Abstract
Background
The PRECINCT (Pattern of peritoneal dissemination and REsponse to systemic Chemotherapy IN Common and uncommon peritoneal Tumors) is a prospective, multicenter, observational study. This report from phase I of PRECINCT outlines variations in recording the surgical peritoneal cancer index (sPCI) at experienced peritoneal malignancy centers and the incidence of pathologically confirmed disease in morphologically different peritoneal lesions (PL).
Methods
The sPCI was recorded in a prespecified format that included the morphological appearance of PL. Six prespecified morphological terms were provided. The surgical and pathological findings were compared.
Results
From September 2020 to December 2021, 707 patients were enrolled at 10 centers. The morphological details are routinely recorded at two centers, structure bearing the largest nodule, and exact size of the largest tumor deposit in each region at four centers each. The most common morphological terms used were normal peritoneum in 3091 (45.3%), tumor nodules in 2607 (38.2%) and confluent disease in 786 (11.5%) regions. The incidence of pathologically confirmed disease was significantly higher in ‘tumor nodules’ with a lesion score of 2/3 compared with a lesion score of 1 (63.1% vs. 31.5%; p < 0.001). In patients receiving neoadjuvant chemotherapy, the incidence of pathologically confirmed disease did not differ significantly from those undergoing upfront surgery [751 (47.7%) and 532 (51.4%) respectively; p = 0.069].
Conclusions
The sPCI was recorded with heterogeneity at different centers. The incidence of pathologically confirmed disease was 49.2% in ‘tumor nodules’. Frozen section could be used more liberally for these lesions to aid clinical decisions. A large-scale study involving pictorial depiction of different morphological appearances and correlation with pathological findings is indicated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
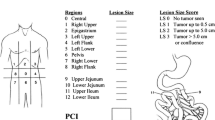
Three decades ago, Paul Sugarbaker devised the peritoneal cancer index (PCI) for quantifying the extent of peritoneal disease.1 The PCI has since proven to be a robust prognostic indicator for predicting the benefit of cytoreductive surgery (CRS) and is an important tool for therapeutic decision making.2 The PCI level is one of the factors considered while selecting patients for CRS for some primary tumors such as colorectal cancer, peritoneal mesothelioma (PeM), and gastric cancer, and by some surgeons for epithelial ovarian cancer (EOC); it is one of the variables used in predictive scores and nomograms, and a stratification factor in randomized trials.3,4,5,6,7,8,9
The PCI is essentially the surgical PCI (sPCI). Although it is recorded as a numerical value, there is more to it than just the absolute value. The sum of the lesion score (LS) in specific regions (e.g. the small bowel PCI) and the number of regions contributing to the sPCI, all have prognostic implications.10,11 Subsequently, the radiological PCI (rPCI) and pathological PCI (pPCI) were devised to document the disease extent on imaging and pathological evaluation, respectively.12,13,14
Although the sPCI is an objective variable, the evaluation of the disease extent by the surgeon is in itself a subjective evaluation. It has been shown that the sPCI differs from the pPCI in over 70% of patients.14,15 Surgeons tend to overestimate the disease extent more often than underestimating the extent. The accuracy also depends on the primary tumor site.14 In the era of precision medicine where multiple therapeutic modalities are available, a surgical intervention that provides no oncological benefit and carries a risk of morbidity should be avoided as far as possible, and a patient who could benefit from a procedure should not be denied the procedure. In this context, the importance of accurate prediction of the sPCI cannot be underestimated. A false positive assessment of the presence of disease could also lead to unnecessary resection of vital structures.
Arguably, of all oncological surgical procedures, CRS is the only procedure that is very heavily dependent on the surgeon’s visual inspection of the disease extent. Consequently, attention needs to be given to the morphological appearance of peritoneal lesions (PLs). To date, the morphological appearance of PLs remains a topic that has been poorly researched. There are a few studies that have looked at the incidence of microscopic disease in areas of post-chemotherapy scarring, and other studies that have described lesions as ‘suspicious’, ‘overtly malignant’, or ‘non-malignant’.16,17 We carried out a prospective observational study called PRECINCT (Pattern of peritoneal dissemination and REsponse to systemic Chemotherapy IN Common and uncommon peritoneal Tumors) that involved a detailed recording of the sPCI, including the morphological appearance of PLs.18 This report from phase I of the PRECINT study looks at the variations in recording the sPCI at experienced peritoneal malignancy centers in different regions of the world and compares the pathological presence of disease in morphologically different PLs, as recorded by the surgeon.
