Abstract
β-amyloid-targeting antibodies represent the first generation of effective causal treatment of Alzheimer’s disease (AD) and can be considered historical research milestones. Their effect sizes, side effects, implementation challenges and costs, however, have stimulated debates about their overall value. In this position statement academic clinicians of the European Alzheimer’s Disease Consortium (EADC) discuss the critical relevance of introducing these new treatments in clinical care now. Given the complexity of AD it is unlikely that molecular single-target treatments will achieve substantially larger effects than those seen with current β-amyloid-targeting antibodies. Larger effects will most likely only be achieved incrementally by continuous optimization of molecular approaches, patient selection and combinations therapies. To be successful in this regard, drug development must be informed by the use of innovative treatments in real world practice, because full understanding of all facets of novel treatments requires experience and data of real-world care beyond those of clinical trials. Regarding the antibodies under discussion we consider their effects meaningful and potential side effects manageable. We assume that the number of eventually treated patient will only be a fraction of all early AD patients due to narrow eligibility criteria and barriers of access. We strongly endorse the use of these new compound in clinical practice in selected patients with treatment documentation in registries. We understand this as a critical step in advancing the field of AD treatment, and in shaping the health care systems for the new area of molecular-targeted treatment of neurodegenerative diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The increasing societal burden of dementia
Of the 450 million people living in the European Union (EU), one in five is 65 years or older. One in three will be 65 or older in 2050 (https://ec.europa.eu/eurostat/). The current estimate of 7.8 million people living with dementia in the EU will almost double to 14.3 million in 2050 (www.alzheimer-europe.org). A recent meta-analysis of 17 European studies reported annual costs of dementia of up to 74,000 € per person in the severe disease stage. More than 90% of the costs are related to care, while less than 10% are related to diagnostic procedures and medical treatment (1).
Dementia risk reduction and effects on dementia prevalence
A meta-analysis of epidemiological studies concluded that 40% of the population attributable risk of dementia is explained by potentially modifiable risk factors (2). Also, there is evidence that the age-specific prevalence and incidence rates of dementia are declining in industrialized countries (3). The magnitude of further reduction in age-specific incidence and prevalence of dementia, however, is uncertain, because some modifiable risk factors have already been successfully lowered at the population level over the past decades (e.g. smoking, hypertension) while others are on the rise (e.g. obesity, diabetes). Moreover, even under the assumption of a further decrease in age-specific incidence and prevalence of dementia, the disproportional demographic changes in Europe will override this effect and the burden of dementia for societies will continue to grow (https://ec.europa.eu/eurostat/). Approaches that slow the disease course and delay the time to moderate and severe dementia stages at an individual level are urgently needed.
Causes of dementia and new treatments
Alzheimer’s disease (AD), the most common cause of dementia, is defined by deposition of extracellular β-amyloid as plaques and intraneuronal aggregation of phosphorylated tau protein with subsequent neurodegeneration (4). Cerebrospinal fluid (CSF) and brain imaging (positron emission tomography, PET) biomarkers are available to detect both pathologies even before dementia at the stage of mild cognitive impairment (MCI). Blood-based biomarkers are under development, which will increase the accessibility of a molecular AD diagnosis (5, 6).
Recently, it has been demonstrated for the first time that monoclonal antibodies against specific epitopes of aggregated β-amyloid reduce amyloid deposits in the brain and slow the progression of symptoms of the disease. Aducanumab was the first antibody to show the association of amyloid lowering with slowing of symptomatic decline in a phase 2 clinical trial (7). The phase 3 clinical trial program of aducanumab comprised two parallel studies (EMERGE, ENGAGE), which were terminated early after a futility analysis. In both trials, strong amyloid reduction was observed, but the clinical data were inconclusive (8). The United States Food and Drug Administration (FDA) granted accelerated approval based on the amyloid reduction only with the requirement for clinical proof of efficacy.
Lecanemab is the first antibody with demonstration of clinical efficacy in a phase 3 program (9). While it is fully approved by the FDA and by the regulatory bodies of Japan, China and South Korea, the Committee for Medical Products for Human Use (CHMP) of the European Medicines Agency (EMA) recommended against approval in July 2024. Donanemab, the second amyloid-targeting antibody with proof of efficacy has been fully approved by the FDA in July 2024. This is a historical milestone in AD research as it is the first time that a causative treatment shows slowing of symptom progression. The current antibodies can be considered the first generation of a new era of molecular-targeted treatment of AD and most likely of other neurodegenerative diseases given that 127 drugs targeting β-amyloid as well as several other molecular mechanisms, are currently in clinical development (10).
Patient groups for β-amyloid-targeting antibodies
β-amyloid-targeting treatment aims at slowing the biological and symptomatic progression of AD. The target population of recent clinical trials were patients at the early symptomatic disease stage, either MCI or mild dementia. From the biological perspective, early treatment is plausible, because the spread and dynamics of pathology are less advanced at earlier stages, and more brain tissue is still preserved. Clinically, early treatment potentially maintains a stage of less impairment with more autonomy, higher independence, and lower costs of care. The efficacy of the new treatments in moderate and severe dementia is not studied and therefore remains unclear. It is likely, however, that the effects will be smaller than at earlier stages.
