Abstract
Background
Cancer-free resection (R0) is one of the most important factors for the long-term survival of biliary carcinoma. For some patients with widespread invasive cancer located between the hilar and intrapancreatic bile duct, hepatopancreaticoduodenectomy (HPD) is considered a radical surgery for R0 resection. However, HPD is associated with high morbidity and mortality rates. Furthermore, previous reports have not shown lymph node metastasis (LNM) status, such as the location or number, which could influence the prognosis after HPD. In this study, first, we explored the prognostic factors for survival, and second, we evaluated whether the LNM status (number and location of LNM) would influence the decision on surgical indications in patients with widely spread biliary malignancy.
Methods
We retrospectively reviewed the medical records of 54 patients who underwent HPD with hepatectomy in ≥2 liver sectors from January 2003 to December 2021 (HPD-G). We also evaluated 54 unresectable perihilar cholangiocarcinoma patients who underwent chemotherapy from January 2010 to December 2021 (CTx-G).
Results
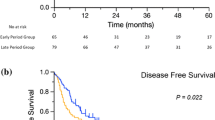
R0 resection was performed in 48 patients (89%). The median survival time (MST) and 5-year overall survival rate of the HPD-G and CTx-G groups were 36.9 months and 31.1%, and 19.6 months and 0%, respectively. Univariate and multivariate analyses showed that pathological portal vein involvement was an independent prognostic factor for survival (MST: 18.9 months). Additionally, patients with peripancreatic LNM had worse prognoses (MST: 13.3 months) than CTx-G.
Conclusions
Patients with peripancreatic LNM or PV invasion might be advised to be excluded from surgery-first indications for HPD.




Similar content being viewed by others
References
Noji T, Tanaka K, Matsui A, et al. Transhepatic direct approach to the “limit of the division of the hepatic ducts” leads to a high R0 resection rate in perihilar cholangiocarcinoma. J Gastrointest Surg. 2021;25(9):2358–67.
Ebata T, Yokoyama Y, Igami T, et al. Hepatopancreatoduodenectomy for cholangiocarcinoma: a single-center review of 85 consecutive patients. Ann Surg. 2012;256(2):297–305.
Mizuno T, Ebata T, Yokoyama Y, et al. Major hepatectomy with or without pancreatoduodenectomy for advanced gallbladder cancer. Br J Surg. 2019;106(5):626–35.
Tran TB, Dua MM, Spain DA, Visser BC, Norton JA, Poultsides GA. Hepato-pancreatectomy: how morbid? Results from the national surgical quality improvement project. HPB (Oxford). 2015;17(9):763–9.
Endo I, Hirahara N, Miyata H, et al. Mortality, morbidity, and failure to rescue in hepatopancreatoduodenectomy: an analysis of patients registered in the National Clinical Database in Japan. J Hepatobiliary Pancreat Sci. 2021;28(4):305–16.
Aoba T, Ebata T, Yokoyama Y, et al. Assessment of nodal status for perihilar cholangiocarcinoma: location, number, or ratio of involved nodes. Ann Surg. 2013;257(4):718–25.
Sakata J, Shirai Y, Wakai T, Ajioka Y, Hatakeyama K. Number of positive lymph nodes independently determines the prognosis after resection in patients with gallbladder carcinoma. Ann Surg Oncol. 2010;17(7):1831–40.
Kelly KJ, Dukleska K, Kuk D, et al. Prognostic significance of the highest peripancreatic lymph node in biliary tract adenocarcinoma. Ann Surg Oncol. 2014;21(3):979–85.
Sakata J, Wakai T, Matsuda Y, et al. Comparison of number versus ratio of positive lymph nodes in the assessment of lymph node status in extrahepatic cholangiocarcinoma. Ann Surg Oncol. 2016;23(1):225–34.
Noji T, Kondo S, Hirano S, Tanaka E, Suzuki O, Shichinohe T. Computed tomography evaluation of regional lymph node metastases in patients with biliary cancer. Br J Surg. 2008;95(1):92–6.
Seo S, Hatano E, Higashi T, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography predicts lymph node metastasis, P-glycoprotein expression, and recurrence after resection in mass-forming intrahepatic cholangiocarcinoma. Surgery. 2008;143(6):769–77.
Kushiya H, Nakamura T, Asano T, et al. Predicting the outcomes of postoperative pancreatic fistula after pancreatoduodenectomy using prophylactic drain contrast imaging. J Gastrointest Surg. 2021;25(6):1445–50.
Sakuhara Y, Abo D, Hasegawa Y, et al. Preoperative percutaneous transhepatic portal vein embolization with ethanol injection. AJR Am J Roentgenol. 2012;198(4):914–22.
Hirano S, Tanaka E, Tsuchikawa T, et al. Oncological benefit of preoperative endoscopic biliary drainage in patients with hilar cholangiocarcinoma. J Hepatobiliary Pancreat Sci. 2014;21(8):533–40.
Noji T, Inoue A, Nakanishi Y, et al. (99m)Tc-GSA scintigraphy could predict post-hepatectomy liver failure-related death in biliary surgery. J Gastrointest Surg. 2021;25(12):3236–8.
