Abstract
Background
This study sought to identify associations between the Yost Index, a geocoded area neighborhood socioeconomic status (nSES) score, and race/ethnicity with patient refusal of recommended surgery for metastatic bone disease.
Methods
Patients with metastatic bone disease were extracted from the Surveillance, Epidemiology, and End Results database. The Yost Index was geocoded using factor analysis and categorized into quintiles using census tract-level American Community Service (ACS) 5-year estimates and seven nSES measures. Multivariable logistic regression models calculated odds ratios (ORs) of refusal of recommended surgery and 95% confidence intervals (CIs), adjusting for clinical covariates.
Results
A total of 138,257 patients were included, of which 14,943 (10.8%) were recommended for surgical resection. Patients in the lowest nSES quintile had 57% higher odds of refusing surgical treatment than those in the highest quintile (aOR = 1.57, 95% CI 1.30–1.91, p < 0.001). Patients in the lowest nSES quintile also had a 31.2% higher age-adjusted incidence rate of not being recommended for surgery compared with those in the highest quintile (186.4 vs. 142.1 per 1 million, p < 0.001). Black patients had 34% higher odds of refusing treatment compared with White patients (aOR = 1.34, 95% CI 1.14–1.58, p = 0.003). Advanced age, unmarried status, and patients with aggressive cancer subtypes were associated with higher odds of refusing surgery (p < 0.001).
Conclusions
nSES and race/ethnicity are independent predictors of a patient refusing surgery for metastatic cancer to bone, even after adjusting for various clinical covariates. Effective strategies for addressing these inequalities and improving the access and quality of care of patients with a lower nSES and minority backgrounds are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An average of 350,000 people die from metastatic disease with osseous extension each year.1 Patients who suffer from bone metastases have an increased risk of fracture, bone pain, spinal cord compression, and the need for radiotherapy among other eventualities. In 2022, the National Cancer Institute (NCI) recognized these patients with metastatic cancer as a frequently overlooked subpopulation of cancer survivors who often face burdensome physical and psychological symptoms and have complex care needs.2
Previous research has highlighted persistent socioeconomic and insurance-related disparities in the outcomes of ethnic and racial minorities living with metastatic bone disease.3,4,5 The exact causes of these disparities are complex and multifactorial, with patient, provider, and system-related factors playing a role.6,7,8,9,10,11,12 Understanding the factors that impact the decision of when to receive care, when to accept care, and how to deal with end-stage disease, such as metastatic cancer remains crucial.13 Within this context, one critical aspect that warrants closer examination is the refusal of recommended surgery.14 The decision to accept or decline surgical interventions can be influenced by a myriad of factors, many of which are intertwined with a patient's nSES.14 While previous studies have studied the refusal of recommended surgical intervention in patients with cancers of the colon, head and neck, breast, pancreas, and non-small cell lung cancer, no studies have specifically examined the association between nSES/racial differences in refusal of recommended surgery for patients living with metastatic bone disease.14,15,16,17,18,19,20,21
This work examined nSES by using the Yost Index22,23—a composite score that is geocoded using census tract-level American Community Service (ACS) 5-year estimates and seven primary measures: median household income, median house value, median rent, percent below 150% of poverty line, Education Index, percent working class, and percent unemployed. The purposes of this work are (1) to determine whether there is a variation in the demographics or characteristics of patients with metastatic cancer to the bones and joints based on the rationale for not receiving cancer-directed surgery and (2) to characterize the association between race/ethnicity and Yost Index with patient refusal of surgical intervention among individuals living with metastatic cancer to the bones and joints. Results may permit the development of interventions to improve access and quality of care for patients from lower nSES backgrounds.
Methods
Study Design and Participants
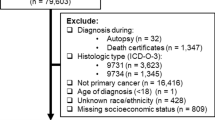
This was a retrospective, cross-sectional analysis of the population-based data of individuals diagnosed with metastatic cancer to the bone and joints between 2010 and 2018. Patient data were extracted from the SEER 18 database, a network of population-based cancer registries that includes geographic regions of the United States that covers approximately 28% of the population. The SEER 18 database provides information on cancer incidence, survival, and treatment modalities, such as radiation therapy, surgery, and chemotherapy. Of note, the SEER registry does not include information on comorbidities, performance status, surgical pathology, margin status, doses, or agents. To identify patients with bone and joint metastases, we utilized the comprehensive set of International Classification of Disease (ICD-10) codes listed in Table 1. Patients who were diagnosed solely via autopsy or death certificate were excluded from this analysis. The STROBE flow diagram in Fig. 1 illustrates the criteria used for participant inclusion and exclusion in the study.
Yost Index and nSES Quintiles
The Yost Index is an effective measure of socioeconomic vulnerability, as validated in previous cancer research studies.24,25,26 The index’s quintiles were calculated via a two-step process using census tract-level American Community Service (ACS) 5-year estimates that were standardized across the entire United States. The first step involved a factor analysis using the following seven variables representing different aspects of nSES: Education (a weighted index that incorporates educational achievement levels, encompassing less than high school completion, high school diplomas, and college degrees), Percent below 150% of poverty line, Percent working class, Percent unemployed, Median rent, Median house value, and Median household income. The second step classified census tracts into nSES quintiles based on equal populations across the United States. The lowest nSES group (first quintile) corresponds with the 20th percentile or lower, whereas the highest nSES group (fifth quintile) corresponds with the 80th percentile or higher. These nSES quintiles were then matched to tumor cases at the census tract level by aligning the ACS survey year with the tumor diagnosis year.