Outcomes of the clinical trials
The 18-month phase 3 clinical trials of the current β-amyloid-targeting antibodies with evidence for efficacy used validated clinical instruments for measuring cognition and daily function as primary and secondary endpoints (9, 11). The Clinical Dementia Rating-Sum of Boxes (CDR-SOB) is most commonly used in early symptomatic AD trials and was the primary outcome of the lecanemab phase 3 clinical study (CLARITY-AD) (12). The phase 3 clinical trial of donanemab (TRAILBLAZER-ALZ 2) used the Integrated Alzheimer Disease Rating Scale (iADRS) as the primary endpoint (13). The CDR-SOB served as a key secondary endpoint. Both assessments (CDR-SOB, iARDS) are based on cognitive testing and interviews with patients and study partners by expert clinicians (raters). Additional instruments for assessing clinical symptoms were used as secondary endpoints in both trials. The primary biological readout of these studies was change a in β-amyloid plaques load measured by PET (9, 11).
Effects and effect sizes
In CLARITY-AD and TRAILBLAZER-ALZ 2, there was consistent and significant slowing of decline on all clinical outcomes by antibody treatment compared with placebo. This was paralleled by a strong reduction of cerebral amyloid load to a level of what is considered amyloid-negative in most participants (9, 11).
The effect was a reduction in decline in comparison to placebo at the end of the studies of 27% on the CDR-SOB for lecanemab and of 35% on the iADRS for donanemab in the primary analysis group of TRAILBLAZER-ALZ 2, which were patients with low to medium tau deposition on PET. The absolute difference in favor of the drug vs. placebo in the CDR-SOB was 0.45 points for lecanemab and 0.68 points for donanemab in the low to medium tau group (0.67 in the full sample) (9, 11).
Clinical meaningfulness of the effects
There is an ongoing discussion about the clinical meaningfulness of the magnitude of the observed effects. The following points are important to consider: the CDR-SOB, the iADRS and all other scales used as clinical outcomes measure inherently meaningful features of the disease, namely impairment in cognition and function, which are the core symptoms that define the clinical manifestation of AD.
Regarding the most used CDR-SOB, studies have linked the magnitude of change on this scale to clinically relevant changes on external references (anchors). Based on the US National Alzheimer’s Coordinating Centers (NACC) database, one study reported a mean change in the CDR-SOB score of 0.98 in MCI-AD patients and of 1.63 in AD patients with mild dementia, who showed a minimal clinically important decline over 12 months according to physician judgement (14). A second study based on the Donepezil/Vitamin E in MCI clinical trial data (ADC-008 NCT00000173) calculated a meaningful change of the CDR-SOB of 0.64 points over 12 months by anchoring it to the MCI-Clinical Global Impression of Change Scale (MCI-CGIC) and of 1.08 by anchoring it to the Global Deterioration Scale (GDS) (15). These results show that the estimates differ substantially between MCI and mild dementia, indicating lower sensitivity to change in MCI, and that the estimates depend on the sample, the context of data acquisition and the selected anchor. It also needs to be recognized that the external anchors in these studies are clinician-based categorical judgements (i.e. worse, not worse) with imperfect reliability and validity. As such, these estimates can only serve as rough guidance. As a side note, in these studies, clinical meaningful change was defined by the treating physician or rater, not by the patient or the care partner.
According to these estimates, the placebo group in CLARITY-AD showed a clinically relevant decline (1.66 points), while the lecanemab group showed a borderline decline (1.21 points) (9). The placebo group in TRAILBLAZER-ALZ 2 showed a clearly relevant decline (1.82 points), while the donanemab group showed a decline of only borderline clinical relevance (1.16 points) (11). The higher number of patients with a CDR global score of 0.5 (indicating milder impairment in the range of MCI) in CLARITY-AD (80.8%) compared with TRAILBLAZER-ALZ 2 (65.7%) may explain the smaller effect of lecanemab given the lower sensitivity of change of the CDR-SOB in MCI compared with mild dementia.
A different way to interpret the effect size is a time-to-event analysis, which is common in other medical fields, such as oncology. The hazard ratios (HR) of progressing to a more severe clinical stage (MCI to mild dementia, mild dementia to moderate dementia based on CDR ratings) within 18 months were 0.69 for lecanemab (risk reduction of 31%) and 0.61 for donanemab in the low to medium tau group (risk reduction of 39%) (full sample: 0.63) (9, 11). From the societal point of view, this risk reduction is important given the increase of care-related costs with advancing disease stages. For comparison with other fields of medicine, a recent meta-analysis across 92 FDA-approved anti-cancer drugs reported a HR for progression-free survival of 0.52 (16).
