Abstract
Background
The purpose of this study was to review and summarize the association between preoperative magnetic resonance imaging (MRI) and surgical outcomes in women with newly diagnosed invasive breast cancer from published randomized controlled trials (RCT).
Materials and Methods
Two independent researchers conducted a systematic review through a comprehensive search of electronic databases, including PubMed, Medline, Embase, Ovid, Cochrane Library, and Web of Science. If there was disagreement between the two reviewers, a third reviewer assessed the manuscript to determine whether it should be included for data extraction. The quality of the papers was assessed using the risk of bias tool, and the evidence was analyzed using GRADE. Meta-analyses using a fixed-effects model were used to estimate the pooled risk ratio (RR) and 95% confidence interval (CI).
Results
Initially, 21 studies were identified, 15 of which were observational comparative studies. A total of five RCTs were included, and they suggested that preoperative MRI significantly reduced the rate of immediate breast-conserving surgery and increased the risk for mastectomy.
Conclusions
From the RCT perspective, preoperative MRI for newly diagnosed invasive breast cancer did not improve surgical outcomes and may increase the risk of mastectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
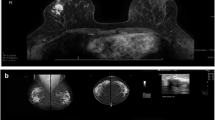
Breast-conserving surgery (BCS) is the standard treatment for early stage breast cancer (BC),1,2 and no ink on the tumor is considered as clear margins3 for invasive BC. Therefore, preoperative evaluation is essential once multifocality and multicentricity are well-known characteristics of BC.4 Magnetic resonance imaging (MRI) is not only a morphological examination, but also a functional technique that provides a higher detection rate of additional lesions than mammography and breast ultrasound.5 MRI is typically used for BC staging.6,7 However, according to a meta-analysis study, the incremental cancer detection rate was only 4.2% [95% confidence interval (CI) 2.7–6]; its false-positive rates are still considered high, leading to unnecessary biopsies and eventually surgical procedures that result in benign pathological results.8,9,10
Currently, BC specialists recommend that MRI may be useful for some groups of patients with BC, such as those with: (1) invasive lobular carcinoma;11,12 (2) aggressive types of BC, such as triple-negative and human epidermal growth factor receptor 2-positive tumors;13 (3) dense breast tissue or younger age, especially age < 50 years;14 and (4) those who plan to undergo neoadjuvant treatment.15,16 MRI is also used for BC screening, especially in patients with BRCA-mutated BC17,18,19 and those with BC with metastatic lymph node disease with occult primary;20 however, it is not yet considered a standard of care8,9,10 for preoperative purposes.
In this context, in 2023,21 a newly published randomized trial composed a list of evidence that assessed the impact of MRI in planning BC surgeries.21 The trial conducted by the research group included surgical management, local and systemic recurrences, and survival as important outcomes. Therefore, considering the current evidence, a new systematic review with meta-analyses is required to assess whether a new trial can change previous estimates.
To summarize, we hypothesized that women exposed to MRI might have detrimental outcomes due to a higher risk of extensive surgeries, lower quality of life, and no proven clinical benefits such as survival, disease-free survival, and other cancer-related outcomes. Therefore, the main objective of this study was to assess the effectiveness of MRI as a preoperative tool in women with BC.
Materials and Methods
Protocol Registration and Rationale of Review
PROMRIINE is a systematic review registered at PROSPERO/University York (CRD42023422415).
This study sought to identify the randomized controlled trials (RCTs) that assessed whether MRI exposure in women with BC was associated with higher levels of surgical procedures such as initial mastectomy and reoperation. Therefore, our research question was as follows: “In RCT, what was the clinical impact (surgery-related outcomes and clinical outcomes) of the use of magnetic resonance imaging (MRI) in women with breast cancer?”
Data Sources and Searches
Five databases were screened for studies: PubMed/MEDLINE, Scopus, Cochrane Central Register of Controlled Trials, and Google Scholar (manual search). The searches included manuscripts published between January 2012 and July 2023 with no language restrictions.
