Abstract
Background
Sarcopenic obesity (SO) is associated with poorer physical performance in the elderly and will increase in relevance with population ageing and the obesity epidemic. The lack of a consensus definition for SO has resulted in variability in its reported prevalence, poor inter-definitional agreement, and disagreement on its impact on physical performance, impeding further development in the field. While sarcopenia definitions have been compared, the impact of obesity definitions in SO has been less well-studied.
Objectives
To compare 3 widely-adopted definitions of obesity in terms of SO prevalence, inter-definitional agreement, and association with muscle function.
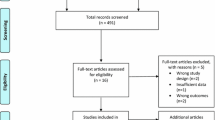
Design
Cross-sectional.
Setting
GERILABS study, Singapore
Participants
200 community-dwelling, functionally-independent older adults.
Measurements
We utilized three commonly-used definitions of obesity: body mass index (BMI), waist circumference (WC) and DXA-derived fat mass percentage (FM%). Sarcopenia was defined using Asian Working Group for Sarcopenia criteria. For muscle function, we assessed handgrip strength, gait speed and Short Physical Performance Battery (SPPB). Subjects were classified into 4 body composition phenotypes (normal, obese, sarcopenic and SO), and outcomes were compared between groups.
Results
The prevalence rate for SO was lowest for BMI (0.5%) compared to FM% (10.0%) and WC (10.5%). Inter-definitional agreement was lowest between BMI and WC (κ=0.364), and at best moderate between FM% and WC (κ=0.583). SO performed the worst amongst body composition phenotypes in handgrip strength, gait speed and SPPB (all p<0.01) only when defined using WC. In regression analyses, SO was associated with decreased SPPB scores (β=−0.261, p=0.001) only for the WC definition.
Conclusion
There is large variation in the prevalence of SO across different obesity definitions, with low-to-moderate agreement between them. Our results corroborate recent evidence that WC, and thus central obesity, is best associated with poorer muscle function in SO. Thus, WC should be further explored in defining obesity for accurate and early characterization of SO among older adults in Asian populations.
Similar content being viewed by others
References
Lim W-S, Canevelli M, Cesari M. Editorial: Dementia, Frailty and Aging. Frontiers in Medicine. 2018;5(168).
Roubenoff R. Sarcopenic obesity: the confluence of two epidemics. Obes Res. 2004;12(6):887–8.
Organisation WH. Global Health and Aging. 2011.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15(2):95–101.
Wannamethee SG, Atkins JL. Muscle loss and obesity: the health implications of sarcopenia and sarcopenic obesity. The Proceedings of the Nutrition Society. 2015;74(4):405–12.
Kemmler W, von Stengel S, Engelke K, Sieber C, Freiberger E. Prevalence of sarcopenic obesity in Germany using established definitions: Baseline data of the FORMOsA study. Osteoporos Int. 2016;27(1):275–81.
Batsis JA, Barre LK, Mackenzie TA, Pratt SI, Lopez-Jimenez F, Bartels SJ. Variation in the prevalence of sarcopenia and sarcopenic obesity in older adults associated with different research definitions: dual-energy X-ray absorptiometry data from the National Health and Nutrition Examination Survey 1999–2004. Journal of the American Geriatrics Society. 2013;61(6):974–80.
Kalinkovich A, Livshits G. Sarcopenic obesity or obese sarcopenia: A cross talk between age-associated adipose tissue and skeletal muscle inflammation as a main mechanism of the pathogenesis. Ageing research reviews. 2017;35:200–21.
Baumgartner RN. Body composition in healthy aging. Annals of the New York Academy of Sciences. 2000;904(1):437–48.
Baumgartner RN, Wayne SJ, Waters DL, Janssen I, Gallagher D, Morley JE. Sarcopenic obesity predicts instrumental activities of daily living disability in the elderly. Obes Res. 2004;12(12):1995–2004.
Batsis JA, Villareal DT. Sarcopenic obesity in older adults: aetiology, epidemiology and treatment strategies. Nature Reviews Endocrinology. 2018;14(9):513–37.
Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. The journals of gerontology Series A, Biological sciences and medical sciences. 2014;69(5):547–58.
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–56.
Akishita M, Kozaki K, Iijima K, Tanaka T, Shibasaki K, Ogawa S, et al. Chapter 1 Definitions and diagnosis of sarcopenia. Geriatr Gerontol Int. 2018;18 Suppl 1:7–12.
Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, et al. American association of clinical endocrinologists and American college of endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocrine practice: official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2016;22 Suppl 3:1–203.