Complementary approaches of assessing meaningfulness are patient-reported outcome measures (PROM). In CLARITY-AD, self- and care partner-reported quality of life and caregiver burden were assessed. Significant superiority of lecanemab was observed in all three domains (17).
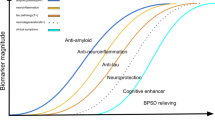
Expected effect sizes of new treatments
AD is a highly complex disease with several relevant molecular pathways beyond β-amyloid and tau aggregation. A recent genome-wide association study (GWAS) identified 75 significant risk loci. A pathway analysis revealed 33 significant gene sets and identified a strong role of the innate immune system and microglia-dependent endocytosis (18). In addition, AD pathology is driven by environmental and lifestyle risk factors as well as general mechanisms of aging. Consequently, current drug development has extended to inflammation, metabolic regulation, oxidative stress, synaptic protection, neurotransmitter imbalance and proteostasis complementary to β-amyloid aggregation and tau pathology (10). Given the multifaceted causes underlying AD and the fact that at the time of symptom manifestation, the disease pathology has already progressed for several years, it is not very likely that targeting a single molecular mechanism at the stage of early symptomatic AD will have much stronger effects than what is now observed in β-amyloid-targeting antibody trials. Larger effects will most likely only be achieved by combination therapies, individualized biomarker-guided patient selection, and by long-term treatment from the very early disease stage onwards. This assumption clearly suggests that the progress in treatments will be incremental and, given the long duration of trials needed in AD will extend over many years.
Side effects of β-amyloid-targeting antibodies
The most discussed side effects of the current β-amyloid-targeting treatments are amyloid-related imaging abnormalities (ARIA), which are changes observed on magnetic resonance imaging (MRI). They are classified as ARIA-E and ARIA-H. The first refers to hyperintense signal abnormalities with evidence of brain swelling on T2-weighted MRI. ARIA-E is considered to reflect vasogenic edema due to antibody effects on amyloid in vascular walls often accompanying AD pathology (19). ARIA-H describes microbleeds or superficial siderosis also considered to be related to cerebral amyloid angiopathy (CAA) and CAA-related inflammation (CAA-ri) (20, 21). In the trials, the occurrence of ARIA led to discontinuation and re-start of dosing following specific protocols.
A recent summary of ARIA related to lecanemab treatment in CLARITY AD including the open label extension study reported an ARIA-E frequency of up to 34.5% in APOE4 homozygous with 14.2% being recurrent (6.5% and 0.8% in APOE4 non-carriers). 92% occurred in the first six months of treatment, 81% resolved within four months. The frequency of symptomatic ARIA-E was 3.3% (11.2% in APOE4 homozygous) with mild to moderate and transient symptoms including headache, confusion, dizziness, vision changes, nausea, aphasia and weakness. Individual cases of seizure were reported in association with ARIA, however, the frequency of seizures in lecanemab-treated patients was the same as in the placebo group (0.6%) (22). In APOE4 homozygous the frequency of ARIA-H was 39.8% in lecanemab-treated group and in 21.1% in the placebo group (11.9% and 3.8% in APOE4-non-carriers). Of all lecanemab-treated patients, 1.7% showed symptomatic ARIA-H. Intracerebral hemorrhage occurred in 0.5% (8 of 1612) of lecanemab-treated cases and in 0.1% (1 of 897) of the placebo group, of which two in the lecanemab group and one in the placebo had fatal outcomes. Of the two fatal cases under lecanemab, one received tissue plasminogen activator (tPA) treatment before the hemorrhage and one received anticoagulant therapy (22).
In TRAILBLAZER-ALZ 2, ARIA-E occurred in 40.6% of APOE4 homozygous (15.7% in non-carriers). 6.1% of all donanemab-treated patients had symptomatic ARIA-E (25.4% of all ARIA-E cases). First events of ARIA-E resolved in 98% of the cases after a mean of 72.4 days. ARIA-H was observed in 36.4% of all treated patients and 13.6% in the placebo group. Intracranial hemorrhage occurred in 0.4% of treated cases (3 of 853) in 0.2% in the placebo group (2 of 874). Three participants in the donanemab group died in relation to severe ARIA-E (n=1), severe ARIA-E and ARIA-H (n=1) and severe ARIA-E and ARIA-H with intracranial hemorrhage (n=1). Two were APOE4 heterozygous carriers and one was an APOE4 non-carrier. None had received anticoagulant or anti-platelet medications (11).
These data show that ARIA-E and ARIA-H are common, particularly in APOE4 carriers. They also show that transient clinical symptoms of mild to moderate severity occur in a fraction of all ARIA cases. Severe clinical side effects even with fatal outcome occur in very rare cases. Every effort must be taken to understand the underlying mechanisms of these severe events. Risk factors for ARIA must be known to prescribing physicians, and biomarker, which indicate ARIA-risk are highly desirable (22). However, the trials also demonstrate that with careful monitoring ARIA are manageable and patient can generally be treated safely. In our view, the perception that β-amyloid-targeting treatment with antibodies puts patient at high risk for dangerous side effect is not supported by data and misleading.
