Abstract
Background
There is no definitive answer regarding the efficacy of intraoperative radiotherapy (IORT) as a tumour bed boost for patients with early-stage breast cancer. The purpose of this meta-analysis was to summarise the available evidence and explore the efficacy and safety of IORT combined with whole breast irradiation (WBI) versus conventional radiotherapy in women with early-stage breast cancer who underwent breast-conserving surgery.
Methods
The PUBMED, MEDLINE, EMBASE, Web of Science, and Cochrane Library databases were searched from inception to December 31, 2022. We collected studies on the efficacy, cosmetic outcome, and safety of IORT boost combined with WBI compared with those of conventional radiotherapy in patients with early-stage breast cancer after breast-conserving surgery. Two authors independently performed the literature selection and data extraction. The quality of the randomised, controlled trials (RCTs) was assessed according to the PEDro scale. The quality of non-RCTs was assessed according to the Methodological Index for Non-Randomised Studies. Risk ratios (RRs) for the local recurrence rate (LRR), distant metastasis rate (DMR), disease-free survival (DFS), cosmetic outcome, and toxicity were pooled using fixed or random effects models. Meta-analysis of the included studies was performed by using RevMan 5.3 software.
Results
Nine studies, including one RCT and eight non-RCTs, with a total of 3219 patients were included. In terms of LRR, there was no significant benefit of IORT boost+WBI over conventional radiotherapy (with or without the tumour bed boost) (RR = 0.77, 95% confidence interval (CI): 0.54–1.09, P = 0.14), but a trend towards benefit could be identified. There was a significant reduction in DMR in the IORT boost+WBI group (RR = 0.63, 95% CI: 0.46–0.85, P = 0.003) and a significant improvement in DFS (RR = 0.40, 95% CI: 0.25–0.65, P = 0.0002). Exploratory subgroup analysis showed that the DMR and DFS of the electron boost group were significantly better than those of conventional radiotherapy group, and there was a tendency for LRR to improve in the electron boost group. However, the LRR, DMR, and DFS did not effectively improve in the x-ray boost group. In terms of appearance and toxicity, there were no significant differences in cosmetic outcome, fibrosis, and hyperpigmentation between the two groups (RR = 0.99, 95% CI: 0.91–1.07, P = 0.78; RR = 1.02, 95% CI: 0.41–2.56, P = 0.96; RR = 0.42, 95% CI: 0.10–1.72, P = 0.23), but the incidence of oedema was significantly reduced in the IORT boost+WBI group (RR = 0.27, 95% CI: 0.13–0.59, P = 0.0009).
Conclusions
IORT boost+WBI is more effective than conventional radiotherapy after breast-conserving surgery in patients with early-stage breast cancer, and electron boost exhibits better efficacy than x-ray boost. In addition, the cosmetic and safety profiles of IORT boost+WBI are not inferior to those of conventional radiotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The 2020 global cancer data show that the incidence of breast cancer has surpassed that of lung cancer, making breast cancer the most common cancer worldwide.1 Breast-conserving surgery is now the internationally accepted treatment of choice for early-stage breast cancer. Studies have shown that the addition of radiation therapy after breast-conserving surgery for early-stage breast cancer can further improve local control rates and reduce the risk of local recurrence after surgery.2,3 Therefore, breast-conserving surgery combined with external beam radiotherapy (EBRT) is considered the “gold standard” treatment for early-stage breast cancer.4,5 The EBCTCG meta-analysis demonstrated that breast-conserving surgery combined with external radiotherapy was effective in reducing the local recurrence rate of breast cancer, but approximately 19.3% of patients still experienced recurrence within 10 years.6 It has been found that 80% to 90% of local recurrences after breast-conserving treatment occur in the tumour bed or its surrounding areas.7,8,9 At present, it is unadvisable to blindly extend the excision of breast tissue around the tumour to reduce the local recurrence rate, as this would severely damage the appearance of the breast and defeat the key significance of breast conservation. Therefore, it is important to find a new radiotherapy method to enhance local tumour control while ensuring complete excision of the tumour.
Conventional radiotherapy after breast-conserving surgery is administered in the form of conventional segmentation (45–50 Gy at 1.8–2.0 Gy/dose, once per day, five times per week, with or without a tumour bed boost of 10.0–16.0 Gy), but the current conventional form of external irradiation has been challenged by the continuous advances in breast cancer research. Studies have shown that conventional radiotherapy has the disadvantages of poor compliance, long intervals, and inaccurate tumour bed localisation.10,11,12 Therefore, it is necessary to adopt new radiotherapy methods to further improve the local tumour control rate after breast-conserving surgery for early-stage breast cancer.
