5.00 KX (1) PU-Ch0-Hep0 (2) PU-Ch3-Hep0 (3) PU-Ch3-Hep0.1; (b) Contact angle of castor oil-based PUs. (c) Water absorption of castor oil-based PUs. Data are expressed as the mean ± SD (n = 10). Bars with different letters (a, b, c) indicate significant differences according to the Tukey test (p < 0.05) between the test materials without and with fillers (different w/w percentages of chitosan (Ch) and heparin (Hep) based on the information in Table 1).
Static water contact angle measurements were used to obtain additional information about the surface properties and analyze the relative surface hydrophilicity of castor oil–based PUs [Fig. 2(b)]. The contact angle exhibited high values (91° < θ < 104°), exhibiting slight differences between prepared materials, although with some significant differences (p < 0.05), and no clear additive-related pattern was observed. However, chitosan additions appeared to reduce the contact angle slightly, and heparin had no effect. The average contact angle was found to be 98.39 ± 6.49°, which agrees with previously published results, indicating that the surfaces of the prepared PU films have a hydrophobic character [12], and adding chitosan and heparin does not affect the surface film hydrophobicity. The high contact angle values can be assigned to the PU cross-linking density, which generates a decreased free volume in the polymer chain. This fact makes polymeric matrices more compacted, limiting the water entering to wet the PU surface [43]. The obtained contact angles constituted average values that can allow cell adhesion and drug transport, which is very important in biomaterials. The study developed by Rajalakshmi et al. [44] was oriented to synthesize polyesters with ricinoleic acid from castor bean oil, which were proposed for biomedical applications. The contact angles of these polymers were found to be between 65° and 100°. The authors stated that a low hydrophilic character (θ < 90°) was due to the hydrophobic nature of ricinoleic acid. However, the apparent hydrophobic effect of the castor oil components in the present prepared PUs seemed to be reduced by chitosan and heparin as inserted fillers. In this regard, water absorption measurements supported these observations (Fig. 2(c)). Results indicated that the water absorption percentage tended to increase as the chitosan concentration increased, but heparin additions did not affect the water absorption. In this context, the swelling ratio must depend on the polymer volume fraction [46]. Our study on water absorption of prepared PUs exhibited values that vary between ca. 1% and 2.5%. These absorption percentages are relatively low, and this feature can be attributed to the cross-linking density and hydrophobicity [44], being the above-described characteristics of these synthesized castor oil–based PUs. This fact can be rationalized due to the low availability of chitosan and heparin used as fillers since they are part of the thick film block.
Biological characterization of castor oil–based PUs
The biological characterization of studied polymers is required to have background information to judge their potential biocompatibility [8]. In this context, degradation is a relevant factor to be measured. The degradation percentages in PBS castor oil–based PUs after 90 days were lower than 1% [Fig. 3(a)]. The reference PU film (i.e., without fillers) exhibited 0.118 ± 0.07% degradation, whereas PU films with chitosan and heparin showed degradation percentages higher than the reference material, reaching values of 0.646 ± 0.174%; therefore, the fillers increased the degradation slightly without exceeding 1% degradation. Additionally, porcine liver esterase was also used to evaluate the castor oil–based PU degradation, considering that esterases catalyze the PU hydrolysis and, therefore, biodegradation [15]. Nevertheless, the prepared PU films showed values lower than 0.1% biodegradation during the 21-day evaluation (data not shown) due to the cross-linking density and hydrophobicity of the test PUs, as determined by previous tests.
Biological characterization of synthesized castor oil–based polyurethane (PU) films. (a) In vitro degradation with PBS for three months. (b) Cell viability effect on L-929 cells; C(–)_latex = latex as negative control; (c) Cell viability effect on HDFa cells; C(–)_latex = latex as negative control; (d) Antibacterial activity against Escherichia coli; CFU/mL = colony formation unit per mL; Control( +) = 1:1 penicillin–streptomycin mixture as positive control; Control(–) = no PU treatment; E.coli(t = 0) = Number of colonies at the beginning of the assay at 0 h. (e) Antibacterial activity against methicillin-resistant Staphylococcus aureus (MRSA). Data are expressed as the mean ± SD (n = 6). Bars with different bold letters (a,b,c,d) indicate significant differences according to the Tukey test (p < 0.05) between the test materials without and with fillers (different w/w percentages of chitosan (Ch) and heparin (Hep) based on the information in Table 1).