Study Selection
Two independent reviewers screened the database on the basis of the title and abstract and included papers that demonstrated adherence to the research strategy defined in the systematic review protocol. If there was disagreement between the two reviewers, a third reviewer assessed the manuscript to determine whether it should be included for data extraction.
Data Extraction
Two independent reviewers extracted the following data (in duplicate) from all included studies: author, year of publication, number of study sites, study design, baseline population information (age), BC staging, receptor status, tumor localization, number of BCSs and mastectomies as initial procedures, the need for reoperation, recurrence, and death. A third reviewer was also available to solve any discrepancies.
Outcomes, Data Synthesis, and Analysis
The main outcomes considered in this review were (1) number of BCSs, (2) number of initial mastectomies, (3) need for reoperation, and (4) need for additional mastectomy. The exploratory outcomes included BC recurrence and death.
The studies are tabulated (Tables 1 and 2). The pooled relative risks were calculated on the basis of the number of events described in each study. Meta-analyses were conducted using R software with a fixed effects model. Heterogeneity was assessed using the I2 method. RCTs were also assessed for the risk of bias, which is available in an MS Excel-based form at https://www.riskofbias.info, and the quality of the evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation GRADE (freely available at http://www.gradeworkinggroup.org). Overall, the risk-of-bias method relies on assessing the quality of randomization, deviations from the initial intervention plan, missing data on outcomes, or selective reporting. GRADE assesses the quality of the evidence by rating the risk of bias and (in)consistency of the summarized outcome from the study and others.
Ethics Approval
Informed consent and ethics approval were not required as this systematic review was based on published studies.
Results
Of the 3403 initially identified studies, 3373 did not have titles or abstracts aligned with the inclusion criteria. After reading 30 studies, the reviewers agreed to include 5 RCTs (Fig. 1).
This review included 3870 randomized women with BC, of whom 1856 underwent MRI and 2014 did not (non-MRI group). The study population comprised women aged 46–61 years with stage I or II BC. When specified, most studies reported women on post-menopausal status (65% of the sample). One study reported data on the localization of the tumor, where approximately 20% of the sample had in situ ductal carcinoma, and two studies reported information on receptor positivity. Mota et al.21 included 13 patients with positive statuses of human epidermal growth factor receptor 2, and Bruck et al.22 included women with hormone receptor-positive BC (Tables 1 and 2).
Initial Surgery: BCS and Mastectomy
MRI was associated with 5% lower rates of BCS [risk ratio (RR) 0.95, 95% CI 0.92–0.97) and increased rates of initial mastectomy (RR 1.59, 95% CI 1.33–1.92). This evidence indicated moderate and high levels of certainty on the basis of the GRADE tool (Figs. 2 and 3; Table 3).
Further Need for Surgery: Any Reoperation and Mastectomy
Using MRI was not statistically different (5% alpha) from the non-MRI group based on the outcomes, such as the need for further reoperation (RR 0.87, 95% CI 0.72–1.05) and additional mastectomies (RR 0.87, 95% CI 0.11–3.89) (Figs. 4 and 5; Table 3).
Recurrence and Death
Only Motta et al.21 reported data on recurrence and death. In this study, MRI use was not considered statistically different from MRI non-use (non-MRI group) (5% alpha) in women with BC with one local recurrence (RR 0.65, 95% CI 0.11–3.89), distant recurrence (RR 0.83, 95% CI 0.23–3.08), or death (RR 1.25, 95% CI 0.55–2.86), as presented in Table 3.
Quality of the Studies and Evidence
Overall, the evidence on BCS as the initial procedure was considered to have moderate certainty due to imprecision in the meta-analysis; however, the outcome was considered critical, and the risk of bias was considered low (not serious). The evidence on mastectomy as the initial procedure as the outcome was considered a “high level of certainty.” As presented in Table 3, reoperation, new mastectomy, recurrence, and death were all considered low certainty because of the lack of statistical significance. Importantly, no study was downgraded due to a lack of blinding because MRI cannot be masked as part of the intervention.
Discussion
The PROMRIINE study is the first systematic review and meta-analysis to include only RCTs that have analyzed the outcomes of MRI in women with BC. The evidence was also assessed through the risk of bias scale and GRADE. Five RCTs were included in our analyses, which are summarized below.