In recent years, an increasing number of breast cancer centres have introduced intraoperative radiotherapy (IORT) into breast-conserving treatments and have investigated its indications, modalities, doses, efficacy, and prognosis. There are currently two techniques of IORT: electron intraoperative therapy (ELIOT) using a linear electron accelerator, and targeted intraoperative radiotherapy (TARGIT) using the INTRABEAM system with 50 kV low energy x-rays.13,14 The idea behind IORT in breast-conserving surgery is to deliver a high, single dose in the most precise way to the areas with the highest risk of subclinical, tumour cell contamination through direct visualisation. The dose of IORT is usually 8–21 Gy, which has the advantages of shortening the treatment course, precisely locating the target area, and improving the radiobiological effect on the tumour, thus compensating for the shortcomings of conventional radiotherapy.
There are two main treatment modalities for IORT; the first is the more radical modality of simply replacing all postoperative, external radiotherapy with a single, high-dose, intraoperative, local irradiation. The second is the more conservative modality of retaining postoperative whole breast irradiation (WBI) and replacing external tumour bed boost with a single, high-dose, intraoperative, local irradiation. Representative studies of a single IORT as a substitute for all postoperative, external radiotherapy include the ELIOT and TARGIT-A trials. More recently, the ELIOT trial published updated results with a median follow-up of 12.4 years, demonstrating a significant 10.2% increase in the 15-year IBTR rate in the single IORT group compared with the external irradiation radiotherapy group.15,16 Similarly, preliminary results from TARGIT-A trial showed that the local control rate of IORT alone after breast-conserving surgery was noninferior to that of postoperative external radiotherapy in patients aged ≥45 years with early-stage breast cancer; however, the 5-year local recurrence rate was significantly higher in the IORT group than in the external, radiotherapy group.17,18 Therefore, the effectiveness of IORT alone remains controversial.
Although IORT can compensate for the shortcomings of conventional radiotherapy to a certain extent, there are limitations to IORT: for example, small area of irradiation, small total dose, short duration, and insufficient evidence. Therefore, optimising and combining IORT with conventional external radiotherapy has become a major challenge in the treatment of early breast cancer after breast-conserving surgery. To address this challenge, some studies have explored the combination of IORT and conventional external radiation radiotherapy, demonstrating that IORT as a tumour bed boost (IORT boost) combined with postoperative WBI is not inferior to postoperative WBI combined with external radiation tumour bed boost (EBRT boost) in terms of local tumour control rate.19,20,21,22,23,24,25,26,27,28 This new radiotherapy modality combines the advantages of IORT with conventional radiotherapy, which can reduce the duration of radiotherapy to a certain degree. To date, no corresponding meta-analyses have sufficiently investigated this novel modality. Thus, we conducted this meta-analysis to evaluate the efficacy, cosmetic results, and safety of IORT as a tumour bed boost combined with WBI compared with traditional radiotherapy in women with early-stage breast cancer and breast-conserving surgery.
Materials and Methods
Literature Search
We searched in PUBMED, MEDLINE, EMBASE, Web of Science, and Cochrane Library by using the following phrases: “breast cancer”; “intraoperative radiotherapy”; “IORT”; and “boost.” Medical subject headings and free terminology were used for each electronic search. There were no language-based restrictions. The search period was from the establishment of the database until December 31, 2022. References of the included studies also were reviewed to identify potentially eligible articles. Two reviewers (JH and SC) independently conducted literature searches. The detailed searching strategy was listed in the Supplemental Data 1.
Study Selection
This meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) 2020 statement.29 Studies that assessed the efficacy, cosmetic outcome, and safety of IORT boost combined with postoperative WBI and compared the findings with those of conventional radiotherapy (with or without tumour bed boost) after breast-conserving surgery in patients with early-stage breast cancer were included. The eligibility criteria are listed below.
Population
-
Women with early-stage breast cancer who underwent breast-conserving treatment, including those with stage T1-2N0-3M0;
-
Experimental group: IORT boost combined with postoperative WBI;
-
Control group: Conventional external beam radiotherapy (EBRT), including WBI using external irradiation with or without tumour bed boost;
-
Outcomes: Local recurrence rates (LRRs), survival outcomes, cosmetic outcomes, and toxicity;
-
Study design: Randomised, clinical trials (RCTs) and other comparative studies with control groups.
The following studies were excluded: studies using single IORT as an alternative to whole breast external radiation radiotherapy; studies with duplicate data or full text not available or no available data; single-arm studies; and reviews. For multiple publications of the same study, publications with the most recent data and applicable information were used.