On the other hand, the cell viability of the synthesized castor oil–based PUs with chitosan and heparin was also determined by direct contact with mouse fibroblast L-929 cells and primary human dermal fibroblasts (HDFa) for 24 h [Fig. 3(b), (c)]. The PU films showed acceptable performance on the test L929 and HFDa cells with values close to 80%. Thus, it can be inferred that these matrices are biocompatible for cells and, therefore, can be safe for implantation [47]. In contrast, the negative control (i.e., latex) produced the expected outcome, i.e., 13.5 ± 1.3% and 12.6 ± 0.8% for L929 and HDFa viability, respectively. In the case of the mouse fibroblast L-929 cells [Fig. 3(b)], cell viability percentages higher than 91.0 ± 14.2% were obtained for all PU films with some variations. On the other hand, the HDFa viability percentages [Fig. 3(c)] were higher than 69.0 ± 6.2%. Although slight variations were also found, significant differences resulted from the highest chitosan (3%) and heparin (0.1%) loads, which tended to a slight cell viability decrease without becoming toxic. Similar results were found for those silver-containing PUs mixed with polycaprolactone and hexamethylene diisocyanate, whose cell viability was greater than 85%, indicating that the produced materials have good potential as biomaterials [48]. Thus, our findings on the effect of PUs on the cell viability of L-929 and HDFa led us to infer that these materials can be further explored for designing cardiovascular devices.
Plant oils are currently employed for synthesizing polymers for biomedical applications due to their biological properties that favor biocompatibility and reasonable response to biological stimuli. In addition, the oils also have some characteristics, such as anti-inflammatory, antioxidant, and antibacterial activity, among others [14], which add relevant features to the test material. In previous GC–MS-based analyses using silylating derivatization, the castor oil used as a polyol source had a low impurities content (data not shown), which agreed with the low observed cytotoxicity. Although ricinoleic acid and its triglycerides exhibited toxicity [49], its appropriate incorporation into the PU structure, combined with low impurities due to proper oil refining, improved the cell viability. According to Ribeiro et al. [14], certain impurities of plant oils (e.g., further metabolites, metals, and pesticide residues) can be responsible for their toxic effects. In this sense, recent surveys have shown that very low impurity concentrations, after adequate purification and refining, have no health risks, allowing these oils to be used in biomedical applications. [50]
The antibacterial activity of the castor oil–based PUs, mixed with chitosan and heparin, was determined by direct contact with E. coli and MRSA for 24 h [Fig. 3(d), (e)]. The antibacterial activity against E. coli and MRSA was assessed since they are two pathogens generally associated with hospital-derived infections [25]. A significant difference was observed between PU-based treatments and negative control (without treatment) for the two test bacteria. PUs with chitosan (1%) + heparin (0.1%) loads showed 3.33 × 106 ± 1.50 × 106 CFU/mL of E. coli and, compared to the negative control that exhibited 1.03 × 107 ± 1.53 × 106 CFU/mL, indicated that these PUs had antimicrobial activity against E. coli. On the other hand, PUs with chitosan (1%) + heparin (0.1%) loads also promoted a MRSA growth reduction (1.07 × 107 ± 2.08 × 106 CFU/mL of the PU treatment versus. 3.57 × 107 ± 2.31 × 106 CFU/mL of the negative control), which suggested that the PUs have antibacterial action against MRSA. In this regard, it was deduced that castor oil–based PUs showed antibacterial activity against E. coli and MRSA. Castor oil derivatives have exhibited antimicrobial activity through bacterial membrane damage against pathogens such as S. aureus, A. brasiliensis, Penicillium, and B. subtilis [14]. In the case of E. coli [Fig. 3(d)], there are no significant differences by adding chitosan or heparin. However, in the case of MRSA (Fig. 3(e)), significant differences can be observed if heparin is added to the polymer.
Concluding remarks
In summary, the present study aimed to synthesize PU films using castor oil–based polyols and isophorone diisocyanate, including mixtures of chitosan and heparin as fillers for improving the cross-linking density. The functional groups of the prepared polymers were determined to be PU by FTIR analysis. The mechanical properties presented maximum stress values close to 1.00 MPa, and the effect of adding commercial chitosan modified with heparin tended to decrease these values by 30%. The materials also exhibited elongation percentages close to 80%, and the fillers’ effect reduced this percentage by 10%. The static water contact angle was found to be high (> 90°), and the water absorption was low (> 2.3%), but the 3% chitosan promoted a slight increase (ca. 1%) in comparison to PU without fillers. The synthesized materials exhibited low degradation in PBS (< 0.1%) and by contact with esterase (< 0.1%) and promoted lower bacterial growth than the negative control (bacteria without exposure to the test polymers), indicating that they have antimicrobial activity. Finally, cell viability was found to be higher than 80%, indicating that PUs are not cytotoxic. In conclusion, these PU films exhibited attractive mechanical and in vitro biological properties since they offer competitive advantages over other materials. Therefore, in subsequent studies, these PUs can be candidate materials for designing cardiovascular devices and implants.