The COMICE Trial23 was a prospective trial in 45 UK centers, with 1623 women. The patients were randomly assigned to undergo either MRI (n = 816) or no further imaging (n = 807). The primary endpoint was the proportion of patients undergoing a repeat operation or further mastectomy within 6 months of random assignment or a pathologically avoidable mastectomy at the initial operation. The addition of MRI to conventional triple assessment was not significantly associated with a reduced reoperation rate, with 153 (19%) requiring reoperation in the MRI group versus 156 (19%) in the non-MRI group (p = 0.77).
The MONET Trial24 RCT in the Netherlands included patients with nonpalpable Breast Imaging-Reporting and Data System (BI-RADS) 3–5 lesions. The patients were randomly assigned to receive routine medical care or additional MRI before biopsy. The primary endpoint was the rate of additional surgical procedures (re-excision or conversion to mastectomy) in patients with nonpalpable BC. A total of 418 patients were randomized: 207 were allocated to the MRI group and 211 to the control group. The primary BCS rate was similar in both groups; however, the number of re-excisions was paradoxically increased in the MRI group 18/53 (34%) versus 6/50 (12%) in the control group (p = 0.008). The number of conversions to mastectomy did not differ significantly between groups.
The POMB Trial25 was a prospective, randomized, multicenter study that included 440 patients aged < 56 years with BC from three Swedish breast units. Patients were randomly allocated (1:1) to either the preoperative staging with breast MRI (n = 220) or no breast MRI (n = 220) group. In patients randomized to the MRI group, a change from suggested breast conservation to mastectomy occurred in 23 of 153 (15%) patients. Breast MRI provided additional information in 83 of 220 (38%) patients, resulting in a change in treatment plan in 40 (18%). The breast reoperation rate was significantly lower in the MRI group: 11 of 220 (5%) versus 33 of 220 (15%) in the control group (p < 0.001). The number of mastectomies, axillary reoperations, and the number of patients receiving neoadjuvant chemotherapy after definitive treatment did not differ significantly between the groups.
Brück et al.22 published an RCT in 2018 from Finland investigating the diagnostic value of preoperative MRI and its impact on short-term surgical outcomes in patients with newly diagnosed unifocal stage I invasive ductal carcinoma. A total of 100 patients were randomized (1:1) to receive either preoperative MRI or to be scheduled directly for surgery. There were 50 patients in both study arms. MRI detected an additional finding in 28%, and in 7%, it was identified as malignant, causing a change in planned surgical management in 10 patients (20%). Mastectomy and reoperation rates were similar in both groups. The mean interval between referral and first surgical procedure was 34 days in the MRI group and 21 days in the control group (p < 0.001).
The BREAST-MRI Trial21 was a phase III, randomized, open-label, single-center Brazilian trial that included female participants with stage 0–III BC who were eligible for BCS. This study compared the role of MRI in preoperative evaluation with that of routine radiologic examinations (mammography and ultrasound) in BCS candidates. The primary outcome was local relapse-free survival, and secondary outcomes were overall survival, mastectomy, and reoperation rates. The study randomized 524 patients to the preoperative MRI group (n = 257) or control group (n = 267); however, the preoperative MRI increased the mastectomy rates by 8%, and the use of preoperative MRI did not influence local relapse-free survival, overall survival, or reoperation rates.
This review revealed that MRI is associated with a 59% increased rate of initial mastectomy as the first procedure and reduced rates of BCS in comparison to those women not exposed to routine MRI.
The frequency at which mastectomy rates are reported does not necessarily indicate the efficacy of MRI in surgical decision-making processes. Several methodological limitations in the existing data compromise its interpretability, including patients already scheduled for BCS; confounding variables such as tumor characteristics or patient-specific factors are often unaccounted for; and mastectomy decisions frequently reflect factors beyond medical necessity, such as surgeon or patient preference, institutional protocols, and socioeconomic or ethnic disparities.26
Furthermore, some studies that reported elevated mastectomy rates associated with MRI did not rigorously validate whether newly identified lesions were benign or malignant. In some cases, histopathological examination of mastectomy specimens has suggested that alterations in the initial surgical approach are not clinically warranted.