Statistical Analysis
SEER*Stat 8.4.126 and RStudio version 1.1.383 were used to perform statistical analyses. Objective 1 involved summarizing patient demographics by age at diagnosis, sex, and race/ethnicity. Chi-squared and analysis of variance (ANOVA) were utilized to assess whether any significant differences existed in the basic clinical covariates between varying reasons for not undergoing cancer surgery. Objective 2 used multivariable logistic regression models, with adjusted odds ratios (aORs) with 95% CIs calculated using the exact method. This was undertaken to identify prognostic factors linked to the refusal of surgery, where aOR <1 was deemed a favorable prognostic factor for undergoing surgery and aOR >1 a poor prognostic factor for undergoing surgery. The primary outcome of interest was undergoing recommended surgery of the primary histological site, which was categorized as (1) recommended and performed or (2) recommended but refused by the patient. The key predictor variables were nSES (Yost Index quintile) and race, which was categorized as White, Black, Asian/Pacific Islander (API), or American Indian/Alaskan Native (AI/AN). Other covariates that were included as potential confounders included age, sex, marital status, urban/metropolitan recode, and primary cancer site. Age-adjusted incidence rates were also calculated for the various reasons for either undergoing or not undergoing surgical treatment and were independently stratified by race and nSES. Age-adjusted incidence rates were calculated and standardized to the 2000 U.S. Standard Population (Census P25-1130). Statistical significance was determined by using the Wald test. All hypotheses were one-sided, and P < 0.05 was regarded as significant.
Results
Patient Demographics and Characteristics
A total of 138,257 patients (2010–2018) with de novo metastatic cancer to the bone and joints from the top ten prevalent primary cancer sites were abstracted from SEER. Of these, 14,943 (10.8%) of these patients had some sort of surgery recommended. Mean age was 67.7 (SD = 12.2), and the majority of patients were male (58.8%, n = 81,759), White (78.8%, n = 109,585), married (53.8%, n = 74,778), and living in a metropolitan area (87.2%, n = 121,190). Table 2 shows baseline covariates among the study patient population, stratified by reasons for not undergoing cancer-directed surgical resection. Of all of the patients who had surgery recommended, 19.6% refused. Reasons for this were unknown (9.8%, n = 1469), active surgical refusal (7.9%, n = 1178), and mortality before surgery (1.9%, n = 282). Among those patients who refused surgery, 55.9% were female (n = 659) and 64.4% were single (n = 759). Surgery was most recommended and performed in patients whose primary cancers were breast (35.8%, n = 4302) and prostate (20.5%, n = 2459).
Factors Associated with Refusing Surgical Treatment
Table 3 shows the direction, magnitude, and precision of the estimated associations between patient race and nSES with refusal of surgery both prior and after adjustment for clinical covariate confounders. Patients who are older at diagnosis were significantly more likely to have refused surgical treatment (aOR 1.07, 95% CI 1.06–1.07, per each additional year). nSES also was a persistent independent predictor of refusing surgical treatment even after adjustment for age, sex, race, marital status, urban/rural status, and primary cancer site. Patients with the lowest nSES had 57% higher odds of refusing surgical treatment compared with patients with the highest nSES (aOR 1.57, 95% CI 1.30–1.91, p < 0.001). Black patients were 34% more likely to refuse treatment compared with White patients (aOR 1.34, 95% CI 1.14–1.58, p = 0.003). Single patients were approximately twice as likely to refuse treatment compared with married patients (aOR 2.10, 95% CI 1.87–2.36, p < 0.001).
Race/Ethnicity, nSES, and Reasons for No-cancer-directed Surgical Resection
Table 4 shows the age-adjusted incidence rates of patients with metastatic cancer to the bone and joints stratified by Yost Index quintiles and their reasons for not undergoing surgical intervention. Patients in the lowest nSES quintile were most likely to not have surgery recommended (186.4 per 1 million, 95% CI 184.0–188.7; SE 1.2) compared with patients in the highest nSES quintile (142.1, 95% CI 140.6–143.7; SE 0.8). Patients in the lowest nSES quintile also had the highest rate of being contraindicated for surgery due to comorbid conditions (6.9, 95% CI 6.4–7.3; SE 0.2) compared with patients in the highest nSES quintile (3.7, 95% CI 3.4–3.9; SE 0.1). Patients in the lowest nSES quintile also were more likely to refuse offered surgery or not undergo a procedure for unknown reasons (2.2, 95% CI 2.0–2.5; SE 0.1 and 3.3, 95% CI 3.0–3.7; SE 0.2, respectively) than those in the highest nSES quintile (1.1, 95% CI 1.0–1.3; SE 0.1 and 1.2, 95% CI 1.1–1.4; SE 0.1, respectively).
Table 5 shows the age-adjusted incidence rates of patients living with metastatic cancer to the bone and joints stratified by race and ethnicity and their reasons for not undergoing surgery. Black patients were less likely to be recommended for surgery (186.4 per 1 million, 95% CI 184.0–188.7; SE 1.2) than White patients (142.1, 95% CI 140.6–143.7; SE 0.8). Black patients were also more likely to be contraindicated for surgery due to comorbid conditions (6.9, 95% CI 6.4–7.3; SE 0.2) compared with White patients (3.7, 95% CI 3.4–3.9; SE 0.1). Black patients were more likely to either refuse surgery or not have surgery for unknown reasons (2.2, 95% CI 2.0–2.5; SE 0.1 and 3.3, 95% CI 3.0–3.7; SE 0.2, respectively) compared with White patients (1.1, 95% CI 1.0–1.3; SE 0.1 and 1.2, 95% CI 1.1–1.4; SE 0.1, respectively). A first-order interaction between Race and the Yost Index was not statistically significant (p > 0.05), indicating that race did not modify the effect of the Yost index on refusal of recommended surgical resection. Likewise, a first-order interaction between marital status was not statistically significant (p > 0.05), indicating that marital status did not modify the effect of the Yost index on refusal of recommended surgical resection.
