Abstract
This study explores differences on health status transitions based on functional health and dead records among older population in Europe. We also study the influence of residence pattern on health changes over time. Method: Data used came from EU-SILC registers on individuals aged 50 + from 19 countries. Fixed and Mixed effect Cox Proportional Hazards Models are used to ascertain any country differences on health outcomes and then by co-residence pattern. Results: There are remarkable country heterogeneity among older people to experience changes on their health status, specially, for health improvements and mortality risk. As expected, Baltic and Eastern European countries have a higher propensity for health deterioration and Southern European countries for health improvements on their functional capacities. However, there are exceptions as Bulgaria and Romania, which have a lower risk of deterioration and death transition than average. Overall, living with partner and adult children-rather than living only with a couple shown positive effects for older European to experience health improvements with notably differences in Southern countries as in Italy and Spain. Discussion: country framework differences play a fundamental role to understand changes on health status at older ages, in particular, how health care support toward older people is managed by health systems within European countries and the availability of close relatives among older adult population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Health dynamics of older adult population are quite diverse in European countries (1, 2). Mortality has declined with varying intensities among regions, countries and by socioeconomic gradients (3–6). While the increase in extra years of remaining life expectancy were due to improvements in older adults’ health and functional status between 1970 and 2000 (7–9), nowadays Life Expectancy (LE) is reported to be stagnating in some countries and in specific ages (10, 11) when compared with the improvements observed in the 2000s.
However, there is still a debate with regard to health trends over time, as this depends on the health dimensions used, the time period under study and the population characteristics covered (12). Some studies illustrate the existence of complex interacting mechanisms for mortality and morbidity trends, including different dimensions of health (13).
Health status can be measured by a quite range of disability measures as health conditions and diseases (chronic condition and long term illness), self-perceived health (self-report about individuals perception about their health status: very good, good, fear, bad, very bad), functional limitation (which captures functioning on six life domains as cognition, mobility, self-care, getting along, life activities and participation (9, 14)). Among them, World Health Organization (WHO) recommends functional based approach to assess health status across population following the disability process as it is closely related to disability and dependence. In addition, it makes possible internationally comparable health outcomes and designing and monitoring health related interventions (15, 16). In this sense, functional limitation is defined in the International Classification of Functioning, Disability and Health (ICF) as limitation in performing physical and cognitive actions, that can be affected by environmental and personal factors that may exacerbate predisposing risk factors in the disablement process (17).
From all indicators measuring functioning, Global Activity Limitation Index (GALI) has shown great advantages as it satisfactorily assess the health status of the population in a worldwide framework (18–20). It was designed for healthy years comparisons across European countries, particularly for the estimation of Healthy Life Expectancy (HLE) (21). And, this measure is one of the three questions of the Minimal European Health Modules (MEHM) in European surveys to monitor health status across countries since 2005 (18, 22). Studies have shown that GALI is significantly associated with other function measures as Activities Daily Life (ADLs) and Instrumental Activities Daily Life limitation (IADLs) (19, 23).
Trends in functional limitations at older ages in European countries reflect pronounced inequalities. Yet, studies don’t show a clear picture about health improvements and deterioration in functioning based in longitudinal data over time. Evidence available reported similar speed of heath deterioration by gender across countries, being older women the group with higher proportion of severe activity limitation (24). Eastern countries as Poland and the Czech Rep have shown highest functional limitation incidence (64% and 49%, respectively). While most countries shown 35–40%. In severe limitations, remarkable figures were found in Southern countries as Greece and Spain with lowest rates (around 5%) in contrast to Poland (19%) (3).
Studies led by Vaupel and colleagues introduced the analysis of heterogeneity in health and mortality dynamics. Their main finding (which is of interest to this study) was that individuals experience different mortality risks based on their characteristics. They used the term “frailty” to study and model unobserved heterogeneity, particularly for older adults (24, 25). Their work also showed large dissimilarities among countries in relation with the processes of compression or expansion of mortality and health conditions. In this line, transition probabilities between health statuses based on longitudinal data are useful indicators to assess improvements or declines in functional capacities that allow to identify divergent pattern on the epidemiological trend among different population groups over time.
Moving the focus to ageing adult health, recently novel studies emphasise the importance of the functional-based approach for measuring health status at old ages. In this sense, functional ability in older population is based on the intrinsic capacity, the environment and the interactions between them. Intrinsic capacity (see Fig. 1) involves five core domains; cognitive, psycho-emotional, sensory function, vitality and locomotion. Domains that are fundamental for developing and maintaining wellbeing and an autonomous life free of dependency in later life (26).