Optimal practice guidelines recommend that any additional suspicious lesions identified via MRI be subjected to biopsy or equivalent confirmatory tests if they can potentially modify the surgical strategy. Institutions offering MRI should possess biopsy capabilities to minimize surgical delays and enhance the overall care quality. Additionally, continuously monitoring quality indicators specific to MRI performance is crucial. Proficiency in the entire MRI process, from image acquisition to interpretation, not only improves diagnostic accuracy, but also fosters innovation in the field.27
Most studies in favor of the use of MRI as a preoperative tool have focused on the sensitivity of the method, which is much higher than that of mammography or ultrasound,28 especially for small tumors.5 They further advocate that the identification of additional disease is important for prognosis and cure; however, we know from the studies that additional disease is common29 and does not seem to affect survival.1
Some specialists advocate that MRI should be used to reduce the risk of reoperation. In a meta-analysis conducted by Eisen et al.,26 which amalgamates data from both randomized and retrospective studies, a statistically significant reduction in both reoperation and recurrence rates was observed. However, the robustness of these findings diminishes when prospective and retrospective studies are combined, thereby compromising the impact of the meta-analysis.
In contrast, our study, which exclusively encompassed prospective studies, revealed no statistically significant variations in either recurrence or reoperation rates between the MRI- and non-MRI-exposed populations. Moreover, our data indicate that the utilization of MRI increases the frequency of mastectomy procedures yet does not yield any measurable improvement in recurrence rates.
Another important point would be the improved detection of lobular invasive carcinoma (LIC), both in the index lesion and in a possible foci, as we know that this histological type presents greater multicentricity and bilaterality, and MRI seems to be able to assess better this subtype.12 Unfortunately, none of the RCTs objectively evaluated ILC and none of them were designed to exclusively assess this subtype.
This scientific evidence showed consistent results across the five RCTs and suggests that additional trials should not provide different information from what is already known in terms of surgical outcomes.
It is important to move forward and address different scientific questions. Therefore, future studies should not expose women to unnecessary research.
For example, Mota et al. (2023) was the only study demonstrating the clinical impact of using MRI in BC.21 During short-term follow-up (3 years), MRI did not differ from not using MRI in terms of recurrence and death risks. Many factors, such as the subtype of BC, can impact survival or disease-free survival. However, triple-negative disease can also be detected by MRI (higher sensitivity, 92–100%), as it is characterized as a larger, well-defined, and more necrotic lesion, impacting disease management.30 Histological characterization of BC (e.g., ductal carcinoma in situ or invasive ductal carcinoma) will play an important role in describing the included population in future studies. According to Lee et al. (2020),31 ductal carcinoma in situ was likely to result (p < 0.001) in more surgical plan changes than invasive ductal carcinoma due to the extent of suspicious lesions on breast MRI, detection of additional nodules, and other findings.
Age at menopause and the type of neoadjuvant chemotherapy are also well-characterized covariates to be assessed as they might impact prognosis.32 However, this information was not clearly stated in the studies included in this review.
Finally, breast density is a key factor that may affect physicians’ preference for MRI.33 Despite the importance of breast density, there was considerable heterogeneity in reporting the baseline characteristics of the included patients in the RCTs; some reported body mass index as a proxy for breast density, but no study has reported information on this. Therefore, this might be a relevant gap that can be addressed in future studies about the clinical impact of MRI in the BC population.
The present study has some limitations. Despite relevant findings on surgical outcomes, the amount of data on relevant clinical outcomes, such as recurrence and death, remain limited. Additionally, the absence of relevant baseline information might result in problems interpreting the evidence on neoadjuvant chemotherapies that can alter survival or even breast density, which is associated with more MRI, and possibly, more mastectomies. This study provides scientific information to inform of the benefits of using MRI on surgical outcomes; the uncertain benefits and potential harm of mastectomies should be discussed with women with BC.