Discussion
Metastatic disease to bone has a poor prognosis and is a source of significant psychological and physical stress.2 The complex care and psychosocial needs of patients living with metastatic disease can modulate their indication for and acceptance of surgical intervention. The present work sought to understand whether socioeconomic factors were independently predictive of patient acceptance of offered surgery, finding that both race and socioeconomic status influenced the decision to undergo surgery. The decision to recommend surgery is influenced by performance status, systemic disease burden, mechanical stability, fracture risk, neurological risk, and life expectancy.27,28 Resection can be beneficial in patients with spinal metastases when surgery is expected to prolong life, and relieve symptoms, and in the combination with radiotherapy has become the standard therapy for eligible patients in the past decades.29,30,31 Although treatment is generally considered to be palliative, surgery aims to maintain spinal stability and increase quality of living.32 Multiple scores have been developed to estimated survival of patients and establish a cutoff for surgical referral in these patients; however, there is no universally recommended treatment strategy.29 Of patients with de novo metastatic cancer to the bone and joints from the top ten most prevalent primary cancer sites, only a minority of patients analyzed in our study were offered surgery (13.5%). Treatment options include en bloc spondylectomy, decompression of the spinal cord followed by stereotactic radiosurgery (“separation surgery”) and palliative surgery to ensure spinal stability via cement augmentation or release neurological symptoms via decompression.29 As advancements in the treatment of spinal tumors continue to progress and patients experience longer survival rates, surgical interventions are anticipated to play an increasingly significant role in the management of metastases. The present work reports that specific patient factors were predictive of refusing surgical treatment.
Older patients were more likely to refuse surgical treatment (aOR 1.07, 95% CI 1.06–1.07, per each additional year), which supports current literature that suggests that older patients are less likely to proceed with cancer treatment or surgical intervention.33,34,35,36 Several mechanisms may underlie elderly patient refusal of surgery, including the changing balance between the risks and benefits of surgery in an individual with a decreased potential lifespan that may lead to a greater emphasis on quality of life rather than lengthening survival.34,37 Older patients also may be in worse health and have significant comorbidities, which may impact their decision to proceed with invasive therapy.36
Our data support previous literature that marital status plays an important role in surgical utilization broadly and within oncology, with higher rates of refusing surgery among patients who were unmarried.33,34,35 This may underscore the need for financial, social, and physical support in driving patients to seek treatment and through the recovery process.38 Previous studies have reported that married couples share emotional burden, thus alleviating some of the cancer patient’s emotional distress and promoting the importance of survival.39 Our studied also showed that women were less likely to undergo surgery, which is consistent with the larger body of literature on female surgical utilization patterns.33,34,35 While causes of this trend have been proposed, to our knowledge no consensus has been achieved regarding this explain this utilization disparity, particularly in orthopedic surgery.40
Black patients were 35% more likely to refuse treatment than White patients. Previous works have highlighted differences in the personal influences on treatment discussions between races. Race and ethnicity dictated the final decision maker in the management of older breast cancer patients, with varying reliance on physician recommendations and family member input.41 A previous SEER study showed that not only are refusal rates higher among African Americans, these differences persisted, albeit narrowed, after adjusting for insurance type and marital status.33 While current studies have shown that the race gap in healthcare outcomes has decreased but remains associated with declining poverty levels in the Black and Hispanic populations,42,43,44,45,46 our study indicates that a substantial gap still persists in the patient’s decision to undergo surgery for metastatic bone disease. It is evident that while current interventions targeting outcome disparities between racial and ethnic populations may be effective, a focus should be placed on the barriers and personal factors that influence a patient’s decision to proceed with treatment.
nSES was a consistent independent predictor of refusing surgical treatment, even when controlling for covariates. Patients in the lowest nSES quintile were less likely to have surgery recommended to them and were more likely to be contraindicated for surgery because of comorbid conditions. Patients in the lowest nSES quintile also were 57% more likely to refuse surgery or not undergo surgery for unknown reasons (aOR 1.57, 95% CI 1.30–1.91, p < 0.001). While this has not been previously reported in orthopedic procedures, there is mixed oncologic data concerning nSES and the decision to undergo surgery. One previous study found that low neighborhood socioeconomic status was associated with increased surgery utilization among metastatic breast cancer patients.47 Another study found that low nSES patients less likely to go undergo surgery for pancreatic cancer.48 Factors closely associated with nSES, such as social and financial support, type of work, and non-English first language, may act as barriers and additive influences on patient decision-making for surgical intervention.49 Despite this understanding, there is limited literature on the main drivers of how nSES affects patient decision-making in the setting of metastatic disease, especially to bone. The present work suggests that the variables used in the Yost Index, such as income, class, and household characteristics, individually or synergistically contribute to patient decision-making.