Data Extraction and Quality Assessment
Two authors (LY and YS) independently performed data extraction and quality assessment. Disagreements were resolved through consensus. Data extracted from each study were as follows: first author, date of publication, study design, study group, study sample size, study intervention, patient characteristics, median follow-up time, and outcomes. Outcomes included local recurrence and distant metastasis rates, disease-free survival (DFS), cosmetic outcomes, and toxicity. The quality of the RCTs was assessed according to the PEDro scale, with a maximum score of 11.30,31 The quality of non-RCTs was evaluated according to the Methodological Index of Non-randomised Studies (MINORS), with a maximum score of 24.32
Statistical Analysis
Statistical analyses were performed by using RenMan 5.3 software. The incidence of the outcome indicators analysed in the included studies were all low. Risk ratios (RRs) and 95% confidence intervals (CIs) were used as effect indicators for local recurrence rate, distant metastasis rate, DFS, cosmetic outcome, and toxicity. Statistical heterogeneity between the results of the included studies was analysed by using a Q-test (test level set at α = 0.10). The results were analysed by using a fixed-effects model if the heterogeneity was small (I2 < 50%), otherwise a random-effects model or descriptive analysis was used. A Z-test was used to test the significance of the pooled RRs (considered significant at p < 0.05). The results of the tests are presented in a forest plot. In addition, we performed sensitivity analyses by excluding studies individually to test the stability of the results of our meta-analysis. Finally, funnel plots were used to determine whether there was publication bias for the main outcome indicators.
Results
Study Selection
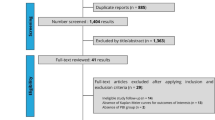
We identified 2898 records. After excluding duplicate records, we retrieved 2350 articles, which were further filtered by screening titles and abstracts. Of these articles, 2337 were excluded for the following reasons: use of intraoperative IORT as an exclusive alternative to total external breast irradiation radiotherapy; lack of a control group in the study; or no available results, reviews, or comments. Finally, through further full-text reading and screening, a total of nine studies met our eligibility criteria and were selected for final analysis.19,20,21,22,23,24,25,26,27 The study selection process is illustrated in Fig. 1.
Study Characteristics and Quality Assessment
The nine included studies comprised one RCT and eight non-RCTs, with a total of 3219 patients. Of these, 1832 patients were in the IORT group and 1387 patients in the EBRT group. The baseline characteristics of each study were balanced between the two groups. Most of the studies began in 2000 or later and were published between 2006 and 2021. The sample sizes ranged from 46 to 1646 cases. Except for the Fastner and Hashemi studies, the mean or median age of the enrolled patients was 50 years or older. The tumour size was inconsistent in each study but was generally less than 3 cm. The follow-up time also was inconsistent in each study; the shortest follow-up time was only 4–6 months, and the longest median follow-up time was up to 12 years. Overall, the methodological quality of the nine included studies was acceptable. One RCT had a score of 8 on the PEDro scale19; the scores were lost because the patients and investigators were not blinded. Six prospective cohort studies had MINORS scores of 19–2022,23,24,25,26,27 whereas the other two, retrospective, case-control studies had MINORS scores of 18.20,21 Table 1 presents the quality assessment of the nonrandomized studies included in this meta-analysis. We considered that all studies have a low risk of bias. The main characteristics and quality assessment results of the nine included studies are presented in Table 2.
Meta-analysis Results and Sensitivity Analysis
Local Recurrence Rate
Local recurrence included ipsilateral intramammary, cutaneous, and chest wall recurrence. Eight of the nine included studies reported RRs for local recurrence rates (LRR) data (one RCT and seven non-RCTs, with a total of 3082 patients).19,20,21,22,23,24,26,27 Because of the small heterogeneity (I2 = 36%, P = 0.15), a fixed-effects model was used for meta-analysis. The pooled RR for LRR showed no statistically significant difference between the IORT boost+WBI group and the conventional radiotherapy group (RR = 0.77, 95% CI: 0.54–1.09, P = 0.14), but LRR in the IORT boost+WBI group showed a trend towards improvement. In subgroup analysis, compared with the EBRT boost+WBI group, LRR in the IORT boost+WBI group also tended to improve, but there was still no statistically significant difference between the two groups (RR = 0.74, 95% CI: 0.52–1.07, P = 0.11; Fig. 2a). We performed sensitivity analyses by excluding these studies individually and found that the heterogeneity in LRR was mainly derived from the article by Reitsamer (2006). When we excluded this article, no significant heterogeneity was found between the remaining seven studies (I2 = 0%, P = 0.52), and there was no statistically significant change in the effect values for recombination (RR = 0.95, 95% CI: 0.65–1.38, P = 0.77).