Materials and methods
Reagents and materials
The pure castor (Ricinus communis) oil was obtained from Químicos Campota y Cía, Ltda., Ecuador. Isophorone diisocyanate (98 wt% purity, mixture of cis/trans isomers), low molecular weight chitosan ≥ 75% (deacetylated)), porcine liver esterase (20 units mg−1), heparin sodium salt from porcine intestinal mucose (180 units mg−1), DMEM 1X (Dulbecco’s modified Eagle medium), MTT (3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide), 2,5% trypsin (10X), penicillin–streptomycin (10,000 units of penicillin and 10,000 μg of streptomycin per milliliter) and FBS (fetal bovine serum) were purchased from Sigma-Aldrich Chemical Co. (St. Louis, MO, USA). PBS (Dulbecco’s phosphate-buffered saline) from Biowest, Nuaille, FR. Escherichia coli (ATCC 2469), methicillin-resistant Staphylococcus aureus (MRSA), L-929 mouse subcutaneous connective tissue fibroblasts cells (ATCC® CCL-1), and HDFa human primary dermal fibroblast cells (ATCC® PCS-201-012TM) were purchased from the strain library of the Universidad de La Sabana (Colombia). TSB (Trypticase soy broth) and TSA (trypticase soy agar) were purchased Scharlau Co (Spain).
Chemical composition of castor oil
Castor oil characterization
The castor oil was initially characterized by typical measurements based on refractive and iodine indexes, saponification number, hydroxyl number, and insoluble impurities, following standard procedures [32]. In addition, the lipid profile of castor oil was analyzed by GC/ESIMS after the derivatization into their fatty acid methyl esters (FAMEs) of saponified triglycerides.
FAMEs profile of castor oil
Castor oil (30 mg) was weighed and dissolved in 0.5 M alcoholic NaOH (1.5 mL). The mixture was heated to 60 °C for 5 min under reflux. BF3-MeOH (2.0 mL) was added and kept at 60 °C for an additional 30 min. The temperature was lowered to 30 °C, and isooctane (2.0 mL) and saturated NaCl solution (5.0 mL) were added until phase separation. The organic phase was placed in a glass vial containing anhydrous MgSO4. This FAME extract was then analyzed by GC/EIMS.
Gas chromatography-electron impact mass spectrometry (GC/EIMS) analysis
The chromatographic analysis was performed in a Trace 1300 LT gas chromatograph (Thermo Scientific, Waltham, MA, USA) with an AI 1310 autosampler, coupled to a Thermo ISQ Mass Spectrometer, with electron impact ionization mode and a single quadrupole analyzer. A column of 60 m × 0.25 mm ID × 0.25 µm DB-5 (Rxi® 5 Sil MS, Restek, State College, PA, USA) was used. Helium (99.999%) with a 1.0 mL/min flow was used as carrier gas. The sample (1 µL) was injected in split mode, and the injection port temperature was 300 °C. The temperature program started with an initial temperature (40 °C), maintained for 1 min, then increased from 150 to 300 °C at 10 °C/min, and held for 4 min. It was then increased to 310 °C at 10 °C/min, and maintained for 6 min. The ion source temperature was 250 °C, and the transference line temperature was 280 °C. [51] The electron impact was achieved at 70 eV, and the detection was performed by scan mode (10–1000 m/z). In addition, linear retention indexes (LRI) were calculated using the retention time performance of a C10–C24 n-alkane series analyzed under identical conditions.
Castor oil-derived PU synthesis with fillers
The commercially purchased, unmodified castor (Ricinus communis) oil was mixed with isophorone diisocyanate using an NCO/OH 1:1 ratio to form a pre-polymer at 60 °C, 300 rpm for 5 min. [52] Then, a solid-phase homogenized mixture of chitosan and heparin (Chi/Hep) was added to the pre-polymer mixture, according to the mixtures presented in Table 1. The material was poured into a 15 cm × 9 cm × 0.3 cm (length × width × height) steel mold and cured at 110° C for 12 h to obtain the PU sheets [53]. At this temperature (110 °C), the fillers (heparin and chitosan) were thermally stable (Figure S9).