Methods
This was a prospective, multicenter, observational study. The detailed protocol of the study has been previously published.18 There was no therapeutic intervention in the study. The study comprised recording the demographic, clinical, radiological, surgical, and pathological details according to a prespecified format that included details of the distribution of disease, morphological appearance of peritoneal metastases (PM), regional node involvement, and pathological response to systemic chemotherapy (SC). All patients with biopsy-proven PM, from colorectal, appendiceal, gastric, or ovarian cancer, or PeM undergoing CRS with or without intraperitoneal chemotherapy were included. Written informed consent was obtained from all patients.
Format of Data Collection
There are currently no reporting guidelines for both imaging and pathological evaluation of CRS specimens.19 The reporting format in this study included calculation of the rPCI and capturing other details such as the sites and structures bearing the largest tumor nodules and a description of the morphology in each region. Similarly, the surgical findings were to be documented in a systematic, prespecified manner. To ensure uniformity in the morphological description, a list of morphological features was made for the radiological, surgical, and pathological evaluations. This list was made in consultation with all the potential contributors and included radiologists and pathologists in addition to the surgeons. The PROMISE internet application was used as reference.19 The morphological description had to be provided with the LS for each region of the PCI. The first 6 months of the study comprised a test phase in which teams would assess the feasibility and compliance of this form of data capturing. This is a report from phase I. Phase II of the study is currently underway. During the second phase, there is an addition to the protocol for pathological evaluation in which pathologists will be required to take additional sections from the ‘normal appearing’ peritoneum adjacent to tumor nodules.
Inclusion and exclusion criteria
-
Only patients with biopsy-proven PM would be included (pathological evaluation was not mandatory prior to CRS if imaging or exploration confirmed the presence of disease).
-
Patients undergoing second-look procedures with no evidence of PM were excluded.
-
Patients undergoing debulking procedures were included.
-
Patients undergoing palliative procedures that did not involve tumor debulking were excluded.
-
For ovarian cancer, only patients with International Federation of Obstetrics and Gynecology (FIGO) stage III-C or IV-A were included. Patients undergoing surgery at first diagnosis, after neoadjuvant chemotherapy (NACT), and those undergoing surgery for recurrent disease were included. Patients without peritoneal disease were excluded.18
Study endpoints
The primary endpoint is disease distribution in the peritoneal cavity, and the secondary endpoints are pathological response to SC, regional lymph node involvement, morphology of PM, overall survival (OS), and progression-free survival (PFS).18
Sample Size
The number of patients required was determined based on our preliminary study looking at the disease distribution in relation to the disease extent. We considered involvement of different regions in relation to the sPCI as well as different structures in relation to the sPCI for each primary tumor. In addition, consideration was given to another endpoint, that is, pathological response to SC. This was only relevant for colorectal cancer and ovarian cancer. Details of the sample size calculation are provided in the published protocol: the target is 500 patients with colorectal cancer (350 post-NACT), 600 for ovarian cancer (350 undergoing interval CRS), 300 for appendiceal tumors and pseudomyxoma peritonei (PMP), and 100 each for gastric cancer and PeM.18
Eithics
This study was approved by the Zydus Hospital (institution of the first author) Ethics Committee on 27 July 2020 (a specific study number was not provided by the committee). At Lyon-Sud Hospital, this study is being carried out within the framework of the RENAPE observational registry (CNIL-no. DR-2010-297) and the BIG-RENAPE registry (NCT02823860), Institutional Review Board (IRB) number A15-128.20 Subsequently, approval was obtained at other centers according to the existing institutional policies.
Statistical Methods (for the Current Study Only)
Categorical data are described as number (%) and non-normally distributed continuous data are expressed as median (range). Categorical data were compared using the Chi-square test. For comparison of parametric and non-parametric data, the Student’s t-test and Mann–Whitney U test were used, respectively.