The Yost Index served as a measure of neighborhood socioeconomic status (nSES) in this study, which encompassed employment, income, living conditions, infrastructure, education, and the social environment. These characteristics have individually shown to influence patient care and outcomes.50,51,52 A comprehensive review conducted by Sorice et al.53 compared indices of nSES and found that the Yost-Index was a reliable tool to assess patients’ vulnerability. Living in deprived neighborhoods has been linked to various health risks, including higher air pollution,54 decreased quality of sleep,55 and inflammation.56 Living in a safe, walkable environment with low crime rates and desirable recreational areas, such as parks, promotes physical and mental health.57,58,59,60 Lower neighborhood socioeconomic status has been linked to increased mortality risk.61,62 There is strong evidence in literature that moving from high-poverty to lower-poverty neighborhoods can have a positive long-term effect on mental and physical well-being.63 Lower nSES also has been associated with decreased mental health and reduced cognitive function.57,64 Residents of affluent neighborhoods have been linked to more favorable dietary patterns65,66 and demonstrated a reduced likelihood of enga/ging in alcoholism and smoking.67 They also have been shown to exhibit a higher capacity to quit smoking68 and a better adherence to prescription medications and adherence to cancer screening.69,70 Nouri et al.71 found that documentation of advanced healthcare planning was significantly inferior in patients with lower nSES compared with individuals living in more affluent areas, even after adjusting for amount of care encounters. While education and language barrier can affect patients understanding of treatment instructions and planning, there is a lack of understanding of healthcare providers which factors influence health-seeking behaviors.72 Social beliefs highly influence patients’ interactions with medical providers and racial minorities were shown to exhibit lower level of trust in the healthcare system with higher rates of refusal of care.73,74 Jakobsen et al.75 found that residents of deprived neighborhoods exhibited a lack of trust which could negatively influence engagement with health care providers.
However, it remains unclear to which extend these factors interfere with decision making and refusal of surgery. We analyzed patients that had already encountered healthcare providers and were recommended for surgery; thus, access to health care alone is unlikely to explain our findings. The link of nSES with refusal of surgical care specifically indicates a deeper systematic discrepancy, that surprisingly persisted independently of race or ethnicity. Identifying risk groups is crucial for providing universal health standards and understanding factors that affecting decision making and clinical outcomes in patients. For instance, patients in rural areas may face limited access to high-capacity healthcare facilities, leading to less favorable treatment responses.76,77 Insufficient access to medical care centers complicates follow-up and postsurgical rehabilitation, with neighborhood socioeconomic status impacting recovery in stroke survivors.76,78 Moreover, zip code areas have been shown to affect care fragmentation, influencing outcomes in cancer patients.79 As elaborated, neighborhood and living environment have been shown to effect mental health and belief systems that are highly likely to influence social interaction and health seeking behavior. However, it remains unclear to which extend these socioeconomic factors are associated with decision making, and our study aimed to gain novel insight into understanding that relationship by analyzing refusal of surgical management and neighborhood socioeconomic factors encompassed by the Yost index.
There are several strengths to this study. The study population from this database represents the racial and ethnic heterogeneity of the United States. The database includes data from 18 national cancer registries from geographically, racially, and ethnically diverse U.S. regions.80 A standardized approach for calculating Yost Index quintiles for census tracts across the entire United States was utilized in making nSES comparisons. In standardizing different states and regions, across measures of economic development, population density, race, and other contributing factors, the authors could make direct nSES comparisons. Validated studies have shown that nSES is better quantified by census tract variables than county-level variables22 due to the smaller size and decreased economic diversity of census tracts. Finally, this work is novel in its comprehensive approach to metastatic disease to bone, including 13 ICD-0-3 codes and a majority of the bones of the human body.
There are several limitations to this work beyond those intrinsic to any retrospective database study. First, data collection on insurance status might serve as a confounding variable within this study. The SEER Census Tract-level nSES and Rurality Database that was used in this study was not compatible with SEER-Medicare data, so it was not possible to further assess insurance status. Another limitation of this study was that due to inconsistencies in merging the 7th and 8th AJCC editions, which covered the span of the study period, we did not include tumor T and N stage in this analysis. Given the study population was all metastatic at diagnosis, AJCC M stage and stratification by primary cancer subtype likely has a larger impact than T and N stage on mortality. Last, misclassification of cancer-related deaths is possible, as local or regional relapses may be incorrectly classified as a new cancer or metastasis to an adjacent organ may be misattributed.
Data Availability
This cross-sectional study utilized data from the publicly accessible Surveillance, Epidemiology, and End Results (SEER) database of the National Cancer Institute (https://seer.cancer.gov/). Because the data is publicly available, no institutional review board review was necessary. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
References
Coleman RE, Roodman, Smith, Body, Suva, Vessella. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res. 2006;12(20):6243–9. https://doi.org/10.1158/1078-0432.CCR-06-0931.
Mollica MA, Smith AW, Tonorezos E, et al. Survivorship for individuals living with advanced and metastatic cancers: National Cancer Institute Meeting Report. JNCI J Natl Cancer Inst. 2022;114(4):489–95. https://doi.org/10.1093/JNCI/DJAB223.
Diessner BJ, Weigel BJ, Murugan P, Zhang L, Poynter JN, Spector LG. Associations of socioeconomic status, public versus private insurance, and race/ethnicity with metastatic sarcoma at diagnosis. JAMA Netw Open. 2020;3(8):e2011087–e2011087. https://doi.org/10.1001/JAMANETWORKOPEN.2020.11087.
Jawad MU, Pollock BH, Wise BL, et al. Sex, racial/ethnic and socioeconomic disparities in patients with metastatic bone disease. J Surg Oncol. 2022;125(4):766. https://doi.org/10.1002/JSO.26765.
