Abstract
Introduction
After extensive small and colon resections, quality of life can be affected. We propose the antiperistaltic transverse coloplasty as a solution that allows for preservation of the transverse colon after both right and left colectomies while achieving a tension-free colorectal anastomosis slowing the transit and increasing the absorption time, resulting in better stool consistency and quality of life compared with an ileorectal anastomosis.
Methods
This technique was performed in a 41-year-old woman with Goblet cell adenocarcinoma of the appendix with peritoneal metastasis. The transverse colon is rotated anticlockwise over the axis of the middle colic vessels toward the left parietocolic flank and relocated to the usual position of the descending colon.
Results
After 1 year of follow-up, the patient led a normal life without parenteral nutrition with five bowel movements per day and a weight gain of 15%.
Conclusions
The use of an antiperistaltic transverse coloplasty may be worthwhile to perform in cases of extensive bowel resections during cytoreductive surgery leading to short-bowel syndrome to avoid a permanent stoma or intestinal failure and improve patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Due to the loss of colonic reabsorption and/or rectal reservoir function, extensive colorectal resections may have poor outcomes, especially when accompanied by short-bowel syndrome. Although reabsorption has been partially preserved in some indications by preserving the cecum and performing a cecorectal anastomosis, colonic and ileal pouches have been proposed to maintain some reservoir function. In cases of carcinomatosis, in addition to extensive colorectal resections, extensive small-bowel resections also are performed; frequently the cecum cannot be preserved. In these cases, antiperistaltic transverse coloplasty can be interposed between the ileum and the rectal stump. Although challenging, this reconstruction can increase reabsorption and improve quality of life.
As far as we know, this kind of reconstruction has not been the subject of any reports in the literature. We describe an antiperistaltic transverse coloplasty technique used during cytoreductive surgery and HIPEC to improve reabsorption and quality of life following extended small-bowel resection and right and left colectomies.
Technique
We conducted this technique in a 41-year-old female after performing resection of small bowel with a remaining small bowel of 1.8 meters, both right and left colectomies, hysterectomy, double adnexectomy, rectal anterior resection and central lymphadenectomy due to Goblet cell adenocarcinoma of the appendix with peritoneal metastasis.
The creation of a tension-free anastomosis after both left and right colectomies can be challenging and requires expertise and anatomical knowledge.1 To avoid tension between the remaining bowel ends, many surgeons would elect to perform a total colectomy. However, this results in deterioration of intestinal function with frequent bowel movements that persist in the long term and have an adverse effect on quality of life.2
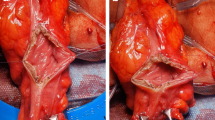
In our case, after the resection was concluded, intestinal transit was restored by performing an antiperistaltic transverse coloplasty before the HIPEC procedure. To perform this technique, middle colic vessels and their distal branches need to be preserved (Fig. 1). After assessing its correct vascularization, transverse colon is rotated anticlockwise over the axis of the middle colic vessels toward the left parietocolic flank. After that, the splenic flexure should remain in its position while the hepatic flexure reaches the middle rectum, and all of the transverse colon gets relocated to the usual position of the descending colon (Fig. 2). In this position, the posterior, mesocolic layer is transferred to an anterior position (Video 1). An anastomosis is then performed between the remnant small bowel and the splenic flexure of the colon. A colorectal anastomosis is constructed between the hepatic flexure of the colon and the rectum, with the colon in an antiperistaltic position.
Results
The patient exhibited a favorable postoperative course during 1-year, follow-up period. Despite possessing a 1.8-meter remnant of small intestine without an ileocecal valve, implementation of a low-fiber diet, low-oxalate diet, and oral supplementation with fiber-free oligomeric hyperprotein hypercaloric formula (Survimed®) resulted in the patient attaining a fully normalized lifestyle with five daily bowel movements and a weight gain of 15%.