Distant Metastases Rate
Similarly, all eight studies that provided LRR data also provided RRs for distant metastasis rate (DMR) with low heterogeneity (I2 = 25%, P = 0.24), so the same fixed-effects model was used for meta-analysis.19,20,21,22,23,24,26,27 The pooled RR showed that DMR was significantly lower in the IORT boost+WBI group than in the conventional radiotherapy group (RR = 0.63, 95% CI: 0.46–0.85, P = 0.003). Furthermore, a subgroup analysis showed that the DMR in the IORT boost+WBI group also was significantly lower than the DMR in the EBRT boost+WBI group (RR = 0.58, 95% CI: 0.42–0.79, P = 0.0006; Fig. 2b). Sensitivity analysis revealed that the heterogeneity in DMR mainly originated from the article by Sperk (2012). When we excluded this article, no significant heterogeneity was found between the remaining seven studies (I2 = 0%, P = 0.42), and no statistically significant change in effect values was observed for the recombination (RR = 0.58, 95% CI: 0.42–0.79, P = 0.0006).
Disease-Free Survival
Disease-free survival (DFS) was defined as the proportion of patients who did not experience any recurrence. Six studies provided data on DFS, but only four non-RCTs provided RRs for DFS data (647 patients in total).20,21,22,24 The other two studies provided 5- or 10-year cumulative survival rates only.19,27 The heterogeneity of DFS was small (I2 = 20%, P = 0.29); therefore, the fixed effects model was used for meta-analysis. The pooled RR showed that DFS was significantly better in the IORT boost+WBI group than in the conventional radiotherapy group (RR = 0.40, 95% CI: 0.25–0.65, P = 0.0002). In a subgroup analysis, it was concluded that DFS also was significantly better in the IORT boost+WBI group than in the EBRT boost+WBI group (RR = 0.40, 95% CI: 0.25–0.65, P = 0.0002; Fig. 2c). Sensitivity analysis showed that the heterogeneity in DFS mainly originated from the article by Reitsamer (2006). When we excluded this article, no significant heterogeneity was found between the remaining seven studies (I2 = 0%, P = 0.75). There was, however, a statistically significant change in the effect values for the recombination (RR = 0.57, 95% CI: 0.31–1.06, P = 0.08). However, considering that the article by Reitsamer (2006) fully met the inclusion criteria, the quality of the article was well assessed, and the overall heterogeneity was low, we still included this article in the pooled analysis of DFS.
Cosmetic Outcome
Two studies provided RRs for cosmetic outcomes (one RCT and one non-RCT; 366 patients in total).19,25 The heterogeneity of cosmetic outcomes was small (I2 = 15%, P = 0.28); therefore, the fixed-effects model was used for meta-analysis. The pooled RR for cosmetic outcome showed no significant difference between the IORT boost+WBI group and the conventional radiotherapy group (RR = 0.99, 95% CI: 0.91–1.07, P = 0.78; Fig. 3a).
Fibrosis
Three studies provided RRs for fibrosis (479 patients in total).24,25,26 The heterogeneity was greater for fibrosis (I2 = 65%, P = 0.06); therefore, a random-effects model was used for meta-analysis. The pooled RR showed no significant difference between the IORT boost+WBI group and the conventional radiotherapy group (RR = 1.02, 95% CI: 0.41–2.56, P = 0.96; Fig. 3b). Sensitivity analysis revealed that the heterogeneity of fibrosis mainly originated from the article by Welzel (2010). When we excluded this article, we found that the heterogeneity could be significantly reduced (I2 = 13%, P = 0.28) and that there was no statistically significant change in the effect values for the recombination (RR = 0.67, 95% CI: 0.39–1.17, P = 0.16).
Oedema
All three studies that provided fibrosis data also provided RRs for oedema with no significant heterogeneity (I2 = 0%, P = 0.51).24,25,26 Thus, a fixed-effects model was used for meta-analysis. The pooled RR indicated that the incidence of oedema was significantly lower in the IORT boost+WBI group than in the conventional radiotherapy group (RR = 0.27, 95% CI: 0.13–0.59, P = 0.0009; Fig. 3c).
Hyperpigmentation
Two studies provided RRs for hyperpigmentation (176 patients in total).24,25 The heterogeneity of hyperpigmentation was small (I2 = 29%, P = 0.24); therefore, a fixed-effects model was used for meta-analysis. The pooled RR showed no significant difference between the IORT boost+WBI group and the conventional radiotherapy group (RR = 0.42, 95% CI: 0.10-1.72, P = 0.23; Fig. 3d).
Subgroup Analysis
We performed a subgroup analysis to explore whether the LRR, DMR, and DFS differed between electron boost+WBI and x-ray boost+WBI groups compared with the corresponding outcomes of conventional radiotherapy. The pooled RRs for LRR showed no statistically significant difference between the two different boosts + WBI compared with conventional radiotherapy respectively (RR = 0.74, 95% CI: 0.34–1.62, P = 0.45; RR = 1.00, 95% CI: 0.50–2.04, P = 0.99), but LRR in the electron boost+WBI group showed a trend towards improvement. Electron boost+WBI group had significantly better DMR and DFS than did the conventional radiotherapy group (RR = 0.50, 95% CI: 0.35–0.72, P = 0.0001; RR = 0.41, 95% CI: 0.17–0.96, P = 0.04). However, the x-ray boost+WBI group did not effectively improve the DMR and DFS (RR = 1.13, 95% CI: 0.71–1.78, P = 0.61; RR = 0.53, 95% CI: 0.22–1.24, P = 0.14; Fig. 4a, b, c).