Jawad MU, Pollock BH, Wise BL, et al. Socioeconomic and insurance-related disparities in disease-specific survival among patients with metastatic bone disease. J Surg Oncol. 2023;127(1):159–73. https://doi.org/10.1002/JSO.27097.
Dodwell E, Wright J, Widmann R, Edobor-Osula F, Pan TJ, Lyman S. Socioeconomic factors are associated with trends in treatment of pediatric femoral shaft fractures, and subsequent implant removal in New York State. J Pediatr Orthop. 2016;36(5):459–64. https://doi.org/10.1097/BPO.0000000000000494.
Hausmann LRM, Mor M, Hanusa BH, et al. The effect of patient race on total joint replacement recommendations and utilization in the orthopedic setting. J Gen Intern Med. 2010;25(9):982–8. https://doi.org/10.1007/S11606-010-1399-5/TABLES/3.
Hausmann LRM, Hanusa BH, Kresevic DM, et al. Orthopedic communication about osteoarthritis treatment: Does patient race matter? Arthritis Care Res (Hoboken). 2011;63(5):635–42. https://doi.org/10.1002/ACR.20429.
Sood A, Gonzalez-Lomas G, Gehrmann R. Influence of health insurance status on the timing of surgery and treatment of bucket-handle meniscus tears. Orthop J Sports Med. 2015. https://doi.org/10.1177/2325967115584883.
Dykes DC, White AA. Getting to equal: strategies to understand and eliminate general and orthopaedic healthcare disparities. Clin Orthop Relat Res. 2009;467(10):2598–605. https://doi.org/10.1007/S11999-009-0993-5/TABLES/1.
Ward E, Jemal A, Cokkinides V, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54(2):78–93. https://doi.org/10.3322/CANJCLIN.54.2.78.
Miller BJ, Gao Y, Duchman KR. Socioeconomic measures influence survival in osteosarcoma: an analysis of the National Cancer Data Base. Cancer Epidemiol. 2017;49:112–7. https://doi.org/10.1016/J.CANEP.2017.05.017.
Fourman MS. CORR Insights®: Are there racial or socioeconomic disparities in ambulatory outcome or survival after oncologic spine surgery for metastatic cancer? Results from a medically underserved center. Clin Orthop Relat Res. 2023;481(2):308–11. https://doi.org/10.1097/CORR.0000000000002510.
Hu X, Ye H, Yan W, Sun Y. Factors associated with patient’s refusal of recommended cancer surgery: based on surveillance, epidemiology, and end results. Front Public Health. 2022;9:785602. https://doi.org/10.3389/FPUBH.2021.785602/BIBTEX.
Makar GS, Makar M, Obinero C, Davis W, Gaughan JP, Kwiatt M. Refusal of cancer-directed surgery in patients with colon cancer: risk factors of refusal and survival data. Ann Surg Oncol. 2021;28(2):606–16. https://doi.org/10.1245/S10434-020-08783-1/FIGURES/3.
Crippen MM, Elias ML, Weisberger JS, et al. Refusal of cancer-directed surgery in head and neck squamous cell carcinoma patients. Laryngoscope. 2019;129(6):1368–73. https://doi.org/10.1002/LARY.27116.
Gaitanidis A, Alevizakos M, Tsalikidis C, Tsaroucha A, Simopoulos C, Pitiakoudis M. Refusal of cancer-directed surgery by breast cancer patients: risk factors and survival outcomes. Clin Breast Cancer. 2018;18(4):e469–76. https://doi.org/10.1016/J.CLBC.2017.07.010.
Tohme S, Kaltenmeier C, Bou-Samra P, Varley PR, Tsung A. Race and health disparities in patient refusal of surgery for early-stage pancreatic cancer: an NCDB cohort study. Ann Surg Oncol. 2018;25(12):3427–35. https://doi.org/10.1245/S10434-018-6680-6/TABLES/3.
Mehta RS, Lenzner D, Argiris A. Race and health disparities in patient refusal of surgery for early-stage non-small cell lung cancer: a SEER cohort study. Ann Surg Oncol. 2012;19(3):722–7. https://doi.org/10.1245/S10434-011-2087-3/TABLES/2.
Groeneveld PW, Kwoh CK, Mor MK, et al. Racial differences in expectations of joint replacement surgery outcomes. Arthritis Care Res (Hoboken). 2008;59(5):730–7. https://doi.org/10.1002/ART.23565.
Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Differences in expectations of outcome mediate African American/white patient differences in “willingness” to consider joint replacement. Arthritis Rheum. 2002;46(9):2429–35. https://doi.org/10.1002/ART.10494.
Yu M, Tatalovich Z, Gibson JT, Cronin KA. Using a composite index of socioeconomic status to investigate health disparities while protecting the confidentiality of cancer registry data. Cancer Causes Control. 2014;25(1):81–92. https://doi.org/10.1007/S10552-013-0310-1/FIGURES/5.
Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control. 2001;12(8):703–11. https://doi.org/10.1023/A:1011240019516/METRICS.
Potter AL, Haridas C, Neumann K, et al. Incidence, timing, and factors associated with suicide among patients undergoing surgery for cancer in the US. JAMA Oncol. 2023;9(3):308–15. https://doi.org/10.1001/JAMAONCOL.2022.6549.
Ellis L, Canchola AJ, Spiegel D, Ladabaum U, Haile R, Gomez SL. Racial and ethnic disparities in cancer survival: The contribution of tumor, sociodemographic, institutional, and neighborhood characteristics. J Clin Oncol. 2018;36(1):25–33. https://doi.org/10.1200/JCO.2017.74.2049.