Characterization of castor oil-derived PU
The FTIR spectrum of the synthesized PUs was obtained in an ATR-FTIR spectrometer (Agilent Cary 630 FTIR Spectrometer), in a range of 400 and 4000 cm−1, with 24 scans and a spectral resolution of 4 cm−1. [18, 54] The percentage of elongation and the maximum stress were determined following ASTM D638-10, in an EZ-LX universal testing machine (Shimadzu, Japan), with a load cell of 5 kN at 25 mm min−1 of displacement [55, 56]. The thermal stability of PUs was investigated in a thermogravimetric analyzer coupled to differential scanning calorimetry model TGA/DCS1—Mettler Toledo, USA, following ASTM D6370, in a temperature range of 25–600 °C, at a heating rate of 25 °C/min in a nitrogen atmosphere and 15 ± 2 mg samples [19]. The glass transition temperature was determined in a DSC (Differential Scanning Calorimetry) analyzer, model DSC 3 + (Mettler Toledo, USA), by measuring the inflection point a temperature from − 70 to 150 ºC at a heating rate of 20 ºC/min, under nitrogen atmosphere with 20 mL/min of flow and 10 ± 2 mg samples [57]. The PU hydrophilicity was evaluated by a “Drop Shape Analysis—DSA” (GH11, Krüss) (Germany), suggesting ASTM-D7334-08 (2013) with the “sessile drop” method, using distilled water (10 µL) at 20 °C. [58] Morphological characterization was performed in a Field Emission Scanning Electron Microscope (FESEM), ZEISS (ULTRA 55) from Oxford Instruments. The samples were coated with platinum at an acceleration voltage of 5 kV. [59] Micrographs were captured at a high voltage (EHT) of 2.00 kV, 5-KX magnifications, and working distances between 5.7 and 6.0 µm to characterize the surface of the materials. The percentage of water absorption was determined by thermogravimetry after immersion in distilled water of the sample until obtaining constant weight at 37 °C. [60] The percentage of water absorption was calculated by comparing the final sample mass (mf) with the initial mass (mi) employing Eq. 1.
Biological properties of castor oil–derived PU
In vitro PU degradation
PU film samples (5 × 5 × 3 mm) were placed in phosphate buffer saline and incubated at 37 °C for 120 days. PUs with identical dimensions were placed in porcine liver esterase enzyme medium (10 units/mg solid) at 37 °C for 21 days. Then, the PUs were kept at 37 °C until a constant weight was obtained. The final material weight was obtained by gravimetry, and the biodegradation percentage was calculated by comparing the sample dry weight (Wf) after degradation with the original sample dry weight (Wi) using Eq. 2. [59, 61]
In vitro cell viability
The effect of PU films on in vitro cell viability was determined by the MTT method (ISO/CD 10993-5) [62]. L-929 mouse subcutaneous connective tissue fibroblast cells and HDFa human primary dermal fibroblast cells were grown in medium DMEM supplemented with 5% fetal bovine serum, 100 mg/mL penicillin–streptomycin, at 37° C and 5% CO2 humidified atmosphere. Cells were cultured in 96-well plates at a concentration of 40,000 cells per well at 37 °C and 5% CO2 for 24 h. Then the media was removed, and cylinders (3 × 2 mm, diameter × height) from PU films were placed over the cells for 24 h at 37 °C and 5% CO2. Then, the medium was removed along with the polymers, and a MTT solution (12 mM in PBS) was added (total volume of 100 µL) for 4 h at 37 °C. The supernatant was discarded, and dimethyl sulfoxide (50 µL) was added for 15 min at 37 °C. Optical density was determined on an iMark™ absorbance microplate reader (Bio-Rad) at 595 nm. Latex was used as the negative control. All tests were carried out in triplicate. Cell viability was determined according to Eq. 3.
where ODsample corresponds to cells after treatment with the biobased PUs, and ODcontrol corresponds to cells without treatment.
Antibacterial activity
The PU films were incubated in PBS (100 µL), adding bacterial suspensions in PBS, previously fine-tuned to Mcfarland’s 0.5 standard (E. coli and methicillin-resistant S. aureus). After incubation at 37 °C for 24 h, the bacterial solutions were plated on trypticase soy agar (TSA) plate and incubated at 37 °C for 18 h. The bacterial colonies were counted and expressed as colony-forming units per milliliter (CFU/mL) at 37 °C for 18 h. A bacterial suspension without test polymers was used as a negative control (–), and penicillin–streptomycin was used as a positive control (+).
Statistical analysis
The results were expressed as the mean ± standard deviation (SD). Shapiro-Wilks test was used to verify the normal distribution of data. Then, data means were compared using a one-way analysis of variance (ANOVA). A posthoc Tukey test examined the statistically significant differences (p < 0.05) between means by creating confidence intervals for all pairwise differences. These intervals were clustered into groups denoted by different lowercase letters (placed over bars in Figures), indicating significant differences between the factor levels.