Source: Own elaboration based on Cesari De Carvalho, Thiyagarajan et al. (2018) and Rudnicka, Napierala and Podfigurna et al. (2020)
All these factors surrounding intrinsic capacity are the framework of the individual’s life and these can be material or external environmental conditions as public areas, including environmental barriers in and surrounding home (e.g. street crossing, social and leisure facilities, public transport features, etc.) living and housing conditions (e.g. closeness to grocery shops or healthcare facilities, living in rural or urban areas, lift or stairs at home, appropriate walking areas considering people using wheel chairs, etc.) (27). Social environmental factors are considered as relationships at home (living arrangements), community and society as a whole. Contextual factors, including the social environmental ones do impact functional ability of adult people differently according to personal’s attributes such as sex, genetics, ethnicity, educational level and life style (28). For instance, the cognitive and physical capacity of a 70-year-old could be better or similar than a 50-year old person due to differential influences of a quite range of factors as health related behaviour or early living conditions. Circumstances that are considered as diversity and also inequalities. Evidence has shown that environmental factors can present barriers in engagement to healthy lifestyle as infrastructure deprivation is positive associated to risky health behaviours, loss of physical function, increased incidence of chronic diseases, between others (29).
In this framework, co-residence pattern is part of the immediate social environment in later life and it plays a fundamental role in preserving health at older ages (30) as social environmental has been considered both facilitator and constrain in mental and physical functioning in this population group (27). The lack of a partner at older ages could be detrimental for health, in particular for men as having a couple is beneficial for their wellbeing at older ages (31, 32). Yet, analysing health transitions by living arrangements has not been previously done including the effect of living with children. Furthermore, there is not concrete proof whether living arrangements are also associated with differences in (the rate of) health transitions, neither, whether those changes on health status are experienced in the same way for the older adults across European countries.
Hence, this study follows the central aim to provide evidence of the variation of health improvements and health deterioration at older ages among 19 European countries and concurrently ascertain the effect that living arrangements groups have on those health transitions. By health transition we mean health deterioration (from healthy to unhealthy), health improvements (from unhealthy to healthy) and death (from any of these two statuses: healthy or unhealthy). To analyse the effect of living arrangements on health status transitions, we apply a multilevel approach —also known as mixed effects survival modelling or shared frailty model (33)— to all three transitions separately. We further contribute to the current body of knowledge by also including countries from Eastern Europe and the former Soviet States where studies on health transition are rare.
Data and Method
Data
The data source used for this study is Eurostat’s European Union Statistics on Income and Living Conditions (EU-SILC) panel survey, which provides up-to-date comparative information of income and living conditions across countries from all parts of Europe. The source combines the use of registers with interviews in household sample surveys, providing information at individual and household level of non-institutionalised household members aged 16 and over since 2004. For this study we use information from respondents aged 50+ in panel data files, period (2004 to 2014) who were at least observed twice (see Table 1).
The EU-SILC survey has a rotational design that defines the sample in cross-sectional and longitudinal form (panel data). Specifically, the sample selection is based on a number of sub-samples or ‘replications’. For this study, the longitudinal design is used, which, permits health transitions to be estimated across four-year spells. Although Eurostat provides harmonized data across countries, variations in data collection procedures do exist among EU-SILC countries (34) (see eData1). For instance, there are countries where data collection relies on surveys with personal and proxy interviews while others also use data from administrative registers (35). Large percentages of missing and truncated data persist in EU-SILC countries that only provided register data (see eData1). Therefore, we removed countries with register data and those which reported high rates of attrition and missing data from our analysis. Countries selected were: Austria, Belgium, Bulgaria, Cyprus, the Czech Rep., Estonia, Greece, Spain, Hungary, Ireland, Italy, Latvia, Lithuania, Luxemburg, Malta, Poland, Portugal, Romania and Slovakia
Indicators used in the analysis
Dependent variable
GALI indicator was used to identify the health status of the target population: population aged 50+. It is a summary measure of functioning and is also considered a self-reported measure of participation restriction by severity level (17, 36, 37). Therefore, GALI measures health changes related to limitation in performing activities people usually do due to health problems experienced during at least the past six months. Answer categories are: 1- Yes, severely limited, 2-Yes, limited but not severely and 3- Not limited (21, 38). This indicator is considered to be a good proxy of impairment and dependence as it is used to calculate Healthy Life Expectancy (“HLE”, expected years to live in a healthy state) by Eurostat. We also choose GALI instead of self-perceived health or long standing illness indicator as the former allows us to compare our results with previous research (19, 20, 39) (see supplementary materials eData2 for further explanation of limitation). Categories 1 and 2 were grouped into one category for identifying “Unhealthy state” and “Not limited” as a “Healthy state”. For the analysis of the transition to death, personal register (Membership status: RB110) and household register (Household status: DB110) variables were used to identify the respondents who had died since the previous survey (40).
With GALI indicator and death register, three health states were identified: Healthy, Unhealthy and Death, from which four types of transitions were calculated: health deterioration (transition from healthy to unhealthy state, health improvement (from unhealthy to healthy state), death from the unhealthy state and death from the healthy state. However, we excluded the transition to death from a healthy state from the analysis, as there were too few respondents who experienced this for the results to be reliable. There are other limitations explained in supplemental material (eData2).