This systematic review with meta-analyses provides robust evidence and a relevant discussion on the increased risks of mastectomies and reduced rates of BCS when exposing women with BC to preoperative MRI, which should be considered when offering routine practice to patients with BC before surgery. The lack of relevant baseline characteristics (breast density, age at menopause, tumor type, type of neoadjuvant chemotherapy, and others) and lack of assessment of clinical outcomes (local recurrence, systemic recurrence, event-free survival, and long-term survival) in RCTs suggest the need for further research in this field.
Data availability
All data are available.
References
Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347(16):1227–32.
Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–41.
Pilewskie M, Morrow M. Margins in breast cancer: how much is enough? Cancer. 2018;124(7):1335–41.
Fisher ER, Gregorio R, Redmond C, et al. Pathologic findings from the National Surgical Adjuvant Breast Project (protocol no. 4). I. Observations concerning the multicentricity of mammary cancer. Cancer. 1975;35(1):247–54.
Chen HL, Zhou JQ, Chen Q, et al. Comparison of the sensitivity of mammography, ultrasound, magnetic resonance imaging and combinations of these imaging modalities for the detection of small (≤2 cm) breast cancer. Medicine (Baltimore). 2021;100(26):e26531.
Mann RM, Cho N, Moy L. Breast MRI: state of the art. Radiology. 2019;292(3):520–36.
Kim SY, Cho N. Breast magnetic resonance imaging for patients with newly diagnosed breast cancer: a review. J Breast Cancer. 2022;25(4):263–77.
Brennan ME, Houssami N, Lord S, et al. Magnetic resonance imaging screening of the contralateral breast in women with newly diagnosed breast cancer: systematic review and meta-analysis of incremental cancer detection and impact on surgical management. J Clin Oncol. 2009;27(33):5640–9.
Houssami N, Ciatto S, Macaskill P, et al. Accuracy and surgical impact of magnetic resonance imaging in breast cancer staging: systematic review and meta-analysis in detection of multifocal and multicentric cancer. J Clin Oncol. 2008;26(19):3248–58.
Xu R, Tang P, Li C. Association between pre-operative magnetic resonance imaging (MRI) and surgical outcomes in breast cancer: not yet determined. Breast Cancer Res Treat. 2019;173(3):749–50.
Barker SJ, Anderson E, Mullen R. Magnetic resonance imaging for invasive lobular carcinoma: is it worth it? Gland Surg. 2018;8(3):237–41.
Parvaiz MA, Yang P, Razia E, et al. Breast MRI in invasive lobular carcinoma: a useful investigation in surgical planning? Breast J. 2016;22(2):143–50.
Kazama T, Takahara T, Hashimoto J. Breast cancer subtypes and quantitative magnetic resonance imaging: a systemic review. Life (Basel). 2022;12(4):635.
Mann RM, Athanasiou A, Baltzer PAT, et al. Breast cancer screening in women with extremely dense breasts recommendations of the European Society of Breast Imaging (EUSOBI). Eur Radiol. 2022;32(6):4036–45.
Janssen LM, den Dekker BM, Gilhuijs KGA, et al. MRI to assess response after neoadjuvant chemotherapy in breast cancer subtypes: a systematic review and meta-analysis. NPJ Breast Cancer. 2022;8(1):107.
Reig B, Lewin AA, Du L, et al. Breast MRI for evaluation of response to neoadjuvant therapy. RadioGraphics. 2021;41(3):665–79.
Elezaby M, Lees B, Maturen KE, et al. BRCA mutation carriers: breast and ovarian cancer screening guidelines and imaging considerations. Radiology. 2019;291(3):554–69.
Naranjo ID, Sogani J, Saccarelli C, et al. MRI screening of BRCA mutation carriers: comparison of standard protocol and abbreviated protocols with and without T2-weighted images. AJR Am J Roentgenol. 2022;218(5):810–20.
Warner E, Plewes DB, Hill KA, et al. Surveillance of BRCA1 and BRCA2 mutation carriers with magnetic resonance imaging, ultrasound, mammography, and clinical breast examination. JAMA. 2004;292(11):1317–25.
de Bresser J, de Vos B, van der Ent F, et al. Breast MRI in clinically and mammographically occult breast cancer presenting with an axillary metastasis: a systematic review. Eur J Surg Oncol. 2010;36(2):114–9.