Discussion
Short-bowel syndrome (SBS) causes structural changes in the intestine, which interfere with its main functions of digestion and absorption due to reduced surface area. The inadequate length of the small intestine increases the risk of developing intestinal insufficiency or failure in patients with SBS, which depends on the degree of malabsorption.3 After extensive intestinal resection, a compensatory adaptation of the residual intestine occurs physiologically, both at a structural and functional level, in order to enhance nutrient absorption and delay gastrointestinal transit.4
The length of the remaining small bowel is crucial for postsurgical outcomes, but the colon can be safely removed if the small bowel is intact. Therefore, the preservation of the colon is not a primary concern for surgeons.5 However, new studies indicate that, in the case of restoration of jejune-colonic anastomosis, the colon plays an important role in reducing the need for parenteral support, ultimately improving survival and quality of life. This highlights the significance of the colon alongside the small bowel in postsurgical outcomes.1,2,3
By performing this technique, at least 28% of the colon is salvaged according to Cummings classification and make it equivalent to a type 2 SBS.6 These patients also are referred to as SBS with a colon-in-continuity (SBS-CiC).5 Type 2 patients having the majority of the colon but no ileocecal valve can avoid parenteral nutrition with a minimum of 65 cm of remaining small bowel.4,7 With the preservation of colon-in-continuity, intravenous supplementation is unnecessary. SBS-CiC can offset malabsorption by increasing oral food intake or using pharmacotherapeutics, thereby avoiding intestinal failure.5
Furthermore, patients with extensive intestinal resections are at risk of bacterial overgrowth of the small intestine, worse absorption of water and sodium, and malabsorption due to fast transit and reduced absorption surface area.5 This results in a lower quality of life and worse stool consistency.2
Good intestinal function may also be preserved by salvaging any large intestine segments when extensive colon resection is added. Because the proximal segment also may serve as a reservoir in place of an ileal pouch, the shorter the rectal remnant, the more prudent the preservation, it stands to reason.8
Antiperistaltic transverse coloplasty allows for preservation of the transverse colon while achieving a tension-free colorectal anastomosis. The antiperistaltic placement of the colon slows the transit while increasing the absorption time, which might result in a retarded transit, increased intestinal absorption, better consistency of the stool, and quality of life compared with an ileorectal or jejunorectal anastomosis while avoiding intestinal failure.6,9
This technique enables us to concentrate on improving the quality of the remaining life in young patients with poor life expectancy after extensive cytoreductive surgery rather than having to perform a permanent ileostomy.8
Conclusions
To avoid a permanent stoma or intestinal failure after cytoreductive surgery, an antiperistaltic transverse coloplasty may be worthwhile to perform whenever possible. An oncologic surgeon should be adept at this technique, because it might be the only workable solution for the saved segment.
References
Amiot A, Messing B, Corcos O, Panis Y, Joly F. Determinants of home parenteral nutrition dependence and survival of 268 patients with non-malignant short bowel syndrome. Clin Nutr. 2013;32:368–74.
Crenn P, Morin MC, Joly F, Penven S, Thuillier F, Messing B. Net digestive absorption and adaptive hyperphagia in adult short bowel patients. Gut. 2004;53:1279–86.
Billiauws L, Thomas M, Le Beyec-Le Bihan J, Joly F. Intestinal adaptation in short bowel syndrome. What is new? Nutr Hosp. 2018;35:731–7.
Gonzalez-Argenté FX, Segura‐Sampedro JJ. Isquemia vascular intestinal . Síndrome de intestino corto. In: Cirugía AEC. Editorial Médica Panamericana: Madrid, 2022.
Verbiest A, Jeppesen PB, Joly F, Vanuytsel T. The role of a colon-in-continuity in short-bowel syndrome. Nutrients. 2023;15:628.
Sidhu GS, Narasimharao KL, Rani VU, Sarkar AK, Mitra SK. Absorption studies after massive small bowel resection and antiperistaltic colon interposition in rhesus monkeys. Dig Dis Sci. 1985;30:483–8.
Billiauws L, Maggiori L, Joly F, Panis Y. Medical and surgical management of short bowel syndrome. J Visc Surg. 2018;155:283–91.
Violi V, Costi R, Marchesi F, Cecchini S, Sarli L, Roncoroni L. Anti-peristaltic ileocolonproctoplasty: A salvage procedure in extensive resective colorectal surgery. Int J Colorectal Dis. 2007;22:1277–81.
Yagi T, Nakagawa K, Sadamori H, Hashimoto M, Kamikawa Y, Tanaka N. Antiperistaltic transverse colostomy for massive bowel necrosis following surgery for an abdominal aortic aneurysm: Report of a case. Surg Today. 1997;27:554–8.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. We declare that there is no funding to report for this research.
Author information
Authors and Affiliations
Contributions
JJS, RM, and CP performed the surgery and followed up with the patient. AC, and JJS conducted the literature search. JJS and AC wrote the manuscript. JJS, and JCR made substantial revisions to the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Disclosure
The authors declare that there is no conflict of interest.
Ethical approval
Our patient signed informed consent to allow the publication of this case.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 10692 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Segura-Sampedro, J.J., Morales-Soriano, R., Rodríguez-Pino, J.C. et al. Antiperistaltic Transverse Coloplasty: A Salvage Procedure in Extensive Bowel and Colorectal Resections to Avoid Intestinal Failure. Ann Surg Oncol 30, 7236–7239 (2023). https://doi.org/10.1245/s10434-023-14165-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14165-0