Control variables used
Sex, year of birth (grouped into 1924–33, 1934–43, 1944–53 and 1954–64), educational attainment (grouped into “primary or less”, “lower and upper secondary”, “post-secondary vocational and tertiary”) and country of residence.
Living arrangements indicator was based on the following variables: Household size, marital status and information on the IDs of the spouse, father and mother. Living arrangements were grouped into four categories: 1) Living with a partner (2-people household); 2) living with partner and children (which also include other co-residents in the same household, but their link could not be attained); 3) living alone (1-person household); 4) and living with others, (includes other relatives or people who shared the same household (e.g. single-parent households)).
Finally, for comparative purposes and to ease the description of the results we have grouped the selected 19 countries into four geographical-historical regions: Eastern Europe, Baltic countries, Southern Europe, and Western Europe.
Modelling strategy
We applied Mixed Effects Survival Modelling (MESM) with a Cox approach for modelling transition probability among health states (41). Methodology widely used in Epidemiology and clinical trials as treatment effects on specific diseases as cancers or progression of disease stages and recurrent infections (42, 43). Furthermore, this type of models allows to understand the association between environment factors and specific health conditions over time (44).
We started by estimating Cox Proportional Hazards models (PH) for measuring the effects of the different kinds of living arrangements on our three types of health transitions. As individuals appear in different waves, we considered possible inter-person correlation. Also, even when individuals reside in different countries, they may share common and unobserved characteristics that violate the Cox assumption of proportionality within categories of covariates (45). This is why we also estimated Mixed Effects Models (with more than one random effect), which allows modelling statistical dependence (46), and, simultaneously, consider individual-and country-level intra-correlations (see further explanation in supplementary material: eMethods1 and eMethods2).
Results
The results show that all models with random effects fit significantly better than the simple Cox PH model for each transition type considering the log-likelihood and chi square values (see eMethods2, model description and eTable1). In general terms, Cox PH ratios for living arrangements are very similar in the simplest Model (see Table 2), to the values we estimated with the models that also include random effects Model 2 y 3, but with one important difference. The main difference lies in the changes in the significance of the risks for the living arrangements categories when we take into account country-specific random effects.
The risk of health deterioration is statistically the same for older adults who live only with their partner compared with those who also co-reside with adult children according to the simple Cox PH model. However, the difference in these risks becomes significant when the country random intercepts are included (see Model 2 in Table 2). Living alone, on the other hand, does lead to a significantly higher risk of health deterioration (in all models), as they experience a 6% higher chance of worsening their health status, and living with others leads to a 3% higher risk of deterioration than older people living with their partners.
For health improvement the picture is different. Adults aged 50 and over living with a partner and adult children are 13% more likely to experience an improvement in health than those who only live with a partner. Conversely, older adults living with others and living alone are 14% and 8%, respectively, less likely to have improvements in their health status than the reference category.
For the transition to death, in comparison with older adults living with their partners, those who exclusively live with others have a remarkably 86% higher mortality risk and those who live with their partner and children a 19% higher risk. All coefficients are highly significant. As there are insufficient events in the living alone category, we discarded this transition from the multilevel model analysis.
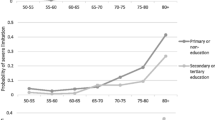
Additionally, we pointed out high differences by birth cohort groups in all health transitions types, while the results by sex and educational level are as expected; women are more likely to experience health deterioration (RR:1.13, p< 0.001) and less likely to improve their health status (RR: 0.98, p<0.01) but they have better survival (RR:0.49, p<0.001) than their male counterparts. Regarding the educational level, higher educational attainment is associated with a lower probability of health deterioration and mortality risk and a higher probability of health improvement.
Random effects among countries
Figure 2 illustrates the differences in the risks for the three transitions at the country level, according to the country sample size. The latter was included to show the effects of smaller and larger country size (e.g., Luxembourg and Spain, respectively) which could shrink or inflate the estimated risk closer to the overall mean (47).
Note: the red line represents the reference risk for each transition type (which is unknown in Cox PH) and the estimated excess risk reported by the (exponentiated) standard deviations for each country. The model controls for sex, education and birth cohort in the fixed coefficients. Mixed coefficients calculated with “survival” and “coxME” R packages; Source: Own calculation based on EU-SILC, Panel Data from 19 countries, Period 2004–2014
For health deterioration transitions, 37% of the total variance is explained by the variation between countries. For health improvements and death, the average between-countries variation is even higher (respectively, 46% y 41%). There are country effects in the risk score for deterioration transition, ranging from less than 0.7 to over 1.8 times the average risk of deterioration. As expected, older adults living in Baltic and Eastern European countries observe the highest excess of risk to experience a deterioration in their health status. Slovakia and Latvia have 1.75 times (75% higher) and Estonia a 1.45 times (45% higher) risk than the mean. Conversely, health deterioration is lowest in older people living in Bulgaria and Greece (50% lower risk than the mean).