Data availability
Data and materials are available from the authors upon reasonable request.
References
T. Sologashvili, S.A. Saat, J.C. Tille, S. De Valence, D. Mugnai, J.P. Giliberto, J. Dillon, A. Yakub, Z. Dimon, R. Gurny, B.H. Walpoth, M. Moeller, Effect of implantation site on outcome of tissue-engineered vascular grafts. Eur. J. Pharm. Biopharm. 139(April), 272 (2019)
J.L. Johnson, Elucidating the contributory role of microRNA to cardiovascular diseases (a review). Vascul Pharmacol 114(July 2018), 31 (2019)
J. Domínguez-Robles, T. Shen, V.A. Cornelius, F. Corduas, E. Mancuso, R.F. Donnelly, A. Margariti, D.A. Lamprou, E. Larrañeta, Development of drug loaded cardiovascular prosthesis for thrombosis prevention using 3D printing. Mater. Sci. Eng. C 129, 112375 (2021)
P. Davoudi, S. Assadpour, M.A. Derakhshan, J. Ai, A. Solouk, H. Ghanbari, Biomimetic modification of polyurethane-based nanofibrous vascular grafts: a promising approach towards stable endothelial lining. Mater. Sci. Eng. C 80, 213 (2017)
H.Y. Mi, Y. Jiang, X. Jing, E. Enriquez, H. Li, Q. Li, L.S. Turng, Fabrication of triple-layered vascular grafts composed of silk fibers, polyacrylamide hydrogel, and polyurethane nanofibers with biomimetic mechanical properties. Mater. Sci. Eng. C 98(September), 241 (2019)
Q. Cai, W. Liao, F. Xue, X. Wang, W. Zhou, Y. Li, W. Zeng, Selection of different endothelialization modes and different seed cells for tissue-engineered vascular graft. Bioact. Mater. 6(8), 2557 (2021)
M. Rychter, A. Baranowska-Korczyc, B. Milanowski, M. Jarek, B.M. Maciejewska, E.L. Coy, J. Lulek, Cilostazol-loaded poly(ε-caprolactone) electrospun drug delivery system for cardiovascular applications. Pharm. Res. 35(2), 1 (2018)
Y.L. Uscátegui, L.E. Díaz, M.F. Valero, In vitro and in vivo biocompatibility of polyurethanes synthesized with castor oil polyols for biomedical devices. J. Mater. Res. 34(4), 519 (2019)
V.P. do Canto, C.E. Thompson, P.A. Netz, Polyurethanases: three-dimensional structures and molecular dynamics simulations of enzymes that degrade polyurethane. J. Mol. Graph Model 89, 82 (2019)
S. Saleh, N.Z.M. Yunus, K. Ahmad, N. Ali, Improving the strength of weak soil using polyurethane grouts: a review. Constr. Build. Mater. 202, 738 (2019)
W.S. Ng, C.S. Lee, C.H. Chuah, S.F. Cheng, Preparation and modification of water-blown porous biodegradable polyurethane foams with palm oil-based polyester polyol. Ind. Crops Prod. 97, 65 (2017)
W. Zhang, H. Deng, L. Xia, L. Shen, C. Zhang, Q. Lu, S. Sun, Semi-interpenetrating polymer networks prepared from castor oil-based waterborne polyurethanes and carboxymethyl chitosan. Carbohydr. Polym. 256(July 2020), 117507 (2021)
P.J. Trzebiatowska, A.S. Echart, T.C. Correas, A. Eceiza, J. Datta, The changes of crosslink density of polyurethanes synthesised with using recycled component. Chemical structure and mechanical properties investigations. Prog Org Coat 115(November 2017), 41 (2018)
A.R. Ribeiro, S.S. Silva, R.L. Reis, Challenges and opportunities on vegetable oils derived systems for biomedical applications. Biomater. Adv. 134, 112720 (2022)
R. Kaur, P. Singh, S. Tanwar, G. Varshney, S. Yadav, Assessment of bio-based polyurethanes: perspective on applications and bio-degradation. Macromol 2(3), 284 (2022)
J.P.P. de Morais, I.K.C. Pacheco, A.L.M.M. Filho, D.C.L. Ferreira, F.J.C. Viana, F. da Silva Reis, J.M.E. de Matos, M. dos Santos Rizzo, A.C.V. Fialho, Polyurethane derived from castor oil monoacylglyceride (Ricinus communis) for bone defects reconstruction: characterization and in vivo testing. J. Mater. Sci. Mater. Med. 32(4), 39 (2021).