Assessment of Publication Bias
Our study assessed publication bias in eight articles for local recurrence and distant metastasis rates due to the variable number of included studies for each outcome indicator.19,20,21,22,23,24,26,27 Funnel plots for the two evaluation indicators both showed a more symmetrical left-right pattern, suggesting a low likelihood of publication bias (Fig. 5a, b). Few articles were included for all other outcome indicators; therefore, publication bias was not assessed.
Discussion
Many single-arm studies have demonstrated the efficacy and safety of IORT boost+WBI;33,34,35,36,37,38,39,40,41,42,43 however, comparative studies on IORT boost+WBI and conventional radiotherapy are still lacking. Through a search of major databases, we screened nine comparative studies of IORT boost+WBI versus conventional radiotherapy, with varying results. In this meta-analysis of nine studies with a total of 3219 patients, the pooled results showed that among women with early-stage breast cancer who underwent breast-conserving surgery, those who received IORT boost+WBI had significantly better DMR and DFS than those who received conventional radiotherapy (with or without the tumour bed boost) (RR = 0.63, 95% CI: 0.46–0.85, P = 0.003; RR = 0.40, 95% CI: 0.25–0.65, P = 0.0002). Although LRR was not significantly different between the two groups, the IORT boost+WBI group showed a trend towards benefit (RR = 0.77, 95% CI: 0.54–1.09, P = 0.14).
In this meta-analysis, we did not find significantly better LRR in the IORT boost+WBI group than in the conventional radiotherapy group, which may be related to the generally short follow-up period of the included studies (3–5 years in most studies). Moreover, all the studies had different inclusion criteria and included different proportions of various subtypes of breast cancer, leading to a bias in the risk of recurrence, and the studies were conducted in different contexts. This indicates some variations in systemic treatment, which may affect the final outcome. However, it is undeniable that the patients included in these studies were generally at low risk of recurrence and had small tumour sizes; therefore, the LRRs in these patients were low even with conventional radiotherapy, making it difficult to achieve a statistically significant advantage in the experimental group and highlighting the need for larger sample sizes and a longer follow-up period.
As shown in Table 2, our meta-analysis included patients with low- to high-risk, early-stage breast cancer staged as T1-2N0-3M0. From Fig. 2a, we observed that IORT boost+WBI tended to be have a more beneficial effect on LRR than did conventional radiotherapy. In addition, a large multicentre, prospective, randomised, clinical study for breast cancer patients with a high risk of recurrence is currently ongoing: the TARGIT-B trial. The inclusion criteria for the TARGIT-B trial are poor characteristics, such as age younger than 46 years, invasive lobular carcinoma, neoadjuvant chemotherapy, and age older than 45 years with grade 3 or ER/PR-negative or lymph node positive. Its primary outcome is local tumour control, with secondary outcomes, including the site of breast recurrence, survival, toxicities, and quality of life. We look forward to the final results of the study. Nonetheless, there is still a lack of relevant, prospective, randomised, clinical studies for those low-risk patients who are not eligible for the TARGIT-B trial.
In our meta-analysis, we were surprised to observe that both DMR and DFS were significantly better in the IORT boost+WBI group than in the conventional radiotherapy group. This result is perhaps more meaningful than that of LRR. This is because it is well known that a large proportion of deaths in breast cancer patients are due to distant metastases, leading to dysfunction of the involved vital organs and, ultimately, death. Only a small proportion of nonbreast–cancer-specific deaths are due to the exacerbation of the patient’s own underlying disease. Therefore, the benefit of DMR and DFS in the IORT boost+WBI group gives us hope for prolonged overall survival (OS) or breast cancer-specific OS. As known, conventional radiotherapy is used to inhibit the growth and reproduction of tumour cells by directly damaging their DNA structure through radiation irradiation. However, IORT differs from conventional radiotherapy in terms of the operating method and treatment dose. After a single high dose of irradiation to local tissues, the DNA structure of tumour cells is destroyed, but the surrounding ductal epithelial cells, adipocytes, or vascular endothelial cells also may be damaged to varying degrees. The inflammatory response of local tissues, fibrosis, and impaired microcirculation are factors that affect distant tumour metastasis and are perhaps the most important mechanisms of IORT. However, no study has specifically investigated the mechanisms of IORT, probably because current clinical trials of IORT have not shown satisfactory results. We hope to see the benefits of IORT in terms of OS for patients in future, high-quality, clinical studies.