The list of terms for reporting the morphology of PM intraoperatively included ‘normal peritoneum’, ‘nodule’, ‘confluent nodules’, ‘plaque’, ‘thickening’, ‘scarring’, and ‘adhesion’. The use of other terms was permitted.
Lesions most likely to be malignant, such as ‘tumor nodules’, ‘confluent disease’, ‘mucinous deposits’, ‘omental cake’, and ‘plaques’, were termed ‘morphologically malignant lesions’, while others that could be considered suspicious of harboring disease, such as ‘thickening’, ‘scarring’, and ‘adhesions’, were termed ‘morphologically suspicious lesions’.
The incidence of disease on pathology for each morphological appearance was determined for each of the 13 peritoneal regions for every patient.
A similar comparison was made between ‘morphologically malignant’ and ‘morphologically suspicious’ lesions.
Based on the LS in regions with the morphological appearance of ‘tumor nodules’, these regions were divided into two groups—those with an LS score of 1 and those with an LS score of 2 or 3. The proportion of patients with disease confirmed on pathology in each group was compared.
Results
From 15 September 2020 to 31 December 2021, 707 patients were recruited at 10 centers.
Contributing Centers
Sixteen centers were considered for the study—2 index centers (of the first and last author) and 14 other centers. Three centers declined and three other centers volunteered to participate after publication of the protocol. Eventually, only 11/19 centers contributed to the study (two centers had problems with pathological evaluation and six centers could not complete other additional requirements for the study). Phase I had to be extended to 18 months to accommodate all the centers that wanted to contribute and to allow time for some centers to get ethical approval and other permissions in place. Data from one center is not included in this analysis due to missing data for all three PCIs.
The distribution of patients according to the center and primary tumor site is provided in electronic supplementary material (ESM) S1.
Primary Tumor Site
The most common primary tumor site was ovarian cancer (n = 263), followed by appendiceal tumors and PMP (n = 181) and colorectal cancer (n = 153). NACT was used in 33 (86.8%) patients with gastric cancer, 107 (70.3%) patients with colorectal cancer, 171 (65.0%) patients with ovarian cancer, 19 (54.2%) patients with rare tumors, 8 (24.2%) patients with PeM, and 35 (19.1%) patients with appendiceal tumors and PMP. Secondary CRS was performed in 72 (10.1%) patients [57 (21.6%) ovarian cancer; 8 (4.3%) PMP; 3 (1.9%) colorectal cancer; 3 (8.5%) rare tumors, and 1 (3.0%) PeM]. Although it was not planned to include the uncommon primary sites or rare tumors, they were included since all the centers provided data for these tumors (ESM S2) .
Surgical Peritoneal Cancer Index and its Additional Details
The sPCI is routinely reported at all 10 centers and was available for 683/707 (96.6%) patients. The median sPCI was 12 (range 0–39) [6 for gastric cancer (range 0–6); 7 for colorectal cancer (range 0–39); 12 for ovarian cancer (range 0–39); 16 for appendiceal tumors and PMP (range 0–39); 11 for rare tumors (range 0–30), and 13 for PeM (range 0–39)]. A completeness of cytoreduction (CC-0/1) resection was achieved in 683 (96.6%) patients.
In addition to the total value of sPCI, the description of morphological appearance, the structure bearing the largest tumor nodule, the size of the largest tumor nodule, and the LS for each region had to be captured. Of these four requirements, the LS was recorded at all centers and morphological details were routinely recorded at two centers, but all centers provided this detail for the study. The structure bearing the largest tumor nodule in each region was recorded at four centers and was available for the current study for only 50 patients. The exact size of the largest tumor deposit in each region was captured for selected patients at four centers.
Peritoneal Regions Evaluated
A synopsis of the main outcomes of this analysis is presented in Fig. 1. Both morphological appearance and pPCI were provided for 603 (86.4%) patients. Overall, 7839 regions were evaluable in 603 patients, of whom the morphological description was available for 6816 (86.9%) regions (Fig. 1). This discrepancy was due to missing details in some patients.
Morphological Terms Used
In addition to the seven prespecified terms, six other terms were used (Table 1), amounting to a total of 13 terms. The most common morphological term used was normal peritoneum in 3091(45.3%) patients, followed by tumor nodules in 2607 (38.2%) patients, and then confluent disease in 786 (11.5%) patients. Prespecified terms were used in 6711 (98.5%) patients and unspecified terms were used in 105 (1.5%) patients.