T.S. Omonov, E. Kharraz, J.M. Curtis, Camelina (Camelina Sativa) oil polyols as an alternative to Castor oil. Ind. Crops Prod. 107(May), 378 (2017)
M.A. Mekewi, A.M. Ramadan, F.M. ElDarse, M.H. Abdel Rehim, N.A. Mosa, M.A. Ibrahim, Preparation and characterization of polyurethane plasticizer for flexible packaging applications: natural oils affirmed access. Egypt. J. Pet. 26(1), 9 (2017).
F. Arévalo, Y.L. Uscategui, L. Diaz, M. Cobo, M.F. Valero, Effect of the incorporation of chitosan on the physico-chemical, mechanical properties and biological activity on a mixture of polycaprolactone and polyurethanes obtained from castor oil. J. Biomater. Appl. 31(5), 708 (2016)
K. Mahmood, K.M. Zia, W. Aftab, M. Zuber, S. Tabasum, A. Noreen, F. Zia, Synthesis and characterization of chitin/curcumin blended polyurethane elastomers. Int. J. Biol. Macromol. 113, 150 (2018)
S.A. Shah, M. Sohail, M.U. Minhas, S. Khan, M. de Matas, V. Sikstone, Z. Hussain, M. Abbasi, and M. Kousar, Biopolymer-based biomaterials for accelerated diabetic wound healing: a critical review. Int. J. Biol. Macromol. (2019).
K.Y. Lee, W.S. Ha, W.H. Park, Blood compatibility and biodegradability of partially N-acylated chitosan derivatives. Biomaterials 16(16), 1211 (1995)
A.A. Romani, L. Ippolito, F. Riccardi, S. Pipitone, M. Morganti, M.C. Baroni, A.F. Borghetti, R. Bettini, Advances in Biomaterials Science and Biomedical Applications (IntechOpen, Rijeka, 2013)
R. Biran, D. Pond, Heparin coatings for improving blood compatibility of medical devices. Adv Drug Deliv Rev 112, 12 (2017)
J. Domínguez-Robles, E. Utomo, V. A. Cornelius, Q. Kurnia Anjani, A. Korelidou, Z. Gonzalez, R. F. Donnelly, A. Margariti, M. Delgado-Aguilar, Q. Tarrés, E. Larrañeta, TPU-based antiplatelet cardiovascular prostheses prepared using fused deposition modelling. Mater. Des. 220, 110837 (2022).
D. Kim, J.J. Chung, Y. Jung, S.H. Kim, The effect of Substance P/Heparin conjugated PLCL polymer coating of bioinert ePTFE vascular grafts on the recruitment of both ECs and SMCs for accelerated regeneration. Sci. Rep. 9(1), 1 (2019)
J.B. Osorno, Biomateriales de uso cardiovascular. Médicas UIS 21(1), 67 (2008)
G.A. Venegas-Cervera, A.I. Oliva, A. Avila-Ortega, J.M. Cervantes-Uc, L.M. Carrillo-Cocom, J.A. Juarez-Moreno, Biocompatibility studies of polyurethane electrospun membranes based on arginine as chain extender. J. Mater. Sci. 32(9), 1 (2021)
Y.L. Uscátegui, S.J. Arévalo-Alquichire, J.A. Gómez-Tejedor, A. Vallés-Lluch, L.E. Díaz, M.F. Valero, Polyurethane-based bioadhesive synthesized from polyols derived from castor oil (Ricinus communis) and low concentration of chitosan. J. Mater. Res. 32(19), 3699 (2017)
S. Arévalo-Alquichire, C. Ramírez, L. Andrade, Y. Uscategui, L.E. Diaz, J.A. Gómez-Tejedor, A. Vallés-Lluch, M.F. Valero, Polyurethanes from modified castor oil and chitosan: synthesis, characterization, in vitro degradation, and cytotoxicity. J. Elastomers Plast. 50(5), 419 (2018)
Y.L. Uscátegui, L.E. Díaz, J.A. Gómez-Tejedor, A. Vallés-Lluch, G. Vilariño-Feltrer, M.A. Serrano, M.F. Valero, Candidate polyurethanes based on castor oil (Ricinus communis), with polycaprolactone diol and chitosan additions, for use in biomedical applications. Molecules 24(2), 237 (2019)
F. Mustata, N. Tudorachi, Synthesis and thermal characterization of some hardeners for epoxy resins based on castor oil and cyclic anhydrides. Ind. Crops Prod. 159, 113087 (2021)
Í.C. Rios, J.P. Cordeiro, T.B.M.G. Arruda, F.E.A. Rodrigues, A.F.J. Uchoa, F.M.T. Luna, C.L. Cavalcante, N.M.P.S. Ricardo, Chemical modification of castor oil fatty acids (Ricinus communis) for biolubricant applications: an alternative for Brazil’s green market. Ind. Crops Prod. 145, 112000 (2020)
A.M.A. Attia, M. Nour, A.I. El-Seesy, S.A. Nada, The effect of castor oil methyl ester blending ratio on the environmental and the combustion characteristics of diesel engine under standard testing conditions. Sustain. Energy Technol. Assess. 42, 100843 (2020)
R.K. Elango, K. Sathiasivan, C. Muthukumaran, V. Thangavelu, M. Rajesh, K. Tamilarasan, Transesterification of castor oil for biodiesel production: process optimization and characterization. Microchem. J. 145, 1162 (2019)
A.A.G. Pájaro, L.R.M. Mendoza, Evaluación Del Comportamiento Físico-Mecánico de Una Poliuretano Reforzado, Producido a Partir de Aceite de Ricino, y Su Competitividad Técnica Como Material de Aplicabilidad Industrial, Universidad Industrial de Santander (2013).