Notably, four of the five studies that provided OS data showed no benefit in OS or breast cancer-specific OS in the IORT boost+WBI group. The 3-year OS in the IORT boost+WBI group in the Sperk 2012 was 93% compared with 100% in the conventional radiotherapy group. After a median follow-up of 5 years in the Fastner (2014) study, the 6-year OS was 86.4% in the IORT boost+WBI group and 92% in the WBI+EBRT boost group, with no statistical difference between the two groups. In Ciabattoni (2021), after a median follow-up of 12 years, the 5-year and 10-year OS in the IORT boost+WBI group were 94.5% and 91.6%, respectively, compared with 99% and 94.3% in the WBI+EBRT boost group, with no statistical difference between the two groups (P = 0.377). Hashemi (2021) yielded a 5-year OS of 95.1%, 97.5%, and 97.2% for the EBRT, electron boost, and x-ray boost groups, respectively. In terms of OS, no statistically significant differences were found among the three groups. However, a study by Kolberg (2017) concluded that the IORT boost+WBI group showed a significantly better 5-year OS (96.7% vs. 81.7%, HR = 0.19, 95% CI: 0.04-0.87, P = 0.016) and nonbreast–cancer-specific OS (100% vs. 89.9%, P = 0.015) than the conventional radiotherapy group did but showed no significant improvement in breast–cancer-specific OS (96.7% vs. 90.9%, HR = 0.42, 95% CI: 0.08-2.30, P = 0.30). It is well known that the two peaks of recurrence in breast cancer are 1–3 years after surgery and 7–8 years after surgery. For patients with a lower risk of recurrence, we need a longer follow-up period to observe recurrence. For these studies, a short follow-up period is probably the most important reason for the reported effects on LRR, OS, and breast–cancer-specific OS. Therefore, these studies need a longer follow-up period to further observe the differences in recurrence rates and survival between the two groups.
As mentioned previously, IORT consists of two main systems: a portable, electron-accelerator ELIOT system, and a photon-therapy INTRABEAM system. In our meta-analysis, the ELIOT system alone was used in four studies, the INTRABEAM system alone was used in four studies, and both systems were used in one study. Surprisingly, Hashemi (2021) concluded that 5-year DFS was 89.5%, 92.3%, and 91.3% for the x-ray boost, electron boost, and EBRT groups, respectively.27 There was no significant difference in 5-year DFS between EBRT and x-ray boost groups (P = 0.36) and between EBRT and electron boost groups (P = 0.26). Nevertheless, there was a significant difference between the x-ray boost and electron boost groups (P = 0.037), with a better DFS in the electron boost group. Therefore, we performed a subgroup analysis to explore whether the LRR, DMR, and DFS differed between electron boost+WBI and x-ray boost+WBI groups compared with the corresponding outcomes of conventional radiotherapy. As a result, we found that the electron boost+WBI group had significantly better DMR and DFS than did the conventional radiotherapy group, and that there was a trend towards a benefit in LRR in the electron boost+WBI group. However, the x-ray boost+WBI group did not effectively improve the LRR, DMR, and DFS. Undoubtedly, these results are premature, and more multicentre, prospective, randomised, clinical studies are needed to explore the differences in the efficacy and safety of electron boost compared to x-ray boost, as well as basic research to explore the mechanistic differences between the two.
In terms of appearance and toxicity, our meta-analysis yielded no significant differences in cosmetic outcome, fibrosis, and hyperpigmentation between the two groups (RR = 0.99, 95% CI: 0.91–1.07, P = 0.78; RR = 1.02, 95% CI: 0.41–2.56, P = 0.96; RR = 0.42, 95% CI: 0.10–1.72, P = 0.23), but the incidence of oedema was significantly reduced in the IORT boost+WBI group (RR = 0.27, 95% CI: 0.13-0.59, P = 0.0009). However, the results should be interpreted with caution due to the small number of studies providing cosmetic outcomes and toxicity as well as mild-to-moderate heterogeneity. Furthermore, several previous studies have explored the toxicity and cosmetic outcomes of IORT boost+WBI. The studies concluded that IORT boost+WBI proved to be safe and feasible compared with conventional treatment, showing no treatment-related mortality, no delayed wound healing, or increased infection rates.19,44,45,46,47,48 According to research by experts, such as Lemanski47 and Salzburg,49 most patients were satisfied with the overall cosmetic effect after IORT+WBI treatment. In addition, for patients receiving IORT boost combined with hypofractionated whole breast irradiation (HWBI), the large, prospective, multicentre HIOB trial suggested that the patient’s early tolerance and cosmetic effect were excellent, but we still need to follow the data on its long-term follow-up.50
Advantages and Limitations