The use of different morphological terms according to the primary tumor site is presented in Table 2. The 13-region distribution of morphological terms for each primary tumor is provided in ESM S3–S8.
Classification of Morphological Appearances
In total, 3587 (52.6%) lesions were classified as morphologically malignant and 73 (1%) lesions were classified as morphologically suspicious (Fig. 1). The use of both types of terms varied significantly according to the primary tumor type (Table 3). Both types of terms were used less for colorectal cancer, gastric cancer, and rare diseases, implying that the disease extent could be responsible for this difference. Among the morphologically malignant lesions, the incidence of disease on pathology was the highest for omental cake (100%), followed by mucinous lesions (83.3%), confluent disease (82.6%), and plaques (71.0%). Conversely, it was only 49.2% for tumor nodules. Of the morphologically suspicious lesions, presence of disease on pathology was highest in lesions labeled as ‘thickening’ (82.7%) and <40% for both scarring and adhesions. However, the incidence of disease in lesions termed ‘scarring’ was 33% and this term was most commonly used for ovarian cancer (Fig. 2). Overall, the incidence of disease on pathology was not significantly different among the morphologically malignant and morphologically suspicious lesions (58.3% vs. 50%; p = 0.260).
Pathologically Confirmed Disease in ‘Tumor Nodules’
Overall, 1152 (44.1%) regions were given an LS of 1, and 1358 (52.0%) were given an LS of 2 or 3. The incidence of disease on pathology was significantly higher in regions with an LS score of 2/3 compared with an LS score of 1 (63.1% vs. 31.5%; p < 0.001). The 13-region distribution is provided in Table 4.
We also studied the impact of NACT. Of the 2607 lesions classified as ‘tumor nodules’, 1572 (60.2%) were in patients who received NACT and 1035 (39.8%) were in patients who did not receive NACT. In patients receiving NACT, 751 (47.7%) lesions showed disease at pathological evaluation that did not differ significantly from those undergoing upfront surgery [532 (51.4%); p = 0.069] (Table 4).
Normal Peritoneum and Incidence of Occult Disease
The term normal peritoneum was used for 3091 (45.3%) regions. The 13-region distribution is provided in ESM S9. Disease on pathology was observed in 335 (10.8%) regions. We did not distinguish between regions that were resected or not resected as this represents the normal course of clinical practice; this is elaborated in the Discussion section. The incidence of occult disease was highest in region 12 (24.5%) and lowest in region 11 (3.0%). The 13-region distribution of occult disease is presented in ESM S10.
Discussion
This study illustrates the heterogeneity in recording the sPCI at experienced peritoneal malignancy centers around the world and highlights the need to further define and standardize the recording of this important prognostic indicator. Six centers could not contribute as they could not provide a detailed sPCI. The most significant finding was that only 50% of the lesions classified as ‘tumor nodules’ showed disease at pathological evaluation. The discrepancy was higher for smaller lesions (LS 1) (Table 4). This calls for more liberal use of frozen section to confirm the presence of disease in small tumor nodules. There was no difference in the incidence of pathologically confirmed disease in tumor nodules among patients who received NACT and those who did not. It might be expected that the accuracy of visual inspection would be higher when surgery is performed upfront, however this was not the case with ‘tumor nodules’. During upfront surgery, there could be confusion with benign lesions or inflammatory changes. Although unspecified terms were used in a small percentage of patients, these could be the lesions that require extra caution when deciding whether to resect the given area or not. In addition, 82.7% of the lesions classified as ‘thickening’ had disease at pathology.
The interobserver variation in recording the PCI has never been studied systematically.21 A large-scale study that involves pictorial depiction of different PLs and correlation with the presence of disease on pathology is needed to improve the accuracy of the sPCI in predicting the true extent of disease and in comparing outcomes from different centers. Examples of different morphological appearances is provided in Fig. 3.