Noji T, Tsuchikawa T, Okamura K, et al. Concomitant hepatic artery resection for advanced perihilar cholangiocarcinoma: a case-control study with propensity score matching. J Hepatobiliary Pancreat Sci. 2016;23(7):442–8.
Hirano S, Tanaka E, Tsuchikawa T, Matsumoto J, Shichinohe T, Kato K. Techniques of biliary reconstruction following bile duct resection (with video). J Hepatobiliary Pancreat Sci. 2012;19(3):203–9.
Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138(1):8–13.
Koch M, Garden OJ, Padbury R, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149(5):680–8.
van Keulen AM, Buettner S, Besselink MG, et al. Primary and secondary liver failure after major liver resection for perihilar cholangiocarcinoma. Surgery. 2021;170(4):1024–30.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Deki H, Sato T. An anatomic study of the peripancreatic lymphatics. Surg Radiol Anat. 1988;10(2):121–35.
Kiriyama M, Ebata T, Aoba T, et al. Prognostic impact of lymph node metastasis in distal cholangiocarcinoma. Br J Surg. 2015;102(4):399–406.
Miura F, Sano K, Amano H, et al. Evaluation of portal vein invasion of distal cholangiocarcinoma as borderline resectability. J Hepatobiliary Pancreat Sci. 2015;22(4):294–300.
Nakanishi Y, Tsuchikawa T, Okamura K, et al. Prognostic impact of the site of portal vein invasion in patients with surgically resected perihilar cholangiocarcinoma. Surgery. 2016;159(6):1511–9.
Nagino M. Hepatopancreatoduodenectomy with simultaneous resection of the portal vein and hepatic artery: ultimate superextended surgery for advanced perihilar cholangiocarcinoma. J Hepatobiliary Pancreat Sci. Dec 22 2021.
Sugiura T, Nishio H, Nagino M, et al. Value of multidetector-row computed tomography in diagnosis of portal vein invasion by perihilar cholangiocarcinoma. World J Surg. 2008;32(7):1478–84.
Matsuyama R, Mori R, Ota Y, et al. Impact of gemcitabine plus S1 neoadjuvant chemotherapy on borderline resectable perihilar cholangiocarcinoma. Ann Surg Oncol. 2022;29(4):2393–405.
Noji T, Nagayama M, Imai K, et al. Conversion surgery for initially unresectable biliary malignancies: a multicenter retrospective cohort study. Surg Today. 2020;50(11):1409–17.
Takagi T, Yokoyama Y, Kokuryo T, Ebata T, Ando M, Nagino M. A clear difference between the outcomes after a major hepatectomy with and without an extrahepatic bile duct resection. World J Surg. 2017;41(2):508–15.
Mueller M, Breuer E, Mizuno T, et al. Perihilar cholangiocarcinoma: novel benchmark values for surgical and oncological outcomes from 24 expert centers. Ann Surg. 2021;274(5):780–8.
Fujii T, Sugimoto H, Yamada S, et al. Modified Blumgart anastomosis for pancreaticojejunostomy: technical improvement in matched historical control study. J Gastrointest Surg. 2014;18(6):1108–15.
Sugiura T, Uesaka K, Ashida R, et al. Hepatopancreatoduodenectomy with delayed division of the pancreatic parenchyma. Ann Surg Open. 2021;2(4).
Watanabe N, Mizuno T, Yamaguchi J, et al. A proposal of drain removal criteria in hepatobiliary resection. J Hepatobiliary Pancreat Sci. 2022.
Nimura Y. Preoperative biliary drainage before resection for cholangiocarcinoma (Pro). HPB (Oxford). 2008;10(2):130–3.
Moole H, Bechtold M, Puli SR. Efficacy of preoperative biliary drainage in malignant obstructive jaundice: a meta-analysis and systematic review. World J Surg Oncol. 2016;14(1):182.
Higuchi R, Yazawa T, Uemura S, et al. ENBD is associated with decreased tumor dissemination compared to PTBD in perihilar cholangiocarcinoma. J Gastrointest Surg. 2017;21(9):1506–14.
Parks RW, Clements WD, Smye MG, Pope C, Rowlands BJ, Diamond T. Intestinal barrier dysfunction in clinical and experimental obstructive jaundice and its reversal by internal biliary drainage. Br J Surg. 1996;83(10):1345–9.
Welsh FK, Ramsden CW, MacLennan K, et al. Increased intestinal permeability and altered mucosal immunity in cholestatic jaundice. Ann Surg. 1998;227(2):205–12.
Nagino M, Hirano S, Yoshitomi H, et al. Clinical practice guidelines for the management of biliary tract cancers 2019: the 3rd English edn. J Hepatobiliary Pancreat Sci. 2021;28(1):26–54.
Takahashi Y, Sasahira N, Sasaki T, et al. The role of stent placement above the papilla (inside-stent) as a bridging therapy for perihilar biliary malignancy: an initial experience. Surg Today. 2021;51(11):1795–804.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors have no financial interests or potential conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoshimi, Y., Noji, T., Okamura, K. et al. The Short- and Long-Term Surgical Results of Consecutive Hepatopancreaticoduodenectomy for Wide-Spread Biliary Malignancy. Ann Surg Oncol 31, 90–96 (2024). https://doi.org/10.1245/s10434-023-14406-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14406-2