The efficacy of IORT alone has been highly questioned, resulting in the extremely slow development of intraoperative radiotherapy. However, IORT as a tumour bed boost combined with WBI is a new radiotherapy modality, and few comparative studies have investigated its efficacy and safety. The strength of our meta-analysis is that it is the first to bring together a systematic review and pooled analysis of relevant clinical studies of IORT boost+WBI compared with conventional radiotherapy. This meta-analysis provides important evidence for the use of IORT as a tumour bed boost. However, our study had some limitations. First, the major limitation of this meta-analysis was that quality scores, patient populations, treatment protocols, and follow-up periods varied across the studies. Second, our meta-analysis included only nine studies involving 3,219 patients. None of these nine studies were blinded, and eight of them were non-RCTs with lower evidence ratings than RCTs, suggesting that our studies are prone to systematic errors, such as selection bias. Moreover, one in nine studies accounted for nearly half of the total number of patients. However, most of the studies were prospective, controlled trials with high-quality scores. Third, as an effect measure of survival data, the statistics of local recurrence, distant recurrence, and especially OS rate were best combined by applying the hazard ratio (HR), 95% CI. However, in the literature included in this study, the majority of the original literature could not extract the time to death and cutoff data. Thus, we used RR instead of HR, which lost some important information compared with HR, meaning that the time factor was not considered. The author suggests that future, clinical trials should improve the follow-up and statistical results to provide more detailed data for the clinical application of IORT. These findings suggest that more high-quality, large-sample, prospective studies are needed to enhance the statistical validity of the combined effect values and validate the reliability of the findings.
Conclusions
This meta-analyses shows that patients with early-stage breast cancer who receive IORT boost+WBI after breast-conserving surgery show significantly better DMR and DFS than those who receive conventional radiotherapy. IORT boost+WBI also shows a tendency to beneficially effect LRR; electron boost exhibit more pronounced efficacy than x-ray boost. Additionally, the cosmetic outcome and adverse effects of IORT boost+WBI are comparable to conventional radiotherapy.
References
Latest Global Cancer Data: Cancer burden rises to 19.3 million new cases and 10.0 million cancer deaths in 2020.
Veronesi U, Marubini E, Mariani L, et al. Radiotherapy after breast-conserving surgery in small breast carcinoma: long-term results of a randomized trial. Ann Oncol. 2001;12(7):997–1003.
Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–41.
Wareńczak-Florczak Z, Roszak A, Bratos K, Milecki P, Karczewska-Dzionk A, Włodarczyk H. Intraoperative radiation therapy as part of breast conserving therapy of early breast cancer: results of one-year follow-up. Rep Pract Oncol Radiother. 2013;18(2):107–11.
Terheyden MM, Melchert C, Kovács G. External beam boost versus interstitial high-dose-rate brachytherapy boost in the adjuvant radiotherapy following breast-conserving therapy in early-stage breast cancer: a dosimetric comparison. J Contemp Brachyther. 2016;8(4):294–300.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG), Darby S, McGale P, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378(9804):1707–16.
Faverly DR, Hendriks JH, Holland R. Breast carcinomas of limited extent: frequency, radiologic-pathologic characteristics, and surgical margin requirements. Cancer. 2001;91(4):647–59.
Holland R, Veling SH, Mravunac M, Hendriks JH. Histologic multifocality of Tis, T1–2 breast carcinomas Implications for clinical trials of breast-conserving surgery. Cancer. 1985;56(5):979–90.
Fisher ER, Anderson S, Redmond C, Fisher B. Ipsilateral breast tumor recurrence and survival following lumpectomy and irradiation: pathological findings from NSABP protocol B-06. Semin Surg Oncol. 1992;8(3):161–6.
Huang J, Barbera L, Brouwers M, Browman G, Mackillop WJ. Does delay in starting treatment affect the outcomes of radiotherapy? a systematic review. J Clin Oncol. 2003;21(3):555–63.
Chen Z, King W, Pearcey R, Kerba M, Mackillop WJ. The relationship between waiting time for radiotherapy and clinical outcomes: a systematic review of the literature. Radiother Oncol. 2008;87(1):3–16.
Benda RK, Yasuda G, Sethi A, Gabram SG, Hinerman RW, Mendenhall NP. Breast boost: are we missing the target? Cancer. 2003;97(4):905–9.
Ramachandran P. New era of electronic brachytherapy. World J Radiol. 2017;9(4):148–54.
Schwid M, Donnelly ED, Zhang H. Therapeutic analysis of Intrabeam-based intraoperative radiation therapy in the treatment of unicentric breast cancer lesions utilizing a spherical target volume model. J Appl Clin Med Phys. 2017;18(5):184–94.
Veronesi U, Orecchia R, Maisonneuve P, et al. Intraoperative radiotherapy versus external radiotherapy for early breast cancer (ELIOT): a randomised controlled equivalence trial. Lancet Oncol. 2013;14(13):1269–77.