Different morphological appearances of peritoneal lesions. (a) Tumor nodule in ovarian cancer, pathologically positive. (b) Tumor nodules in PMP, pathologically negative. (c) Tumor nodules in ovarian cancer, pathologically positive. (d) Confluent disease in high-grade PMP, pathological positive. (e) Plaques and confluent disease in gastric cancer, pathologically positive. (f) Scarring in ovarian cancer, pathologically positive. (g) Adhesions in high-grade PMP, pathologically positive. (h) Thickening in ovarian cancer, pathologically positive. (i) Mucinous lesions in low-grade PMP, pathologically positive. (j) Adhesions in ovarian cancer, pathologically negative. (k) Nodules and thickening in sigmoid colon cancer, pathologically positive. PMP pseudomyxoma peritonei
Tumor Nodules Could be Classified as ‘Morphologically Suspicious’
While only 50% of tumor nodules had disease at pathological assessment, in all other morphologically malignant lesions the incidence was more than 70%. To the best of our knowledge, this is the first study in which the morphology of PL was reported using a prespecified set of terms. In the study by Costantini et al., visual appearance of diaphragmatic disease was classified as visually pathologic or visually dubious.17 Over 80% of patients with visually dubious lesions had disease on pathology, while 100% of the visually pathologic lesions had disease on pathology. From the images presented in the manuscript, many surgeons could have classified the visually dubious lesions as pathologic.
While designing this study, we had no supportive studies for a baseline reference. Therefore, we could not predict what proportion of patients with ‘tumor nodules’ might have pathologically confirmed disease. A recently published manuscript evaluating the role of artificial intelligence in correctly distinguishing malignant from non-malignant lesions reported a similar incidence of disease at pathology (50%) when the evaluation was performed by surgeons.22
Potential Role of Fluorescence-Guided Surgery
Another alternative method of classifying PL accurately is the use of fluorescence-guided surgery (FGS). Currently, large-scale validation studies on the role of FGS are lacking, as is standardization regarding the dye to be used, the timing of injection, and the imager to be used.23,24 The main advantage seems to be the high negative predictive value of 90–100%.23 Some of the dyes that are used, such as indocyanine green, detect lesions based on the vascularity, which may not be ideal for detecting malignant PLs, while others such as 5-aminolevulinic acid (ALA) are expensive and not widely available.25,26 Other targeted probes are being developed based on the molecular profiles of tumors.27 The performance of these in relation to tumor heterogeneity, timing of PM, the sites that are biopsied, and timing of surgery and the non-flourescent sites that are biopsied will need to be considered.28
‘Normal Appearing’ Peritoneum
While estimating the sPCI, even regions that are not involved or resected are evaluated, which is why the most common morphologic term used was ‘normal peritoneum’. The incidence of occult disease in lesions termed ‘normal peritoneum’ was 10%, which is in line with previously published reports.19 We did not make a distinction between regions that were or were not resected as this captures the clinical scenario at CRS and the incidence of occult disease could be higher. Some structures such as the greater omentum are removed in the majority of patients and the lesser omentum is removed in selected patients, even if not directly involved by disease, which explains why normal peritoneal regions were resected in this study.
Variation of Morphological Terms According to the Primary Tumor Type
There was a significant difference in the morphological terms used for different diseases—normal peritoneum was reported in nearly 70% of the regions in patients with gastric cancer (median sPCI-6), but was reported for only 33% of patients with appendiceal tumors and PMP (median sPCI-16) (Table 2). Apart from the extent of disease itself, the reason for the variation could be that different primary tumors produce morphologically different lesions, for example, mucinous lesions in PMP, scarring in ovarian cancer after NACT, plaques in mesothelioma and signet ring cell tumors, and this will be studied in greater detail when the study completes recruitment. The mechanisms of peritoneal spread could have an impact on the morphologic appearance.29,30 Trans-lymphatic spread and hematogenous spread are likely to produce more diffuse involvement and miliary disease compared with transcoelomic spread, however this is an unproven assumption.
Future Directive
The main takeaway from this study is that caution should be exercised when resecting regions that the surgeon classifies as ‘tumor nodules’. Frozen section could be used more liberally in these cases before performing potentially morbid procedures such as visceral resections or diaphragmatic stripping more so in older and frail patients. The same should be applied to ‘morphologically suspicious lesions’ such as ‘adhesions’ and ‘scarring’. Using pictorial depiction of various lesions to obtain a consensus among surgeons regarding the most appropriate morphological term for each one, it may be possible in future to limit the number of terms used. It could also help less experienced surgeons in intraoperative decision making.