Mota BS, Reis YN, de Barros N, et al. Effects of preoperative magnetic resonance image on survival rates and surgical planning in breast cancer conservative surgery: randomized controlled trial (BREAST-MRI trial). Breast Cancer Res Treat. 2023;198(3):447–61.
Brück N, Koskivuo I, Boström P, et al. Preoperative magnetic resonance imaging in patients with stage I invasive ductal breast cancer: a prospective randomized study. Scand J Surg. 2017;107(1):14–22.
Turnbull L, Brown S, Harvey I, et al. Comparative effectiveness of MRI in breast cancer (COMICE) trial: a randomised controlled trial. Lancet. 2010;375(9714):563–71.
Peters NH, van Esser S, van den Bosch MA, et al. Preoperative MRI and surgical management in patients with nonpalpable breast cancer: the MONET - randomised controlled trial. Eur J Cancer. 2011;47(6):879–86.
Gonzalez V, Sandelin K, Karlsson A, et al. Preoperative MRI of the breast (POMB) influences primary treatment in breast cancer: a prospective, randomized, multicenter study. World J Surg. 2014;38(7):1685–93.
Eisen A, Fletcher GG, Fienberg S et al. Breast magnetic resonance imaging for preoperative evaluation of breast cancer: a systematic review and meta-analysis. Can Assoc Radiol J 2023: 8465371231184769.
Choi WJ, Cha JH, Kim HH, et al. Long-term survival outcomes of primary breast cancer in women with or without preoperative magnetic resonance imaging: a matched cohort study. Clin Oncol (R Coll Radiol). 2017;29(10):653–61.
Aristokli N, Polycarpou I, Themistocleous SC, et al. Comparison of the diagnostic performance of magnetic resonance imaging (MRI), ultrasound and mammography for detection of breast cancer based on tumor type, breast density and patient’s history: a review. Radiography. 2022;28(3):848–56.
Holland R, Veling SH, Mravunac M, et al. Histologic multifocality of Tis, T1–2 breast carcinomas. Implications for clinical trials of breast-conserving surgery. Cancer. 1985;56(5):979–90.
Chen IE, Lee-Felker S. Triple-negative breast cancer: multimodality appearance. Curr Radiol Rep. 2023;11(4):53–9.
Lee J, Jung JH, Kim WW, et al. Efficacy of breast MRI for surgical decision in patients with breast cancer: ductal carcinoma in situ versus invasive ductal carcinoma. BMC Cancer. 2020;20(1):934.
Azzam H, Kamal R, El-Assaly H, et al. The value of dynamic contrast-enhanced MRI in the diagnosis and management of triple-negative breast cancer. Egypt J Radiol Nucl Med. 2020;51(1):26.
Lundberg P, Forsgren MF, Tellman J, et al. Breast density is strongly associated with multiparametric magnetic resonance imaging biomarkers and pro-tumorigenic proteins in situ. Br J Cancer. 2022;127(11):2025–33.
Acknowledgement
We would like to thank Editage (www.editage.com) for English language editing.
Funding
All authors declare that they have no conflicts of interest. This study did not receive any funding or financial grants.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by AM, MA, and LO. The first draft of the manuscript was written by LO and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclosure
All authors declare that they have no conflicts of interest. This study did not receive any funding or financial grants.
Consent to participate
Informed consent and ethics approval were not required as this systematic review was based on published studies.
Consent to publish
Informed consent and ethics approval were not required as this systematic review was based on published studies.
Ethics approval
Informed consent and ethics approval were not required as this systematic review was based on published studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mattar, A., Antonini, M., Amorim, A. et al. PROMRIINE (PRe-operatory Magnetic Resonance Imaging is INEffective) Study: A Systematic Review and Meta-analysis of the Impact of Magnetic Resonance Imaging on Surgical Decisions and Clinical Outcomes in Women with Breast Cancer. Ann Surg Oncol (2024). https://doi.org/10.1245/s10434-024-15833-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1245/s10434-024-15833-5