For health improvements, country variation in the risk is slightly greater, as country effects vary from 0.5 to over twice the average. Countries with higher estimated risk of health improvements are mainly Southern European countries: Malta (2.1), followed by Luxemburg, Cyprus and Spain with excess risks estimated close to 50% more than the reference risk. On the contrary, Eastern European and Baltic countries have lower propensities for improvements than the mean. For instance, an individual living in Slovakia has approximately half the risk of experimenting health improvements than the sample average.
For death transition from unhealthy status, country effects range from less than 0.5 to 1.9 times the average risk. The model results show Baltic and Eastern European countries to have the highest excess of risk of death (Bulgaria 1.9 times the mean, Latvia and Hungary 1.5 times) and Belgium, Romania and Italy the lowest risk.
Regarding country effects on health transitions, Western European countries tend to report values close to the average risk for three health transition types, although Belgium exhibits the lowest mortality risk. On the other hand, Baltic and Eastern European countries have a higher propensity for deterioration and Southern European countries for health improvements. Several countries do not follow this regional pattern, such as Bulgaria and Romania which have a lower risk of health deterioration and death transition than average.
Spain has the average risk for mortality and health deterioration, but regarding health improvements its risk is 50% higher than the sample mean. For health improvements there are no Eastern European and Baltic countries above the mean risk, indicating a lower likelihood for older adults to improve their health status. Only Bulgaria and Latvia are close to the average risk.
For health deterioration, most Eastern European and Baltic older adults experience a higher risk (more than double in Slovakia and 50% more likely than the average in Estonia), although Bulgaria, the Czech Republic and Poland are exceptions with risks that are 20–35% lower. Conversely, the worst situation is shown for Hungary, Lithuania and Estonia. Countries which report lower health improvement and higher health deterioration and mortality risk, as well. Meanwhile striking values are reported by Slovakia and Latvia; Slovakia with the lowest risk to improve for older adults their health status (less than 50% the mean risk) and the highest risk for deterioration (more than double mean risk). Latvia with 50% higher relative risk than the average for deterioration and mortality risk.
Lastly, if we compare these results with the simple Cox PH model (see Table 2), the mean effects of living arrangements observed few changes after including the random country intercepts. In the case of health improvements, it declined slightly, most noteworthy for living with children and partner (from 13% to 10%).
This also applies to living with others in the case of the transition to death (from 1.9% to 1.8%), while living with both children and partner became significant in health deterioration (from 1% to 2%, with p<0.05). This implies that the effect of living with both children and partner contains significant country-specific differences in comparison with the reference risk (living with a partner), while living with others doesn’t.
Random effects by living arrangements within countries
There are more country differences (level 2) in the average risk of health deterioration (8%) according to living arrangements (level 1) than is the case for health improvements (5%), while there is almost no variation in the mean effect of living arrangements on mortality risk for older adults between countries.
Turning now to the differences between type of living arrangement, they are significant for health improvement and mortality risk, although associations are not in the same direction. Living with both partner and children favours health improvement for older adults, as they are 10% more likely to do so than those who only live with a partner. Nevertheless, there are country-differences as this effect is more than 5% higher in Slovakia, Italy, Ireland and Greece but 5% less likely in Luxemburg, the Czech Republic and Spain.
Conversely, older people living alone and living with others are 6% and 12%, respectively, less likely to improve their health status. The negative mean effect for living alone is less pronounced (7%) in the Czech Republic and Portugal, meaning that in those countries, older adults living alone doesn’t represent a disadvantage in health status when compared to those living with a partner. In Italy, Greece and Latvia health improvement among those living alone are the lowest. Concerning the 50+ living with others, in Poland, Malta and Bulgaria health improvements are more than 5% higher than the mean effect, while in Romania and the Czech Republic the risk is about 5% lower.
In the case of health deterioration, the only significant difference is regarding older people living alone in comparison with those living with a partner (+4%), whereby differences with the reference are particularly high in the case of the two Southern countries, Malta and Greece (+10%). On the opposite end of the scale, Romanians and Latvians living alone show the lowest risk (10% less than the average).
Discussion
This study analysis health status in 19 European countries using the European Union Statistics on Income and Living Conditions (EU-SILC) survey, through the implementation of hierarchical or mixed effects (multi-level) models on survival analysis, with the aim to describe the heterogeneity of the health changes health improvement, health deterioration and mortality among the population aged 50 years and over in 19 European countries. We also analysed the influence of living arrangements on these health dynamics and its variation between countries, with the intention of illustrating health patterns in the European context.
The results show a diverse pattern in health transitions at older ages across countries, which is slightly greater for health improvements and mortality (around 40 %) than for health deterioration (30%). In particular, Eastern European and Baltic countries tend to perform worse than Western and Southern European countries as they have higher risk of health deterioration and mortality and, as expected, are less likely to experience improvement in health. This pattern reflects trends in LE and healthy LE as reported by previous studies and national statistics (48–50).