Strengths and Limitations
The biggest limitation of this study is the missing data. This was something that we had anticipated while designing the study. The study received no external funding and it was not possible to employ additional personnel for data collection, with the existing staff already working at full capacity. No additional training was organized for data collection as most of the information specific to this study was related to the three PCIs and required additional work from the surgeons, radiologists and pathologists. This was quite time-consuming for the radiologists and pathologists, which explains the 10–25% of missing data for many variables. The strengths of this study are its prospective nature and the involvement of high-volume centers from around the world, some of which have been pioneers in this field.
Conclusions
The sPCI was recorded with a lot of heterogeneity in the details captured at experienced peritoneal malignancy centers. The incidence of pathologically confirmed disease was only 49.2% in lesions labeled as ‘tumor nodules’. A large-scale study that involves pictorial depiction of different morphological appearances of PLs and correlation with the presence of disease at pathological evaluation is needed to improve the accuracy of the sPCI in predicting the true extent of disease. Frozen section should be used more liberally in lesions classified as ‘tumor nodules’, and morphologically suspicious lesions such as ‘scarring’ and ‘adhesions’, to guide intraoperative decisions.
References
Jacquet P, Sugarbaker PH. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat Res. 1996;82:359–74. https://doi.org/10.1007/978-1-4613-1247-5_23.
Foster JM, Zhang C, Rehman S, Sharma P, Alexander HR. The contemporary management of peritoneal metastasis: a journey from the cold past of treatment futility to a warm present and a bright future. CA Cancer J Clin. 2023;73:49–71. https://doi.org/10.3322/caac.21749.
Faron M, Macovei R, Goéré D, Honoré C, Benhaim L, Elias D. Linear Relationship of Peritoneal Cancer Index and Survival in Patients with Peritoneal Metastases from Colorectal Cancer. Ann Surg Oncol. 2016;23(1):114–9. https://doi.org/10.1245/s10434-015-4627-8.
Kusamura S, Torres Mesa PA, Cabras A, Baratti D, Deraco M. The Role of Ki-67 and Pre-cytoreduction Parameters in Selecting Diffuse Malignant Peritoneal Mesothelioma (DMPM) Patients for Cytoreductive Surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC). Ann Surg Oncol. 2016;23(5):1468–73. https://doi.org/10.1245/s10434-015-4962-9.
Chia CS, You B, Decullier E, Vaudoyer D, Lorimier G, Abboud K, Bereder JM, Arvieux C, Boschetti G, Glehen O; BIG RENAPE Group. Patients with Peritoneal Carcinomatosis from Gastric Cancer Treated with Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy: Is Cure a Possibility? Ann Surg Oncol. 2016 Jun;23(6):1971-9. https://doi.org/10.1245/s10434-015-5081-3.
Jónsdóttir B, Lomnytska M, Poromaa IS, et al. The Peritoneal Cancer Index is a Strong Predictor of Incomplete Cytoreductive Surgery in Ovarian Cancer. Ann Surg Oncol. 2021;28:244–51. https://doi.org/10.1245/s10434-020-08649-6.
Demey K, Wolthuis A, de Buck van Overstraeten A, Fieuws S, Vandecaveye V, Van Cutsem E, D'Hoore A. External Validation of the Prognostic Nomogram (COMPASS) for Patients with Peritoneal Carcinomatosis of Colorectal Cancer. Ann Surg Oncol. 2017 Nov;24(12):3604-3608. https://doi.org/10.1245/s10434-017-6042-9.
Enblad M, Ghanipour L, Cashin PH. Prognostic scores for colorectal cancer with peritoneal metastases treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Int J Hyperthermia. 2018;34(8):1390–5. https://doi.org/10.1080/02656736.2018.1464668.
Quénet F, Elias D, Roca L, Goéré D, Ghouti L, Pocard M, Facy O, et al. Cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy versus cytoreductive surgery alone for colorectal peritoneal metastases (PRODIGE 7): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22(2):256–66. https://doi.org/10.1016/S1470-2045(20)30599-4.