Eligibility for treatment
In the United States (US) appropriate use recommendations (AUR) for aducanumab and lecanemab have been published to guide the clinical use of these antibodies with special consideration of patient selection and safety monitoring (23, 24). In addition to the proof of AD pathology by biomarkers in mildly symptomatic patients, the AURs list several eligibility criteria, which are oriented along the inclusion and exclusion criteria as well as safety findings of the clinical trials (9, 10). Key aspects are the level of impairment as defined by cognitive testing, co-medication, and eligibility for safety monitoring (i.e. lack of MRI contraindications).
A number of reports have estimated the proportion of individuals who would qualify for treatment. In the Mayo Study of Aging, 5.1%–17% of 237 patients with MCI or mild dementia and evidence for Aβ pathology were found to be eligible depending on the compound and the neuropsychological criteria used (25). In an analysis of the Karolinska Memory Clinic sample 27% of MCI cases and 28% of dementia cases would qualify for aducanumab treatment without consideration of MR-based exclusion criteria (26). An analysis of the database of the Centre for Dementia and Cognitive Decline (CDCD) in Brecia revealed 32.6% of with MCI patients to be potentially eligible for aducanumab treatment (27). Based on National Health Service data, it was estimated that 30.200 patients (3.1% of all dementia cases) would qualify for antibody treatment in the UK (28). These estimates show that among those patients at the early symptomatic stage of AD, only a fraction is eligible for the currently available β-amyloid-targeting antibodies.
Access barriers
The identification of early-stage AD patients potentially eligible for amyloid-targeting treatment requires vigilance from patients, family members and physicians for early symptoms. While there is a general openness in primary care for early diagnosis, many barriers exist for early case finding. Frequent topics hindering early diagnosis at the non-specialized level include lack of time and knowledge about early AD as well as insufficient reimbursement (29). There is a substantial need to develop tools which allow correct detection of MCI and mild dementia in the non-specialized settings and to create an environment, in which the primary care physician is supported in the diagnostic process, counseling and care for patients with early-stage AD. A second barrier to early diagnosis of AD is access to an expert diagnosis including evaluation of CSF or PET biomarkers. The necessary capacities for diagnostics currently exceed what is available in almost all European countries (30). Plasma-based biomarkers may help to overcome challenges of diagnostic capacity in the future, but expert centers guiding the diagnostic process will still be required and present a bottleneck. With regard to treatment, infusion center capacity is a limiting factor. An additional challenge is the requirement of MRI side effect monitoring with five and - in case of ARIA - potentially even morse scans within the first year of treatment and additional scans subsequently, which is needed to guide dosing decisions including even cessation of treatment. As such, access to repeated MRI represents another bottleneck, which needs to be overcome in order to make effective treatment available.
Besides eligibility criteria and structural barriers of access other aspects will most likely impact on the number of patients eventually receiving treatment. Of relevance will be for instance the risk/benefit/effort/cost considerations of individual patients and care partners after the informed-consent process, lack of knowledge about new treatments on the level of patients and physicians, skepticism of consulting physician including recommendation against treatment, long distance or complicated traveling to facilities, out-of-the-pocket expenses in some healthcare systems and many other. All of these aspects most likely contribute to the lower than expected number of treated patients currently observed in the US, where antibodies are approved.
Costs related to treatment
There has been a concern that the costs of diagnostics, treatment and monitoring per patient with the current β-amyloid-targeting antibodies will exceed the capacity of national health care systems. In a previous EADC paper, we concluded that the economic consequences would be considerable, if one third of the early AD-population would get access to treatment (31). Given the consideration above, however, all cost models carry uncertainties, because the real number of individuals who will be treated is difficult to estimate before the compounds enter healthcare.
In addition, prospective developments of treatments will potentially lower the costs. For example, subcutaneous application of antibodies, which is under development, will make infusion centers dispensable; treatment only until amyloid negativity, which was reached in 80% of all patients in the TRAILBLAZER-ALZ 2 trial after 18 months, would limit treatment duration per patient (for this, meaningful blood biomarkers for treatment-related amyloid lowering are needed); improvement in anti-amyloid treatment with regard to ARIA risk may make MRI-monitoring in the future unnecessary.