Reasons why older people in Eastern Europe generally have a lower chance for health to improve and a higher change to deteriorate compared to the rest of Europe is well established. While prior to the fall of communism, health differences already existed as the East did not experience the onset of renewed mortality decline in the 1970s and 1980s, especially from cardiovascular mortality, as the West did, the abrupt political and economic changes that led to the collapse of its social welfare system, strained its health care system and higher levels of unhealthy behaviour, had devastating repercussions on population health (51). At the same time, most Southern European countries converged and even surpassed the levels of LE recorded in Western and Northern Europe.
Our results, however, did show some notable exceptions for the period under study (2004–14). In particular, the 50+ in the Czech Republic, Bulgaria and Poland observed a lower propensity of health deterioration than the European average, with levels similar to Belgium and Greece. Likewise, the risk of death in Romania is lower than average and similar to Italy and Portugal. These results are in line with recent mortality reversal in Central Europe driven by improvements in health behaviour and health care (52, 53). The Czech Republic pioneered this trend, followed by Poland and Slovenia Slovakia, Hungary and Estonia and more recently (but still lagging behind by a great margin) by Russia, Ukraine and the remaining Baltic States (52, 54).
Health transition probabilities —whether it pertains to an improvement or a deterioration or death— differ not only between but also within countries. We therefore examined differences according to living arrangement, controlling for age, sex and educational attainment, as there are still notable country differences in intergenerational co-residence in Europe. Results show that older adults living with a couple and living with partner and children have the same probability of health deterioration, while in the case of health improvements, the latter group has a higher chance to improve their health condition. Others living arrangements show a lower chance of health improvements compared to those only living with a couple. These findings therefore support others who found that the influence of family resources, in particular living with partner and older children, is beneficial in the wellbeing of older people with health problems (55). Nevertheless, there is possibility of a selection effect on the health status of those who live with their partner and children as they may have chosen this living arrangement because of bad health. Although this could lead to an overestimation of the risk of health deterioration, this is not observed. On the contrary, results show that the presence of a co-residing partner and children leads to a greater probability of recovery and an equal probability of health deterioration compared to those who live only with a partner. Therefore, we can rule out a selection effect on the state of health in this living arrangements group.
Surprisingly, Southern European countries showed the most diverse pattern of health changes according to the co-residence pattern. This is perhaps unexpected given certain cultural, economic and political similarities between the countries, including a similar profile of (multigenerational) living arrangements, proportion of older adults people in the population and a lack of state support regarding long-term older adults care (56). For instance, Spain and Italy are on the opposite spectrum in terms of the probability of experiencing health improvement when living with a partner and children as Italy reported a 10% higher than average chance and Spain a 7% lower chance. Concurrently, for those living alone, results were also the opposite. Likewise, some countries in Eastern Europe are also atypical. Older people living with their partner and children in Slovakia showed more propensity (5–10%) to improve their health status than the overall risk, as did people living alone in the Czech Republic. While future research should look into finding factors that could provide an explanation for these patterns, in countries with strong family ties, older people increase the likelihood of improving their health status when living with their children, as is clearly the case in Italy. However, it does not protect against health deterioration or lead to an increase in health improvements in other Southern European countries.
Conclusion and Recommendations
Our results showned evidence of complex interactions between country frameworks and the influence of living arrangements on health dynamics. Country profiles play a fundamental role on how residence pattern affect and moderate health improvements and deterioration rather than mortality risk at older ages, as more co-residence-variation was reported in the transition to health deterioration (8%) and for health improvement (5%). This also reflects country differences in the composition by living arrangement (57, 58), how health care policies are addressed to older population (59), availability of children and the type of help that is provided to older adults, which is likely related to the age of adult children (60).
While current official statistics show increases in life expectancy in European countries (48), major challenges are concentrated in improving functional abilities at older ages. Policy strategies across European countries for a healthy ageing should prioritize friendly environments and integration initiatives with an ecological approach in later life to improve the intrinsic capacities of older individuals and mitigate social inequalities (28, 61). Strategies should also consider: lifelong prevention programmes promoting healthy behaviours (exercising, social participation, learning activities focused on third age, etc.), interventions for reducing barriers to get access to healthcare including enough geriatrics and physicians according to the population size of older people at community level, and implementing health-related social initiatives that integrate older adults, their families and community.
References
McEniry M. Early Life Conditions and Rapid Demographic Changes in the Developing World. Early Life Cond Rapid Demogr Chang Dev World Consequences Older Adult Health. 2014;9789400769:1–216. Available from: http://www.scopus.com/inward/record.url?eid=2-s2.0-84928853533&partnerID=tZOtx3y1
Siegel JS. The Demography and Epidemiology of Human Health. Chicago Illinois, USA: Springer; 2012.