Rajeshuni N, Zubair T, Ludwig CA, Moshfeghi DM, Mruthyunjaya P. Evaluation of racial, ethnic, and socioeconomic associations with treatment and survival in uveal melanoma, 2004–2014. JAMA Ophthalmol. 2020;138(8):876–84. https://doi.org/10.1001/JAMAOPHTHALMOL.2020.2254.
Confavreux CB, Follet H, Mitton D, Pialat JB, Clézardin P. Fracture risk evaluation of bone metastases: a burning issue. Cancers (Basel). 2021;13(22):5711. https://doi.org/10.3390/CANCERS13225711.
Conti A, Acker G, Kluge A, et al. Decision making in patients with metastatic spine. The role of minimally invasive treatment modalities. Front Oncol. 2019. https://doi.org/10.3389/FONC.2019.00915.
Al Farii H, Aoude A, Al Shammasi A, Reynolds J, Weber M. Surgical management of the metastatic spine disease: a review of the literature and proposed algorithm. Global Spine J. 2023;13(2):486–98. https://doi.org/10.1177/21925682221146741.
Falicov A, Fisher CG, Sparkes J, Boyd MC, Wing PC, Dvorak MF. Impact of surgical intervention on quality of life in patients with spinal metastases. Spine (Phila Pa 1976). 2006;31(24):2849–56. https://doi.org/10.1097/01.BRS.0000245838.37817.40.
Itshayek E, Cohen JE, Yamada Y, et al. Timing of stereotactic radiosurgery and surgery and wound healing in patients with spinal tumors: a systematic review and expert opinions. Neurol Res. 2014;36(6):510–23. https://doi.org/10.1179/1743132814Y.0000000380.
Kurisunkal V, Gulia A, Gupta S. Principles of management of spine metastasis. Indian J Orthop. 2020;54(2):181–93. https://doi.org/10.1007/S43465-019-00008-2.
Hu X, Ye H, Yan W, Sun Y. Factors associated with patient’s refusal of recommended cancer surgery: based on surveillance, epidemiology, and end Results. Front Public Health. 2022. https://doi.org/10.3389/FPUBH.2021.785602.
Clark J, Hudak P, Hawker G, JBJS PC, 2004 undefined. The moving target: a qualitative study of elderly patients’ decision-making regarding total joint replacement surgery. journals.lww.com. Accessed May 6, 2023. https://journals.lww.com/jbjsjournal/Fulltext/2004/07000/The_Moving_Target__A_Qualitative_Study_of_Elderly.3.aspx?__hstc=215929672.82af9c9a98fa600b1bb630f9cde2cb5f.1535587200299.1535587200300.1535587200301.1&__hssc=215929672.1.1535587200302&__hsfp=2025384311&casa_token=CDdGz8W3RY4AAAAA:Q1LFCSxQIMIEd_To4ZI3KREKHAonq60jguRo3act8KEyBY_i1NzMWdcSLBwL-gjcxTUO0yUcjT6QDa-iGP8Opqg
Makar GS, Makar M, Obinero C, Davis W, Gaughan JP, Kwiatt M. Refusal of cancer-directed surgery in patients with colon cancer: risk factors of refusal and survival data. Ann Surg Oncol. 2021;28(2):606–16. https://doi.org/10.1245/S10434-020-08783-1.
Sio TT, Chang K, Jayakrishnan R, et al. Patient age is related to decision-making, treatment selection, and perceived quality of life in breast cancer survivors. World J Surg Oncol. 2014;12(1):230. https://doi.org/10.1186/1477-7819-12-230.
Wedding U, Pientka L, Höffken K. Quality-of-life in elderly patients with cancer: a short review. Eur J Cancer. 2007;43(15):2203–10. https://doi.org/10.1016/J.EJCA.2007.06.001.
Boen CE, Barrow DA, Bensen JT, et al. Social relationships, inflammation, and cancer survival. Cancer Epidemiol Biomarkers Prev. 2018;27(5):541–9. https://doi.org/10.1158/1055-9965.EPI-17-0836.
Goldzweig G, Andritsch E, Hubert A, et al. Psychological distress among male patients and male spouses: What do oncologists need to know? Ann Oncol. 2010;21(4):877–83. https://doi.org/10.1093/ANNONC/MDP398.
Borkhoff CM, Hawker GA, Wright JG. Patient gender affects the referral and recommendation for total joint arthroplasty. Clin Orthop Relat Res. 2011;469(7):1829–37. https://doi.org/10.1007/S11999-011-1879-X.
Maly RC, Umezawa Y, Ratliff CT, Leake B. Racial/ethnic group differences in treatment decision-making and treatment received among older breast carcinoma patients. Cancer. 2006;106(4):957–65. https://doi.org/10.1002/CNCR.21680.
Sun T, Wang S, Sun H, Wen J, An G, Li J. Improved survival in multiple myeloma, with a diminishing racial gap and a widening socioeconomic status gap over three decades. Leuk Lymphoma. 2018;59(1):49–58. https://doi.org/10.1080/10428194.2017.1335398/SUPPL_FILE/ILAL_A_1335398_SM0185.DOC.
Truong B, Green AL, Friedrich P, Ribeiro KB, Rodriguez-Galindo C. Ethnic, racial, and socioeconomic disparities in retinoblastoma. JAMA Pediatr. 2015;169(12):1096–104. https://doi.org/10.1001/JAMAPEDIATRICS.2015.2360.