Yonemura Y, Prabhu A, Sako S, Ishibashi H, Mizumoto A, Takao N, Ichinose M, Motoi S, Liu Y, Nishihara K, et al. Long Term Survival after Cytoreductive Surgery Combined with Perioperative Chemotherapy in Gastric Cancer Patients with Peritoneal Metastasis. Cancers. 2020;12(1):116. https://doi.org/10.3390/cancers12010116.
Bhatt A, Kammar P, Mehta S, Damodaran D, Zaveri S, Patel MD, Sinukumar S, et al. Chasing Rainbows? the Possibility of “Cure” in Patients with Colorectal Peritoneal Metastases Undergoing Cytoreductive Surgery and HIPEC: a Retrospective Study by INDEPSO. Indian J Surg Oncol. 2019;10(Suppl 1):49–56. https://doi.org/10.1007/s13193-019-00879-9.
Salo SAS, Lantto E, Robinson E, Myllärniemi M, Laaksonen S, Salo JA, Rantanen T, Ilonen I. Prognostic role of radiological peritoneal cancer index in malignant peritoneal mesothelioma: national cohort study. Sci Rep. 2020;10(1):13257. https://doi.org/10.1038/s41598-020-70044-8.
Avesani G, Arshad M, Lu H, Fotopoulou C, Cannone F, Melotti R, Aboagye E, Rockall A. Radiological assessment of Peritoneal Cancer Index on preoperative CT in ovarian cancer is related to surgical outcome and survival. Radiol Med. 2020;125(8):770–6. https://doi.org/10.1007/s11547-020-01170-6.
Bhatt A, Yonemura Y, Mehta S, Benzerdjeb N, Kammar P, Parikh L, et al. The Pathologic Peritoneal Cancer Index (PCI) Strongly Differs From the Surgical PCI in Peritoneal Metastases Arising From Various Primary Tumors. Ann Surg Oncol. 2020;27(8):2985–96. https://doi.org/10.1245/s10434-020-08234-x.
de Boer NL, Brandt-Kerkhof ARM, Madsen EVE, Doukas M, Verhoef C, Burger JWA. The Accuracy of the Surgical Peritoneal Cancer Index in Patients with Peritoneal Metastases of Colorectal Cancer. Dig Surg. 2021;38(3):205–11. https://doi.org/10.1159/000513353.
Hynninen J, Lavonius M, Oksa S, Grénman S, Carpén O, Auranen A. Is perioperative visual estimation of intra-abdominal tumor spread reliable in ovarian cancer surgery after neoadjuvant chemotherapy? Gynecol Oncol. 2013;128(2):229–32. https://doi.org/10.1016/j.ygyno.2012.11.007.
Costantini B, Rosati A, Vargiu V, Gallitelli V, Di Ilio C, Moroni R, et al. Visual Peritoneal Evaluation of Residual Disease After Neoadjuvant Chemotherapy in Advanced Ovarian Cancer Patients: The VIPER Study. Ann Surg Oncol. 2023;30(4):2319–28. https://doi.org/10.1245/s10434-022-12861-x.
Bhatt A, Rousset P, Baratti D, et al. Patterns of peritoneal dissemination and response to systemic chemotherapy in common and rare peritoneal tumours treated by cytoreductive surgery: study protocol of a prospective, multicentre, observational study BMJ Open 2021;11:e046819. https://doi.org/10.1136/bmjopen-2020-046819
Bhatt A, Yonemura Y, Benzerdjeb N, Mehta S, Mishra S, Parikh L, et al. Pathological assessment of cytoreductive surgery specimens and its unexplored prognostic potential-a prospective multi-centric study. Eur J Surg Oncol. 2019;45(12):2398–404. https://doi.org/10.1016/j.ejso.2019.07.019.
Villeneuve L, Thivolet A, Bakrin N, et al. A new Internet tool to report peritoneal malignancy extent. peritoneal malignancy stage evaluation (promise) application. Eur J Surg Oncol 2016;42:877–82. https://doi.org/10.1016/j.ejso.2016.03.015
Villeneuve L, Passot G, Glehen O, et al. The RENAPE observational registry: rationale and framework of the rare peritoneal tumors French patient registry. Orphanet J Rare Dis. 2017;12:37. https://doi.org/10.1186/s13023-017-0571-y.