Jagger C, Weston C, Cambois E, Van Oyen H, Nusselder W, Doblhammer G, et al. Inequalities in health expectancies at older ages in the European Union: findings from the Survey of Health and Retirement in Europe (SHARE). J Epidemiol Community Health. 2011;65(11):1030–5. doi: https://doi.org/10.1136/jech.2010.117705
Cambois E, Solé-Auró A, Robine J-MJ, Sole-Auro A, Robine J-MJ. Economic Hardship and Educational Differentials in Disability in 26 European Countries. J Aging Health. 2016;28(7):1214–38. doi: https://doi.org/10.1177/0898264316656503
Caselli G, Vallin J, Wunsch G. Demography: Analysis and Synthesis. A Treaties in Population. 2006. 2857 p.
Robine J-M, Saito Y, Jagger C. The relationship between longevity and healthy life expectancy. Qual Ageing Older Adults. 2009;10(2):5–14. doi: https://doi.org/10.1108/14717794200900012
Beltrán-Sánchez H, Preston SH, Canudas-Romo V. An integrated approach to cause-of-death analysis: cause-deleted life tables and decompositions of life expectancy. Stat Methods Med Res. 2009;18(2):195–222.
Crimmins EM, Beltrán-sánchez H. Mortality and Morbidity Trends: Is There Compression of Morbidity? 2010;75–86.
Goldstein S, Naglieri JA. Assessing Impairment. 2016. Springer. E-book. doi: https://doi.org/10.1007/978-1-4899-7996-4
Lindahl-Jacobsen R, Rau R, Jeune B, Canudas-Romo V, Lenart A, Christensen K, et al. Rise, stagnation, and rise of Danish women’s life expectancy. Proc Natl Acad Sci. 2016;113(15):4015–20. doi: https://doi.org/10.1073/pnas.1602783113
Romo VC, Engelman M. Maximum life expectancies: Revisiting the best practice trends. Genus. 2009;65(1):59–79.
Crimmins EM. Trends in the Health of the Elderly. Annu Rev Public Heal. 2004
Tomassini C, Glaser K, Wolf DA, Broese van Groenou MI, Grundy E. Living arrangements among older people: an overview of trends in Europe and the USA. Popul Trends. 2004
Rueda-Salazar S, Spijker J, Devolder D, Albala C. The contribution of social participation to differences in life expectancy and healthy years among the older population: A comparison between Chile, Costa Rica and Spain. Navaneetham K, editor. PLoS One. 2021 Mar 12;16(3):e0248179. https://doi.org/10.1371/journal.pone.0248179
World Health Organization. Towards a common language for functioning, disability and health: ICF. Int Classif. 2002;1149:1–22. Available from: http://www.who.int/classifications/icf/training/icfbeginnersguide.pdf
WHO. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule WHODAS 2.0. Üstün, N Kostanjsek, S Chatterji JR, editor. World Health Organization. Malta: WHO Library Cataloguing-in-Publication Data Measuring; 2010. 152 p. Available from: https://apps.who.int/iris/handle/10665/43974
Verbrugge LM, Jette AM. The Disablement Process. Sm Sci Med. 1994;38(1):48109–2007. https://doi.org/10.1016/j.jmatprotec.2007.03.111
Berger N, Robine J-M, Ojima T, Madans J, Van Oyen H. Harmonising summary measures of population health using global survey instruments. J Epidemiol Community Health. 2016 Oct 1;70(10):1039–44. https://doi.org/10.1136/jech-2015-206870
Bogaert P, Van Oyen H, Beluche I, Cambois E, Robine JM. The use of the global activity limitation Indicator and healthy life years by member states and the European Commission. Arch Public Heal. 2018 Jun 28;76(1). https://doi.org/10.1186/s13690-018-0279-z
Van Oyen H, Bogaert P, Yokota RTC, Berger N. Measuring disability: a systematic review of the validity and reliability of the Global Activity Limitations Indicator (GALI). Arch Public Heal. 2018 Dec 28;76(1):25. https://doi.org/10.1186/s13690-018-0270-8
Jagger C, Gillies C, Cambois E, Van Oyen H, Nusselder W, Robine JM. The Global Activity Limitation Index measured function and disability similarly across European countries. J Clin Epidemiol. 2010;63(8):892–9. https://doi.org/10.1016/j.jclinepi.2009.11.002