Conclusion and outlook
With the advent of β-amyloid targeting treatments as the first generation of causal treatment of AD and the rapidly evolving biomarkers, the field of neurodegenerative diseases is entering a new era, which for the first time holds promise for effectively slowing the biological disease processes and eventually preventing severe clinical disease stages which are associated with high burden and costs of care. The complex biological nature of AD and other neurodegenerative diseases implies that the clinical effects of single-target treatments starting at the symptomatic stage of the disease will most likely be limited. We expect upcoming mono-targeted non-amyloid treatments to achieve effect sizes comparable to those of lecanemab and donanemab. It is likely that significantly stronger effects will only be achieved by combination therapies, by individualized biomarker-guided patient selection or by much earlier treatments. All these approaches require trial designs, which are more complex than the recent phase 3 clinical trials. Their development will need to build on current clinical trial evidence, but also capitalize on experience and knowledge gained by clinical use. Overall, the progress towards larger effect sizes will most likely be incremental and extend over several years. It is of critical importance for the research community as well as regulators, payers and the public to acknowledge these expectations. To eventually achieve the best outcome, we need strong and sustained investments in research and in the development of health care systems with the integration of innovations. We need to establish technologies and pathways of care that allow timely identification of patients who are eligible for and may benefit from these treatment and guarantee access to safe administration and monitoring. As in other fields, we must make use of real-world data collected in large-scale registries to better understand effects and risk of the upcoming treatments. With sustained commitment of all stakeholders, the field of neurodegenerative diseases will eventually evolve from symptomatic dementia care to early disease detection with effective causal treatment and delay or even prevention of late stage disease leading to reduced care dependency and cost savings for the society.
References
Jönsson L, Tate A, Frisell O, Wimo A. The Costs of Dementia in Europe: An Updated Review and Meta-analysis. Pharmacoeconomics 2023;41:59–75. doi: https://doi.org/10.1007/s40273-022-01212-z.
Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020;396:413–446. doi: https://doi.org/10.1016/S0140-6736(20)30367-6.
Wolters FJ, Chibnik LB, Waziry R, et al. Twenty-seven-year time trends in dementia incidence in Europe and the United States: The Alzheimer Cohorts Consortium. Neurology 2020;95:e519–e531. doi: https://doi.org/10.1212/WNL.0000000000010022.
DeTure MA, Dickson DW. The neuropathological diagnosis of Alzheimer’s disease. Mol Neurodegener 2019;14:32. https://doi.org/10.1186/s13024-019-0333-5.
Hansson O, Blennow K, Zetterberg H, Dage J. Blood biomarkers for Alzheimer’s disease in clinical practice and trials. Nat Aging 2023;3:506–519. doi: https://doi.org/10.1038/s43587-023-00403-3
Perneczky R, Hansen N, Hofmann A, et al. Diagnostic Tools Working Group. Blood-Based Biomarkers for Early Alzheimer’s Disease Diagnosis in Real-World Settings. Methods Mol Biol 2024;2785:3–14. doi: https://doi.org/10.1007/978-1-0716-3774-6_1.
Sevigny J, Chiao P, Bussière T, et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature 2016;537:50–6. doi: https://doi.org/10.1038/nature19323.
Budd Haeberlein S, Aisen PS, Barkhof F, et al. Two Randomized Phase 3 Studies of Aducanumab in Early Alzheimer’s Disease. J Prev Alzheimers Dis 2022;9:197–210. doi: https://doi.org/10.14283/jpad.2022.30.
van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in Early Alzheimer’s Disease. N Engl J Med 2023;388:9–21. doi: https://doi.org/10.1056/NEJMoa2212948.
Cummings J, Zhou Y, Lee G, Zhong K, Fonseca J, Cheng F. Alzheimer’s disease drug development pipeline: 2024. Alzheimers Dement (N Y) 2024 Apr;10:e12465. doi: https://doi.org/10.1002/trc2.12465. PMID: 38659717
Sims JR, Zimmer JA, Evans CD, et al. Donanemab in Early Symptomatic Alzheimer Disease: The TRAILBLAZER-ALZ 2 Randomized Clinical Trial. JAMA 2023;330:512–527. doi: https://doi.org/10.1001/jama.2023.13239.
Morris JC. Clinical dementia rating: a reliable and valid diagnostic and staging measure for dementia of the Alzheimer type. Int Psychogeriatr 1997;9 Suppl 1:173–176. doi: https://doi.org/10.1212/wnl.48.6.1508.
Wessels AM, Rentz DM, Case M, Lauzon S, Sims JR. Integrated Alzheimer’s Disease Rating Scale: Clinically meaningful change estimates. Alzheimers Dement (N Y) 2022;8:e12312. doi: https://doi.org/10.14283/jpad.2015.82.
Andrews JS, Desai U, Kirson NY, Zichlin ML, Ball DE, Matthews BR. Disease severity and minimal clinically important differences in clinical outcome assessments for Alzheimer’s disease clinical trials. Alzheimers Dement (N Y) 2019;5:354–363. doi: https://doi.org/10.1016/j.trci.2019.06.005.
Lansdall CJ, McDougall F, Butler LM, et al. Establishing Clinically Meaningful Change on Outcome Assessments Frequently Used in Trials of Mild Cognitive Impairment Due to Alzheimer’s Disease. J Prev Alzheimers Dis 2023;10:9–18. doi: https://doi.org/10.14283/jpad.2022.102.