Bhatt A, Rousset P, Benzerdjeb N, et al. Prospective correlation of the radiological, surgical and pathological findings in patients undergoing cytoreductive surgery for colorectal peritoneal metastases: implications for the preoperative estimation of the peritoneal cancer index. Colorectal Dis. 2020;22:2123–32. https://doi.org/10.1111/codi.15368.
Schnelldorfer T, Castro J, Goldar-Najafi A, Liu L. Development of a Deep Learning System for Intra-Operative Identification of Cancer Metastases. Ann Surg. Epub 5 Apr 2024. https://doi.org/10.1097/SLA.0000000000006294.
Boussedra S, Benoit L, Koual M, Bentivegna E, Nguyen-Xuan HT, Bats AS, et al. Fluorescence guided surgery to improve peritoneal cytoreduction in epithelial ovarian cancer: A systematic review of available data. Eur J Surg Oncol. 2022;48(6):1217–23. https://doi.org/10.1016/j.ejso.2022.02.022.
El-Swaify ST, Laban M, Ali SH, et al. Can fluorescence-guided surgery improve optimal surgical treatment for ovarian cancer? A systematic scoping review of clinical studies. Int J Gynecol Cancer. 2023;33:549–61.
Paumgartner G, Probst P, Kraines R, Leevy CM. Kinetics of indocyanine green removal from the blood. Ann N Y Acad Sci. 1970170:134–147
Yonemura Y, Canbay E, Ishibashi H, Nishino E, Endou Y, Sako S, et al. 5-Aminolevulinic Acid Fluorescence in Detection of Peritoneal Metastases. Asian Pac J Cancer Prev. 2016;17(4):2271–5. https://doi.org/10.7314/apjcp.2016.17.4.2271.
Hentzen JEKR, de Jongh SJ, Hemmer PHJ, van der Plas WY, van Dam GM, Kruijff S. Molecular fluorescence-guided surgery of peritoneal carcinomatosis of colorectal origin: a narrative review. J Surg Oncol. 2018;118(2):332–43. https://doi.org/10.1002/jso.25106.
Yonemura Y, Kawamura T, Bandou E, et al. The natural history of free cancer cells in the peritoneal cavity. In: S Gonzalez-Moreno, editor., et al., Advances in peritoneal surface oncology. Berlin: Springer-Verlag, Berlin Heidelberg; 2007. p. 11–23.
Deraco M, Kusamura S, Corbellini C, Guaglio M, Paviglianiti C, Baratti D. Treatment principles for peritoneal surface malignancies. Minerva Chir. 2016;71(2):124–45.
Funding
Open access funding provided by Hospices Civils de Lyon.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Olivier Glehen is a consultant for Gamida Tech. Aditi Bhatt, Laurent Villeneuve, Armando Sardi, Amine Souadka, Alison Buseck, Brendan J. Moran, Basma El Khannousi, Carlos Gonzalez de Pedro, Dario Baratti, Danielle Biacchi, David Morris, Daniel Labow, Edward A. Levine, Faheez Mohamed, Gbadebo Adeleke, Gaurav Goswami, Isabelle Bonnefoy, Katherine Cummins Perry, Konstantinos I. Votanopoulos, Loma Parikh, Marcello Deraco, Mohammad Alyami, Noah Cohen, Nazim Benzerdjeb, Nehal Shah, Nezha El Bahaoui, Nazanin Khajoueinejad, Pascal Rousset, Perry Shen, Shoma Barat, Sophia Stanford, Selma Khouchoua, Samantha Troob, Sakina Shaikh, Umut Sarpel, Vadim Gushchin, Vasanth Mark Samuel, Vahan Kepenekian, and Paolo Sammartino have no disclosures to declare and report no conflicts of interest that may be relevant to the contents of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bhatt, A., Villeneuve, L., Sardi, A. et al. Correlation of Morphological Appearance of Peritoneal Lesions at Laparotomy and Disease at Pathological Assessment in Patients Undergoing Cytoreductive Surgery for Peritoneal Malignancy: Results of Phase I of the PRECINCT Study in 707 Patients. Ann Surg Oncol (2024). https://doi.org/10.1245/s10434-024-16035-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1245/s10434-024-16035-9