EUROSTAT. Global Activity Limitation Indicator (GALI) as a core variable. Meeting of the European Directors of Social Statistics, Luxembourg; 2015. Available from: https://circabc.europa.eu/sd/a/8eec189a-3389-47d3-999e-c12afc4a0f7d/DSS-2015-Sep-04.3 GALI as a core variable.pdf
Charafeddine R, Berger N, Demarest S, Van Oyen H. Using mortality follow-up of surveys to estimate social inequalities in healthy life years. Popul Health Metr. 2014 Dec 12;12(1):13. https://doi.org/10.1186/1478-7954-12-13
Scherbov S, Weber D. Future trends in the prevalence of severe activity limitations among older adults in Europe: a cross-national population study using EU-SILC. BMJ Open. 2017 Sep 23;7(9):e017654. https://doi.org/10.1136/bmjopen-2017-017654
Vaupel JW, Manton KG, Stallard E. The Impact of Heterogeneity in Individual Frailty on the Dynamics of Mortality. Demography. 1979;16(3):439. https://doi.org/10.2307/2061224
Yashin AI, Manton KG, Vaupel JW. Mortality and aging in a heterogeneous population: A stochastic process model with observed and unobserved variables. Theor Popul Biol. 1985;27(2):154–75. https://doi.org/10.1016/0040-5809(85)90008-5
Cesari M, Araujo de Carvalho I, Amuthavalli Thiyagarajan J, Cooper C, Martin FC, Reginster J-Y, et al. Evidence for the Domains Supporting the Construct of Intrinsic Capacity. Journals Gerontol Ser A. 2018 Nov 10;73(12):1653–60. https://doi.org/10.1093/gerona/gly011
Annear M, Keeling S, Wilkinson T, Cushman G, Gidlow B, Hopkins H. Environmental influences on healthy and active ageing: a systematic review. Ageing Soc. 2014 Apr 6;34(4):590–622. https://doi.org/10.1017/S0144686X1200116X
Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020;139(February):6–11. https://doi.org/10.1016/j.maturitas.2020.05.018
Kooiker S, Christiansen T. Inequalities in health: the interaction of circumstances and health related behaviour. Sociol Heal Illn. 1995 Sep;17(4):495–524. https://doi.org/10.1111/1467-9566.ep10932690
Henning-Smith C, Shippee T, Capistrant B. Later-Life Disability in Environmental Context: “Why Living Arrangements Matter. Gerontologist. 2018 Sep 14;58(5):853–62. https://doi.org/10.1093/geront/gnx019
Herm A, Anson J, Poulain M. Living arrangements and marital status: a register-based study of survival of older adults in Belgium at the beginning of the 21st century. Ageing Soc. 2016 Nov 7;36(10):2141–62. https://doi.org/10.1017/S0144686X15001002
Grundy EMD, Tomassini C. Marital history, health and mortality among older men and women in England and Wales. BMC Public Health. 2010 Dec 15; 10(1):554. https://doi.org/10.1186/1471-2458-10-554
Yashin AI, Vaupel JW, Iachine IA. Correlated individual frailty: An advantageous approach to survival analysis of bivariate data. Math Popul Stud. 1995 Mar;5(2):145–59. https://doi.org/10.1080/08898489509525394
EUROSTAT. EU Statistics on Income and Living Conditions (EU-SILC). eurostat explained. 2016 [cited 2017 May 10]. Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=EU_statistics_on_income_and_living_conditions_(EU-SILC)_methodology_—_data_collection#Mode_of_data_collection
Jäntti M, Törmälehto V-M, Marlier E. The use of registers in the context of EU—SILC: challenges and opportunities. Eurostat, editor. 2013. (Collection: Statistical working papers). Report No.: Theme 3: Population and social conditions. https://doi.org/10.2785/45854
Robine J-M, Jagger C, Mathers CD, Crimmins EM, Suzman RM. Determining Health Expectancies. Robine J-M, Jagger C, Mathers CD, Crimmins EM, Suzman RM, editors. Chichester, UK: John Wiley & Sons, Ltd; 2002. 444 p. https://doi.org/10.1002/0470858885
ELHEIS. Health questions from the Minimum European Health Module used in EU-SILC in the 27 EU countries. Montpellier, France; 2015. Available from: http://www.eurohex.eu/pdf/healthmodule/Allcountries.pdf
EUROSTAT. Overview of the implementation of the GALI question in EU-SILC. 2016. Available from: https://ec.europa.eu/eurostat/cache/metadata/Annexes/hlth_hlye_esms_an2.pdf
EUROSTAT. Methodological Guidelines and Description of EU-SILC Target Variables. Vol. DocSILC065. 2020.