Ladanie A, Schmitt AM, Speich B, et al. Clinical Trial Evidence Supporting US Food and Drug Administration Approval of Novel Cancer Therapies Between 2000 and 2016. JAMA Netw Open 2020;3:e2024406. doi: https://doi.org/10.1001/jamanetworkopen.2020.24406.
Cohen S, van Dyck CH, Gee M, et al. Lecanemab Clarity AD: Quality-of-Life Results from a Randomized, Double-Blind Phase 3 Trial in Early Alzheimer’s Disease. J Prev Alzheimers Dis 2023;10:771–777. doi: https://doi.org/10.14283/jpad.2023.123.
Bellenguez C, Küçükali F, Jansen IE, et al. New insights into the genetic etiology of Alzheimer’s disease and related dementias. Nat Genet 2022;54:412–436. doi: https://doi.org/10.1038/s41588-022-01024-z.
Söderberg L, Johannesson M, Gkanatsiou E, et al. Amyloid-beta antibody binding to cerebral amyloid angiopathy fibrils and risk for amyloid-related imaging abnormalities. Sci Rep 2024;14:10868. doi: https://doi.org/10.1038/s41598-024-61691-2.
Hampel H, Elhage A, Cho M, Apostolova LG, Nicoll JAR, Atri A. Amyloid-related imaging abnormalities (ARIA): radiological, biological and clinical characteristics. Brain 2023;146:4414–4424. doi: https://doi.org/10.1093/brain/awad188.
Piazza F, Caminiti SP, Zedde M, et al. Association of Microglial Activation With Spontaneous ARIA-E and CSF Levels of Anti-Aβ Autoantibodies. Neurology 2022;99:e1265–e1277. doi: https://doi.org/10.1212/WNL.0000000000200892.
Honig LS, Sabbagh MN, van Dyck CH, et al. Updated safety results from phase 3 lecanemab study in early Alzheimer’s disease. Alzheimers Res Ther 2024;16:105. doi: https://doi.org/10.1186/s13195-024-01507-7.
Cummings J, Rabinovici GD, Atri A, et al. Aducanumab: Appropriate Use Recommendations Update. J Prev Alzheimers Dis 2022;9:221–230. doi: https://doi.org/10.14283/jpad.2022.34.
Cummings J, Apostolova L, Rabinovici GD, et al. Lecanemab: Appropriate Use Recommendations. J Prev Alzheimers Dis 2023;10:362–377. doi: https://doi.org/10.14283/jpad.2023.30.
Pittock RR, Aakre JA, Castillo AM, et al. Eligibility for Anti-Amyloid Treatment in a Population-Based Study of Cognitive Aging. Neurology 2023;101:e1837–e49. doi: https://doi.org/10.1212/WNL.0000000000207770.
Rosenberg A, Ohlund-Wistbacka U, Hall A, et al. Beta-Amyloid, Tau, Neurodegeneration Classification and Eligibility for Anti-amyloid Treatment in a Memory Clinic Population. Neurology 2022;99:e2102–e13. doi: https://doi.org/10.1212/WNL.0000000000201043.
Padovani A, Caratozzolo S, Rozzini L, Pilotto A, Benussi A, Tedeschi G. “Real-world” eligibility for aducanumab depends on clinical setting and patients’ journey. J Am Geriatr Soc 2022;70:626–628. doi: https://doi.org/10.1111/jgs.17530.
Laurell AAS, Venkataraman AV, Schmidt T, et al. Estimating demand for potential disease-modifying therapies for Alzheimer’s disease in the UK. Br J Psychiatry 2024;224:198–204. doi: https://doi.org/10.1192/bjp.2023.166.
Sannemann L, Müller T, Waterink L, et al. General practitioners’ attitude toward early and pre-dementia diagnosis of AD in five European countries-A MOPEAD project survey. Alzheimers Dement (Amst) 2021;13:e12130. doi: https://doi.org/10.1002/dad2.12130.
Hlavka JP, Mattke S, Liu JL. Assessing the Preparedness of the Health Care System Infrastructure in Six European Countries for an Alzheimer’s Treatment. Rand Health Q 2019;8(3). PMID: 31205802; PMCID: PMC6557037.
Jönsson L, Wimo A, Handels R, et al. The affordability of lecanemab, an amyloid-targeting therapy for Alzheimer’s disease: an EADC-EC viewpoint. Lancet Reg Health Eur 2023;29:100657. doi: https://doi.org/10.1016/j.lanepe.2023.100657.
Acknowledgment
The EDAC is the network of leading national academic memory centers in Europe (https://eadc.online). 45 representatives of EADC centers from 18 European countries contributed to this position statement. Many EADC centers have clinical trials experience with β-amyloid-targeting antibodies.