Kish JK, Yu M, Percy-Laurry A, Altekruse SF. Racial and ethnic disparities in cancer survival by neighborhood socioeconomic status in surveillance, epidemiology, and end results (SEER) registries. JNCI Monographs. 2014;2014(49):236–43. https://doi.org/10.1093/JNCIMONOGRAPHS/LGU020.
Ailawadhi S, Frank RD, Advani P, et al. Racial disparity in utilization of therapeutic modalities among multiple myeloma patients: a SEER-medicare analysis. Cancer Med. 2017;6(12):2876–85. https://doi.org/10.1002/CAM4.1246.
De La Garza Ramos R, Javed K, Ryvlin J, Gelfand Y, Murthy S, Yassari R. Are there racial or socioeconomic disparities in ambulatory outcome or survival after oncologic spine surgery for metastatic cancer? Results from a medically underserved center. Clin Orthop Relat Res. 2023;481(2):301–7. https://doi.org/10.1097/CORR.0000000000002445.
Bhattacharyya O, Li Y, Fisher JL, et al. Low neighborhood socioeconomic status is associated with higher mortality and increased surgery utilization among metastatic breast cancer patients. Breast. 2021;59:314–20. https://doi.org/10.1016/J.BREAST.2021.08.003.
Bakens MJAM, Lemmens VEPP, de Hingh IHJT. Socio-economic status influences the likelihood of undergoing surgical treatment for pancreatic cancer in the Netherlands. HPB (Oxford). 2017;19(5):443–8. https://doi.org/10.1016/J.HPB.2017.01.010.
Modi CS, Veillette CJH, Gandhi R, Perruccio AV, Rampersaud YR. Factors that influence the choice to undergo surgery for shoulder and elbow conditions. Clin Orthop Relat Res. 2014;472(3):883–91. https://doi.org/10.1007/S11999-013-3357-0.
Daniel H, Bornstein SS, Kane GC, et al. Addressing social determinants to improve patient care and promote health equity: an American College of Physicians Position Paper. Ann Intern Med. 2018;168(8):577–8. https://doi.org/10.7326/M17-2441.
Kendzor DE, Reitzel LR, Mazas CA, et al. Individual- and area-level unemployment influence smoking cessation among African Americans participating in a randomized clinical trial. Soc Sci Med. 2012;74(9):1394–401. https://doi.org/10.1016/J.SOCSCIMED.2012.01.013.
Crapo PA, Kolterman OG, Henry RR. Metabolic consequence of two-week fructose feeding in diabetic subjects. Diabetes Care. 1986;9(2):111–9. https://doi.org/10.2337/DIACARE.9.2.111.
Sorice KA, Fang CY, Wiese D, et al. Systematic review of neighborhood socioeconomic indices studied across the cancer control continuum. Cancer Med. 2022;11(10):2125–44. https://doi.org/10.1002/CAM4.4601.
Steppuhn H, Laußmann D, Baumert J, et al. Individual and area-level determinants associated with C-reactive protein as a marker of cardiometabolic risk among adults: results from the German National Health Interview and Examination Survey 2008–2011. PLoS One. 2019;14(2):e0211774. https://doi.org/10.1371/JOURNAL.PONE.0211774.
Rumble DD, O’Neal K, Overstreet DS, et al. Sleep and neighborhood socioeconomic status: a micro longitudinal study of chronic low-back pain and pain-free individuals. J Behav Med. 2021;44(6):811–21. https://doi.org/10.1007/S10865-021-00234-W.
Iyer HS, Hart JE, James P, et al. Impact of neighborhood socioeconomic status, income segregation, and greenness on blood biomarkers of inflammation. Environ Int. 2022;162:107164. https://doi.org/10.1016/J.ENVINT.2022.107164.
Byrne T, Prvu Bettger J, Brusilovskiy E, Wong YLI, Metraux S, Salzer MS. Comparing neighborhoods of adults with serious mental illness and of the general population: research implications. Psychiatr Serv. 2013;64(8):782–8. https://doi.org/10.1176/APPI.PS.201200365.
Wilson DK, Lawman HG, Segal M, Chappell S. Neighborhood and parental supports for physical activity in minority adolescents. Am J Prev Med. 2011;41(4):399–406. https://doi.org/10.1016/J.AMEPRE.2011.06.037.
Van Dyck D, Sallis JF, Cardon G, et al. Associations of neighborhood characteristics with active park use: an observational study in two cities in the USA and Belgium. Int J Health Geogr. 2013;12:26. https://doi.org/10.1186/1476-072X-12-26.
Nelson K, Taylor L, Lurie N, Escarce J, McFarland L, Fihn SD. Neighborhood environment and health status and mortality among veterans. J Gen Intern Med. 2011;26(8):862–7. https://doi.org/10.1007/S11606-011-1710-0.
Abdel-Rahman O. Outcomes of non-metastatic colon cancer patients in relationship to socioeconomic status: an analysis of SEER census tract-level socioeconomic database. Int J Clin Oncol. 2019;24(12):1582–7. https://doi.org/10.1007/S10147-019-01497-9.
Kim T. Relationship of neighborhood and individual socioeconomic status on mortality among older adults: evidence from cross-level interaction analyses. PLoS One. 2022;17(5):e0267542. https://doi.org/10.1371/JOURNAL.PONE.0267542.
Ludwig J, Duncan GJ, Gennetian LA, et al. Neighborhood effects on the long-term well-being of low-income adults. Science. 2012;337(6101):1505–10. https://doi.org/10.1126/SCIENCE.1224648.
Shih RA, Ghosh-Dastidar B, Margolis KL, et al. Neighborhood socioeconomic status and cognitive function in women. Am J Public Health. 2011;101(9):1721–8. https://doi.org/10.2105/AJPH.2011.300169.