Crowther MJ. Multilevel mixed effects survival analysis: Estimation, simulation and application. 2018;1–17. https://doi.org/10.1177/1536867X19893639
Gran JM, Wasmuth L, Amundsen EJ, Lindqvist BH, Aalen OO. Growth rates in epidemic models: application to a model for HIV/AIDS progression. Stat Med. 2009;28(July 2006):221–39. https://doi.org/10.1002/sim.3219
Thiébaut ACM, Bénichou J. Choice of time-scale in Cox’s model analysis of epidemiologic cohort data: A simulation study. Stat Med. 2004;23(24):3803–20. https://doi.org/10.1002/sim.2098
Eulenburg C, Schroeder J, Obi N, Heinz J, Seibold P, Rudolph A, et al. A Comprehensive Multistate Model Analyzing Associations of Various Risk Factors With the Course of Breast Cancer in a Population-Based Cohort of Breast Cancer Cases. Am J Epidemiol. 2016 Feb 15;183(4):325–34. https://doi.org/10.1093/aje/kwv163
Vatchera K., Lee M, MacCormick JB, Rahbar MH. The Effect of Ignoring Statistical Interactions in Regression Analyses Conducted in Epidemiologic Studies: An Example with Survival Analysis Using Cox Proportional Hazards Regression Model. Epidemiology. 2015;6(1):1–17. https://doi.org/10.4172/2161-1165.1000216
Petersen JH, Andersen PK, Gill RD. Variance components models for survival data. Stat Neerl. 1996;50(1):193–211. https://doi.org/10.1111/j.1467-9574.1996.tb01487.x
Jackson C. Flexsurv: A Platform for Parametric Survival Modeling in R. J Stat Softw. 2016;70(8). https://doi.org/10.18637/jss.v070.i08
EUROSTAT. Healthy life years and life expectancy at age 65 by sex. 2019. Available from: https://ec.europa.eu/eurostat/tgm/table.do?tab=table&plugin=1&language=en&pcode=tepsr_sp320. Accessed 20/05/2019
World Health Organizacion. Life expectancy and Healthy life expectancy. Data by country. Global Health Observatory data repository. 2018 [cited 2020 Dec 18]. Available from: http://apps.who.int/gho/data/node.main.688?lang=en
EHLEis. Healthy Life Years (HLY). European Health & Life Expectancy Information System. [cited 2019 Sep 15]. Available from: http://www.eurohex.eu/IS/web/app.php/Ehleis/Survey/Health?SubTyp=None
Salavecz G, Chandola T, Pikhart H, Dragano N, Siegrist J, Jöckel K, et al. Work stress and health in Western European and post- communist countries: an East — West comparison study. J Epidemiol Community Heal. 2010;64(1):57–62. https://doi.org/10.1136/jech.2008.075978
Meslé F, Vallin J. The End of East—West Divergence in European Life Expectancies? An Introduction to the Special Issue. Eur J Popul. 2017;33(5):615–27. https://doi.org/10.1007/s10680-017-9452-2
Fihel A, Pechholdová M. Between ‘Pioneers’ of the Cardiovascular Revolution and Its ‘Late Followers’: Mortality Changes in the Czech Republic and Poland Since 1968. Eur J Popul. 2017. https://doi.org/10.1007/s10680-017-9456-y
Pechholdová M, Fihel A. Understanding recent mortality reversal in Central Europe: case of Czech Republic and Poland. In: Paper presented at the XXVII IUSSP International Population Conference, Busan, Korea, 26–31 August 2013. Busan, Korea; 2013. p. 1–5.
Moor N, de Graaf PM, Komter A. Family, welfare state generosity and the vulnerability of older adults: A cross-national study. J Aging Stud. 2013;27(4):347–57. https://doi.org/10.1016/j.jaging.2013.07.002
Dykstra PA. Older adult loneliness: Myths and realities. Eur J Ageing. 2009;6(2):91–100. https://doi.org/10.1007/s10433-009-0110-3
Fokkema T, Liefbroer AC. Trends in living arrangements in Europe: Convergence or divergence? Demogr Res. 2008;19:1351–418. https://doi.org/10.4054/DemRes.2008.19.36
Mohd S, Senadjki A, Mansor N. Living Arrangements of Elderly: Evidence from Household Income Expenditure Survey. J Popul Ageing. 2017;10(4):323–42. https://doi.org/10.1007/s12062-016-9165-z
Jürges H. Health insurance coverage and access to care among European elders: Cross- national differences and social gradients. Ageing Eur Policies an Incl Soc. 2015;301–15.
Dykstra PA, Fokkema T. Relationships between parents and their adult children: a West European typology of late-life families. Ageing Soc. 2011;31(May):545–69. https://doi.org/10.1017/S0144686X10001108
Venkatapuram S, Ehni H-J, Saxena A. Equity and healthy ageing. Bull World Health Organ. 2017 Nov 1;95(11):791–2. https://doi.org/10.2471/BLT.16.187609
Funding
Funding: Sarahí Rueda-Salazar received funding from the Spanish Ministry of Economy and Competitiveness. FPI scholarship I+D+I Project “With whom will I live and who will take care of me? Present and future determinants of co-residence and dependence of the old-age population” (Reference Project CSO2014-60113-R). This work was also supported by the Spanish ‘Ramón y Cajal’ programme (JS, RYC-2013-14851) and the R&D projects CSO2017-89721-R (Will future elderly have any relative available to care for them) and PID2020-113934RB-I00 (COMORHEALTHSES) as well as the European Research Council (ERC-2019-CoG-864616, HEALIN project; and the Catalan government under the CERCA programme). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest: The authors have declared that no competing interests exist.
Supplemental material
Rights and permissions
Open Access: This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
About this article
Cite this article
Rueda-Salazar, S., Spijker, J. & Devolder, D. Functional Limitations among European Older Adults: Cross-Country Differences in Health Improvements and Social Environment Influence. J Frailty Aging 11, 378–386 (2022). https://doi.org/10.14283/jfa.2022.55
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jfa.2022.55