Funding
Funding note: Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest disclosure: D. Aarsland reports personal fees for advice and lectures from Eisai, Biogen, Eli Lilly, EIP Pharma, Roche Diagnostics, Sanofi, and Heptares, and grants from Roche Diagnostics, Sanofi and Evonik. D. Angioni reports being an investigator in clinical trials sponsored by Alector, Alzheon, Biogen, Eisai, Genentech, Green Valley, Hoffmann-La Roche, Janssen, Medesis Pharma, Nestle, Novo Nordisk, Otsuka, Regenlife, Toulouse University Hospital, and UCB Pharma. No direct personal benefit. M. Balasa reports no conflict of interest. M. Boban reports no conflict of interest. K. Bennys reports grants form Alzheon Inc, Araclon Biotech S.L., Biogen, Eisai, Roche Genentech. No personal fees. M. Boada reports fees for advice from Grifols, Araclon, Biotech, Roche, Biogen, Lilly, Merck, Zambon, Novo Nordisk, Bioiberica, Eisai, Servier, and Schwabe Pharma; fees for lectures from Roche, Biogen, Grifols, Nutricia, Araclon Biotech, Servier, and Novo Nordisk. A. Chincarini reports no conflict of interest. S. Engelborghs reports fees from Eisai, icometrix, Novartis, Roche all paid to institution, and personal fees from Roche and Biogen. L. Exalto received personal fees from Julius Clinical and Brain Research Center. A. Felbecker reports personal fees for advisory boards and lectures from Eisai, Eli Lilly, Schwabe Pharma AG, Ompharma, Roche Pharma, Specialty care Therapiezentren AG, and grants from Fujirebio. K. Fliessbach reports no conflict of interest. G.B. Frisoni reports funding through the Private Foundation of Geneva University Hospitals from: A.P.R.A. – Association Suisse pour la Recherche sur la Maladie d’Alzheimer, Genève; Fondation Segré, Genève; Ivan Pictet, Genève; Race Against Dementia Foundation, London, UK; Fondation Child Care, Genève; Fondation Edmond J. Safra, Genève; Fondation Minkoff, Genève; Fondazione Agusta, Lugano; McCall Macbain Foundation, Canada; Nicole et René Keller, Genève; Fondation AETAS, Genève. He has received funding through the University of Geneva or Geneva University Hospitals: for IISSs from ROCHE Pharmaceuticals OM Pharma EISAI Pharmaceuticals Biogen Pharmaceuticals and Novo Nordisk; for competitive research projects from: H2020, Innovative Medicines Initiative (IMI), IMI2, Swiss National Science Foundation, and VELUX Foundation as well as payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from: Biogen, Roche, Novo Nordisk, GE HealthCare, all through the institution. A.J. Garza-Martinez reports no conflict of interest. T. Grimmer reports consulting fees from AbbVie, Advantage Therapeutics Alector, Anavex, Biogen, BMS, Cogthera, Iqvia, Noselab, NuiCare, Orphanzyme Eisai, Eli Lilly, Functional Neuromodulation, Grifols, Janssen, Novo Nordisk, Roche Pharma, UCB, and Vivoryon, and lecture fees from Biogen, Eisai, Grifols, Medical Tribune, Schwabe, Synlab, Novo Nordisk, and Roche Pharma. Her served as Principal Investigator in drug trials by AbbVie, Advantage Therapeutics, Alector, Anavex, Biogen, Eli Lilly, Functional Neuromodulation, Roche Pharma, UCB, and Vivoryon; The Institution received payment for study performance. Further grants to his institution from: Biogen and Eisai and Roche Diagnostics. L. Froelich reports grants and personal fees for lectures and advice from Roche, and personal fees for lectures and advice from Eisai, Araclon/Grifols, Eli Lilly, Noselab, NovoNordisk, BioVie, Biogen, MerckSharpe&Dohme, Neurimmune, TauRX, Dr. Willmar Schwabe Otsuka/Avanir, Axon Neuroscience, Pharmatropix, Neuroscios, Vivoryon, Hummingbird, Anavex, and Boehringer Ingelheim. B. Hanseeuw reports personal fees for advice and lectures from Eisai, Roche, Biogen, and grants from Fonds National de la Recherche Scientifique, Fondation Stop Alzheimer, and WEL Research institute (WELBIO). J. Hort reports consulting and lecture fees from Schwabe, Eisai, and Eli Lilly and holds stock options in Alzheon. A. Ivanoiu reports no conflict of interest. F. Jessen has reports honoraria for advisory boards and presentations from Abbvie, AC immune, Biogen, Eli Lilly, Eisai, GE Healthcare, Grifols, Janssen-Cliag and Roche. L. Krajcovicova reports no conflict of interest. S. Klöppel reports fees for advice and lectures from Biogen, Eisai Switzerland, Lundbeck, and OM Pharma. M.G. Kramberger reports no conflict of interest. B. McGuinness reports personal fees from Eisai, Biogen, Eli Lilly, and Nutricia. P. Mecocci reports personal fees for advice and lectures from Lundbeck and Lilly, and non-financial support from Merck. A. de Mendonca reports no conflict of interest. A. Nous reports