Kim Y, Liao Y, Colabianchi N. Examining the long-term association between neighborhood socioeconomic status and obesity and obesity-related unhealthy behaviors among children: results From the Fragile Families and Child Wellbeing Study. Ann Behav Med. 2023;57(8):640–8. https://doi.org/10.1093/ABM/KAAD001.
Gary-Webb TL, Baptiste-Roberts K, Pham L, et al. Neighborhood and weight-related health behaviors in the Look AHEAD (Action for Health in Diabetes) Study. BMC Public Health. 2010. https://doi.org/10.1186/1471-2458-10-312.
Wang X, Auchincloss AH, Barber S, et al. Neighborhood social environment as risk factors to health behavior among African Americans: The Jackson Heart Study. Health Place. 2017;45:199–207. https://doi.org/10.1016/J.HEALTHPLACE.2017.04.002.
Reitzel LR, Vidrine JI, Businelle MS, et al. Neighborhood perceptions are associated with tobacco dependence among African American smokers. Nicotine Tob Res. 2012;14(7):786–93. https://doi.org/10.1093/NTR/NTR285.
Mayhand KN, Handorf EA, Ortiz AG, et al. Effect of neighborhood and individual-level socioeconomic factors on colorectal cancer screening adherence. Int J Environ Res Public Health. 2021;18(9):4398. https://doi.org/10.3390/IJERPH18094398.
Mukhopadhyay A, Blecker S, Li X, et al. Neighborhood-level socioeconomic status and prescription fill patterns among patients with heart failure. JAMA Netw Open. 2023;6(12):e2347519. https://doi.org/10.1001/JAMANETWORKOPEN.2023.47519.
Nouri S, Lyles CR, Rubinsky AD, et al. Evaluation of neighborhood socioeconomic characteristics and advance care planning among older adults. JAMA Netw Open. 2020;3(12):e2029063. https://doi.org/10.1001/JAMANETWORKOPEN.2020.29063.
Pimentel Maldonado DA, Eusebio JR, Amezcua L, et al. The impact of socioeconomic status on mental health and health-seeking behavior across race and ethnicity in a large multiple sclerosis cohort. Mult Scler Relat Disord. 2022;58:103451. https://doi.org/10.1016/J.MSARD.2021.103451.
Warren RC, Forrow L, Hodge DA, Truog RD. Trustworthiness before trust—Covid-19 vaccine trials and the Black community. N Engl J Med. 2020;383(22):e121. https://doi.org/10.1056/NEJMP2030033.
Coaston TN, Sakowitz S, Chervu NL, et al. Persistent racial disparities in refusal of resection in non-small cell lung cancer patients at high-volume and Black-serving institutions. Surgery. 2023;174(6):1428–35. https://doi.org/10.1016/J.SURG.2023.09.006.
Jakobsen AL, Jørgensen A, Tølbøll L, Johnsen SB. Opening the black box of the relationship between neighborhood socioeconomic status and mental health: neighborhood social-interactive characteristics as contextual mechanisms. Health Place. 2022;77:102905. https://doi.org/10.1016/J.HEALTHPLACE.2022.102905.
Kansagra SM, Curtis LH, Schulman KA. Regionalization of percutaneous transluminal coronary angioplasty and implications for patient travel distance. JAMA. 2004;292(14):1717–23. https://doi.org/10.1001/JAMA.292.14.1717.
Gao TP, Green RL, Kuo LE. Disparities in access to high-volume surgeons and specialized care. Endocrinol Metab Clin N Am. 2023;52(4):689–703. https://doi.org/10.1016/J.ECL.2023.05.006.
Twardzik E, Clarke P, Elliott MR, Haley WE, Judd S, Colabianchi N. Neighborhood socioeconomic status and trajectories of physical health-related quality of life among stroke survivors. Stroke. 2019;50(11):3191–7. https://doi.org/10.1161/STROKEAHA.119.025874.
Greenberg JA, Thiesmeyer JW, Egan CE, et al. Care fragmentation in patients with differentiated thyroid cancer. World J Surg. 2022;46(12):3007–16. https://doi.org/10.1007/S00268-022-06712-9.
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002;40(IV):3–18. https://doi.org/10.1097/01.MLR.0000020942.47004.03.
Funding
This study did not receive any specific funding or sponsorship in the public, commercial, or non-profit sectors for the design and conduct of the study; collection, analysis, or interpretation of data; or preparation or review of this manuscript.
Author information
Authors and Affiliations
Contributions
KAM had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: All authors. Acquisition, analysis, and interpretation of data: KM, MSF. Drafting of the manuscript: All authors. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: KM. Obtained funding: N/A. Administrative, technical, or material support: MSF. Study supervision: All authors.
Corresponding author
Ethics declarations
Disclosure
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members. All authors contributed substantially to this work. Neither this manuscript nor one with substantially similar content under our authorship has been published or is being considered for publication elsewhere. All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Ethical Approval
This study did not involve identifiable human data or animals, and all data is publicly available, therefore, no institutional review was sought. The research was conducted in accordance with applicable laws and regulations, and the study design and methods complied with relevant STROBE guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mani, K., Kleinbart, E., Schlumprecht, A. et al. Area Socioeconomic Status is Associated with Refusal of Recommended Surgery in Patients with Metastatic Bone and Joint Disease. Ann Surg Oncol (2024). https://doi.org/10.1245/s10434-024-15299-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1245/s10434-024-15299-5