M.A. Javaid, R.A. Khera, K.M. Zia, K. Saito, I.A. Bhatti, M. Asghar, Synthesis and characterization of chitosan modified polyurethane bio-nanocomposites with biomedical potential. Int. J. Biol. Macromol. 115, 375 (2018)
E. Aydoğmuş, F. Kamişli, New commercial polyurethane synthesized with biopolyol obtained from canola oil: optimization, characterization, and thermophysical properties. J. Mol. Struct. 1256, 132495 (2022)
S. Ruanpan, H. Manuspiya, Synthesized amino-functionalized porous clay heterostructure as an effective thickener in waterborne polyurethane hybrid adhesives for lamination processes. Int. J. Adhes. Adhes. 80(October 2017), 66 (2018)
F. Kara, E.A. Aksoy, Z. Yuksekdag, S. Aksoy, N. Hasirci, Enhancement of antibacterial properties of polyurethanes by chitosan and heparin immobilization. Appl. Surf. Sci. 357, 1692 (2015)
J. Wang, Z. Liu, M. Qiu, C. He, Heparin-mimicking semi-interpenetrating composite membrane with multiple excellent performances for promising hemodialysis. J. Memb. Sci. 618(May 2020), 118740 (2021)
M.A. Hiob, S. She, L.D. Muiznieks, A.S. Weiss, Biomaterials and modifications in the development of small-diameter vascular grafts. ACS Biomater. Sci. Eng. 3(5), 712 (2017)
W. Zhang, Y. Zhang, H. Liang, D. Liang, H. Cao, C. Liu, Y. Qian, Q. Lu, C. Zhang, High bio-content castor oil based waterborne polyurethane/sodium lignosulfonate composites for environmental friendly UV absorption application. Ind. Crops Prod. 142(October), 111836 (2019)
P. Rajalakshmi, J.M. Marie, A. John, M. Xavier, Castor oil-derived monomer ricinoleic acid based biodegradable unsaturated polyesters. Polym. Degrad. Stab. 170, 109016 (2019)
A. Tenorio-Alfonso, M.C. Sánchez, J.M. Franco, Impact of the processing method on the properties of castor oil/cellulose acetate polyurethane adhesives for bonding wood. Int. J. Adhes. Adhes. 116, 103153 (2022)
R. Tennankore, M. Brunette, T. Cox, R. Vazquez, A. Shikanov, M. L. Burns, B. Love, Swellable catheters based on a dynamic expanding inner diameter. J. Mater. Sci. Mater. Med. 32(5) (2021).
N. Bokhari, T. Fatima, S. Nosheen, F. Iqbal, F. Moeen, F. Sharif, Bioactive bacterial cellulose–chitosan composite scaffolds for prospective periodontal tissue regeneration. J. Mater. Res. 38(7), 1952 (2023)
L. Wang, W. Cao, X. Wang, P. Li, J. Zhou, G. Zhang, X. Li, X. Xing, Biodegradable silver-loaded polycation modified nanodiamonds/polyurethane scaffold with improved antibacterial and mechanical properties for cartilage tissue repairing. J. Mater. Sci. 30(4) (2019).