no conflict of interest. P.J. Dr. Ousset reports research grants from Acadia Pharmaceuticals, Alzheon Inc., Araclon Biotech S.L., AstraZeneca, Biogen, Avanir Pharmaceuticals, Eisai Inc., Eli Lilly, Genentech, Inc., Hoffmann-La Roche, Janssen Research & Development, Merck Sharp & Dohme, Novartis Pharmaceuticals, Shanghai Greenvalley Pharmaceutical Co., TauRx Therapeutics Ltd, UCB Biopharma without personal fee. He reports personal fees for advice from Lilly France. C. Paquet reports no conflict of interest. R. Perneczky reports personal fees for advice and lectures from Biogen, Eisai, Eli Lilly, Grifols, Novo Nordisk Roche, Schwabe, and GSK, and grants from Astra Zeneca, Roche, Janssen Cilag, Eli Lilly, and Takeda. O. Peters reports grants from Alector and Predemtec, grants and personal fees for advice and lectures from Biogen, Eisai, Roche, Noselab, and Novo Nordisk, personal fees for advice and lectures from Grifols, Lilly, Prinnovation, Medtrix, Neurolive, and Neurotransdata. F. Piazza reports consulting fees from Alector, Araclon, Alnylam, Biogen, Lilly, and Roche, and personal honoraria for advisory board membership from Roche, Araclon and Lilly. He holds a patent for the ultrasensitive quantification of anti-amyloid antibodies in human biological fluids. D. Platone reports no conflict of interest. M. Riverol reports personal fees for advice and lectures from Grifols, Nutricia and Esteve. A. Ruiz reports grants from the Instituto de Salud Carlos III (ISCIII), the European Comision-IMI program, the EU-JPND, VLAIO, Janssen, Grifols SA, Roche AG, and Araclon Biotech; and personal fees from Landstenier Genmed, Glenn Biggs Institute, UTHSA, Fundación ADEY, and Novo Nordisk. G. Sacco reports no conflict of interest. I. Santana reports grants from Biogen, and personal fees from Eisai. N. Scarmeas reports grants from NIH, and NovoNordisc. E. Solje reports personal fees from Novartis, Novo Nordisk, Eisai, and Roche and personal fees from Roche. E. Stefanova reports no conflict of interest. S. Sutovsky reports lecture fees from Eisai, Biogen, Schwabe and Krka. M. Tabuas-Pereira reports no conflict of interest. W. van der Flier reports grants from ZonMW, NWO, EU-JPND, EU-IHI, Alzheimer Nederland, Hersenstichting CardioVascular Onderzoek Nederland, Health∼Holland, Topsector Life Sciences & Health, stichting Dioraphte, Gieskes-Strijbis fonds, stichting Equilibrio, Edwin Bouw fonds, Pasman stichting, stichting Alzheimer & Neuropsychiatrie Foundation, Philips, Biogen MA Inc, Novartis-NL, Life-MI, AVID, Roche BV, Fujifilm, Eisai, Combinostics. She holds the Pasman chair. She is recipient of ABOARD, which is a public-private partnership receiving funding from ZonMW (#73305095007) and Health∼Holland, Topsector Life Sciences & Health (PPP-allowance; #LSHM20106). She is recipient of TAP-dementia (https://www.tap-dementia.nl), receiving funding from ZonMw (#10510032120003). TAP-dementia receives co-financing from Avid Radiopharmaceuticals and Amprion. All funding is paid to her institution. She reports fees to the institution for lectures from Biogen MA Inc, Danone, Eisai, WebMD Neurology (Medscape), Novo Nordisk, Springer Healthcare, and European Brain Council. She consulted the Oxford Health Policy Forum CIC, Roche, Biogen MA Inc, and Eisai. All funding is paid to her institution. WF participated in advisory boards of Biogen MA Inc, Roche, and Eli Lilly. WF is member of the steering committee of EVOKE/EVOKE+ (NovoNordisk). All funding is paid to her institution. WF is member of the steering committee of PAVE, and Think Brain Health. WF was associate editor of Alzheimer, Research & Therapy in 2020/2021. WF is associate editor at Brain. T. Welsh is Research and Medical Director of The Research Institute for the Care of Older People (RICE), Bath, UK, which runs a mixture of commercial and non-commercial research activity. Commercial research projects run in the Institute have been funded by: Lilly, Roche, Biogen, Eisai, Janssen, AC Immune, Novo Nordisk, Pfizer, Elan, Immunobrain, Actinogen, and Julius Clinical. A. Wimo report to be the License holder (part) of RUD instrument. B. Winblad reports no conflict of interest.
Rights and permissions
Open Access: This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
About this article
Cite this article
Jessen, F., Kramberger, M.G., Angioni, D. et al. Progress in the Treatment of Alzheimer’s Disease Is Needed – Position Statement of European Alzheimer’s Disease Consortium (EADC) Investigators. J Prev Alzheimers Dis (2024). https://doi.org/10.14283/jpad.2024.153
Received:
Accepted:
Published:
DOI: https://doi.org/10.14283/jpad.2024.153