Tay L, Ding YY, Leung BP, Ismail NH, Yeo A, Yew S, et al. Sex-specific differences in risk factors for sarcopenia amongst community-dwelling older adults. Age (Dordrecht, Netherlands). 2015;37(6):121.
Sahadevan S, Lim PP, Tan NJ, Chan SP. Diagnostic performance of two mental status tests in the older chinese: influence of education and age on cut-off values. International journal of geriatric psychiatry. 2000;15(3):234–41.
Lee YS, Biddle S, Chan MF, Cheng A, Cheong M, Chong YS, et al. Health Promotion Board-Ministry of Health Clinical Practice Guidelines: Obesity. Singapore Medical Journal. 2016;57(6):292–300.
Who EC. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet (London, England). 2004;363(9403):157.
Odegaard AO, Pereira MA, Koh WP, Gross MD, Duval S, Yu MC, et al. BMI, all-cause and cause-specific mortality in Chinese Singaporean men and women: the Singapore Chinese health study. PloS one. 2010;5(11):e14000.
Organization WH. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia; 2000.
Alberti KG, Zimmet P, Shaw J. Metabolic syndrome—a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabetic medicine: a journal of the British Diabetic Association. 2006;23(5):469–80.
Scott D, Daly RM, Sanders KM, Ebeling PR. Fall and fracture risk in sarcopenia and dynapenia with and without obesity: the role of lifestyle interventions. Current osteoporosis reports. 2015;13(4):235–44.
Dufour AB, Hannan MT, Murabito JM, Kiel DP, McLean RR. Sarcopenia definitions considering body size and fat mass are associated with mobility limitations: the Framingham Study. The journals of gerontology Series A, Biological sciences and medical sciences. 2013;68(2):168–74.
Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc. 2013;14(8):531–2.
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–8.
Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clinical Gerontologist: The Journal of Aging and Mental Health. 1986;5(1–2):165–73.
Guigoz Y. The Mini Nutritional Assessment (MNA) review of the literature—What does it tell us? J Nutr Health Aging. 2006;10(6):466–85; discussion 85-7.
Guerra RS, Amaral TF, Marques EA, Mota J, Restivo MT. Anatomical location for waist circumference measurement in older adults: a preliminary study. Nutricion hospitalaria. 2012;27(5):1554–61.
Puthoff ML. Outcome measures in cardiopulmonary physical therapy: short physical performance battery. Cardiopulmonary physical therapy journal. 2008;19(1):17.
Yeo A, Chong M, Tay L, Yew SP, Tan C, Ismail N, et al. TRENDS AND PREDICTORS OF 2-YEAR ACTIVITY PARTICIPATION IN COMMUNITY DWELLING OLDER ADULTS. Innovation in Aging. 2017;1(suppl_1):905–6.
Kemmler W, Teschler M, Weisenfels A, Sieber C, Freiberger E, von Stengel S. Prevalence of sarcopenia and sarcopenic obesity in older German men using recognized definitions: high accordance but low overlap! Osteoporos Int. 2017;28(6):1881–91.
de Carvalho DHT, Scholes S, Santos JLF, de Oliveira C, Alexandre TdS. Does abdominal obesity accelerate muscle strength decline in older adults? Evidence from the English Longitudinal Study of Ageing. The Journals of Gerontology: Series A. 2018:gly178-gly.
Lim JP, Leung BP, Ding YY, Tay L, Ismail NH, Yeo A, et al. Monocyte chemoattractant protein-1: a proinflammatory cytokine elevated in sarcopenic obesity. Clinical Interventions in Aging. 2015;10:605–9.
McHugh ML. Interrater reliability: the kappa statistic. Biochemia Medica. 2012;22(3):276–82.
Acknowledgments
This study was supported by Lee Foundation grant 2013. We extend our appreciation to the Senior Activity Centers and the study participants who have graciously consented to participate in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure: The authors report no conflicts of interest in this work.
Electronic supplementary material
Supplementary Table 1
: Additional comparisons of demographics, comorbidities and geriatric syndromes among body composition phenotypes for different definitions of obesity
Rights and permissions
About this article
Cite this article
Khor, E.QE., Lim, J.P., Tay, L. et al. Obesity Definitions in Sarcopenic Obesity: Differences in Prevalence, Agreement and Association with Muscle Function. J Frailty Aging 9, 37–43 (2020). https://doi.org/10.14283/jfa.2019.28
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jfa.2019.28