A. Blaszczyk, S. Matysiak, J. Kula, K. Szostakiewicz, Z. Karkusiewicz, Cytotoxic and genotoxic effects of (R)- and (S)-ricinoleic acid derivatives. Chirality 32(7), 998 (2020)
V.R. Patel, G.G. Dumancas, L.C.K. Viswanath, R. Maples, B.J.J. Subong, Castor oil: properties, uses, and optimization of processing parameters in commercial production. Lipid Insights 9, LPI.S40233 (2016)
R. Marentes-Culma, L. L. Orduz-Díaz, E. Coy-Barrera, Targeted metabolite profiling-based identification of antifungal 5-n-alkylresorcinols occurring in different cereals against fusarium oxysporum. Molecules 24(4) (2019).
M.F. Valero, L.E. Díaz, Poliuretanos obtenidos a partir de aceite de higuerilla modificado y poli-isocianatos de lisina: síntesis, propiedades mecánicas y térmicas y degradación in vitro. Quim Nova 37(9), 1441 (2014)
M.F. Valero, Y. Ortegón, Polyurethane elastomers-based modified castor oil and poly(e-caprolactone) for surface-coating applications: synthesis, characterization, and in vitro degradation. J. Elastomers Plast. 47(4), 360 (2015)
S.A.A. Shah, M. Imran, Q. Lian, F.K. Shehzad, N. Athir, J. Zhang, J. Cheng, Curcumin incorporated polyurethane urea elastomers with tunable thermo-mechanical properties. React. Funct. Polym. 128(May), 97 (2018)
R. Simón-Allué, P. Pérez-López, S. Sotomayor, E. Peña, G. Pascual, J.M. Bellón, B. Calvo, Short- and long-term biomechanical and morphological study of new suture types in abdominal wall closure. J. Mech. Behav. Biomed. Mater. 37, 1 (2014)
K. Yoshida, H. Jiang, M. J. Kim, J. Vink, S. Cremers, D. Paik, R. Wapner, M. Mahendroo, K. Myers, Quantitative evaluation of collagen crosslinks and corresponding tensile mechanical properties in mouse cervical tissue during normal pregnancy. PLoS ONE 9(11) (2014).
M.E.V. Hormaiztegui, M.I. Aranguren, V.L. Mucci, Synthesis and characterization of a waterborne polyurethane made from castor oil and tartaric acid. Eur Polym J 102(March), 151 (2018)
P. Kanmani, J.-W. Rhim, Physical, mechanical and antimicrobial properties of gelatin based active nanocomposite films containing AgNPs and nanoclay. Food Hydrocoll 35, 644 (2014)
P. Basak, B. Adhikari, Effect of the solubility of antibiotics on their release from degradable polyurethane. Mater. Sci. Eng., C 32(8), 2316 (2012)
S. Członka, M.F. Bertino, K. Strzelec, Rigid polyurethane foams reinforced with industrial potato protein. Polym. Test 68(April), 135 (2018)
Y. Wang, Y. Yu, L. Zhang, P. Qin, P. Wang, One-step surface modification of polyurethane using affinity binding peptides for enhanced fouling resistance. J. Biomater. Sci. Polym. Ed. 26(8), 459 (2015)
H. Bakhshi, H. Yeganeh, S. Mehdipour-Ataei, M.A. Shokrgozar, A. Yari, S.N. Saeedi-Eslami, Synthesis and characterization of antibacterial polyurethane coatings from quaternary ammonium salts functionalized soybean oil based polyols. Mater. Sci. Eng. C 33(1), 153 (2013)
Acknowledgments
Authors thank the financial support provided by “Fondo Nacional de Financiamiento para la Ciencia, la Tecnología, y la Innovación -Fondo Francisco José de Caldas- Minciencias, for the postdoctoral grant (Contract 160-2020) after 848-2019 call. Our gratitude is extended to Universidad Militar Nueva Granada (through Project IMP-CIAS-2924 and EXT-CIAS-3275) and Universidad de La Sabana for the financial, analytical, and facilities support.
Funding
Open Access funding provided by Colombia Consortium. Funding was provided by Ministerio de Ciencia Tecnología e Innovación (Minciencias) (160-2020) and Universidad Militar Nueva Granada (IMP-CIAS-2924, EXT-CIAS-3275).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest was reported by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Uscátegui Maldonado, Y.L., Díaz Barrera, L.E., Valero Valdivieso, M.F. et al. Synthesis and characterization of polyurethane films based on castor oil-derived polyols with heparin and low-molecular-weight chitosan for cardiovascular implants. Journal of Materials Research 38, 3349–3361 (2023). https://doi.org/10.1557/s43578-023-01060-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1557/s43578-023-01060-3