Orecchia R, Veronesi U, Maisonneuve P, et al. Intraoperative irradiation for early breast cancer (ELIOT): long-term recurrence and survival outcomes from a single-centre, randomised, phase 3 equivalence trial. Lancet Oncol. 2021;22(5):597–608.
Vaidya JS, Joseph DJ, Tobias JS, et al. Targeted intraoperative radiotherapy versus whole breast radiotherapy for breast cancer (TARGIT-A trial): an international, prospective, randomised, non-inferiority phase 3 trial. Lancet. 2010;376(9735):91–102.
Vaidya JS, Bulsara M, Baum M, et al. Long term survival and local control outcomes from single dose targeted intraoperative radiotherapy during lumpectomy (TARGIT-IORT) for early breast cancer: TARGIT-A randomised clinical trial. BMJ. 2020;370:m2836.
Ciabattoni A, Gregucci F, Fastner G, et al. IOERT versus external beam electrons for boost radiotherapy in stage I/II breast cancer: 10-year results of a phase III randomized study. Breast Cancer Res. 2021;23(1):46.
Fastner G, Reitsamer R, Ziegler I, et al. IOERT as anticipated tumor bed boost during breast-conserving surgery after neoadjuvant chemotherapy in locally advanced breast cancer–results of a case series after 5-year follow-up. Int J Cancer. 2015;136(5):1193–201.
Kolberg HC, Loevey G, Akpolat-Basci L, et al. Targeted intraoperative radiotherapy tumour bed boost during breast-conserving surgery after neoadjuvant chemotherapy. Zielgerichtete intraoperative Strahlentherapie als vorgezogener Boost im Rahmen der brusterhaltenden Operation nach neoadjuvanter Chemotherapie. Strahlenther Onkol. 2017;193(1):62–9.
Reitsamer R, Sedlmayer F, Kopp M, et al. The Salzburg concept of intraoperative radiotherapy for breast cancer: results and considerations. Int J Cancer. 2006;118(11):2882–7.
Sperk E, Welzel G, Keller A, et al. Late radiation toxicity after intraoperative radiotherapy (IORT) for breast cancer: results from the randomized phase III trial TARGIT A. Breast Cancer Res Treat. 2012;135(1):253–60.
Welzel G, Hofmann F, Blank E, et al. Health-related quality of life after breast-conserving surgery and intraoperative radiotherapy for breast cancer using low-kilovoltage X-rays. Ann Surg Oncol. 2010;17(Suppl 3):359–67. https://doi.org/10.1245/s10434-010-1257-z.
Kraus-Tiefenbacher U, Bauer L, Kehrer T, Hermann B, Melchert F, Wenz F. Intraoperative radiotherapy (IORT) as a boost in patients with early-stage breast cancer: acute toxicity. Onkologie. 2006;29(3):77–82.
Sorrentino L, Fissi S, Meaglia I, et al. One-step intraoperative radiotherapy optimizes conservative treatment of breast cancer with advantages in quality of life and work resumption. Breast. 2018;39:123–30.
Hashemi S, Javadi S, Akbari ME, Mirzaei H, Mahdavi SR. Comparison of IORT (radical and boost dose) and EBRT in terms of disease-free survival and overall survival according to demographic, pathologic, and biological factors in patients with breast cancer. Int J Surg Oncol. 2021;2021:2476527.
Fadavi P, Nafissi N, Mahdavi SR, Jafarnejadi B, Javadinia SA. Outcome of hypofractionated breast irradiation and intraoperative electron boost in early breast cancer: A randomized non-inferiority clinical trial. Cancer Rep (Hoboken). 2021;4(5):e1376.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
PEDro scale. https://pedro.org.au/english/resources/pedro-scale/
de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129–33.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–6.
Ciabattoni A, Gregucci F, Llange K, et al. Intraoperative electron radiation therapy (IOERT) anticipated boost in breast cancer treatment: An Italian multicenter experience. Cancers (Basel). 2022;14(2):292.
Jazmati D, Bölke E, Halfmann K, et al. Early outcome, cosmetic result and tolerability of an IOERT-boost prior to adjuvant whole-breast irradiation. Cancers (Basel). 2022;14(15):3636.
Stoian R, Erbes T, Zamboglou C, et al. Intraoperative radiotherapy boost as part of breast-conservation therapy for breast cancer: a single-institution retrospective analysis. Strahlenther Onkol. 2021;197(9):812–9.
Oses G, Cases C, Valduvieco I, et al. Chronic toxicity and long-term outcome in intraoperative electron radiotherapy as boost followed by whole-breast irradiation. Clin Transl Oncol. 2021;23(8):1593–600.
Valente SA, Tendulkar RD, Cherian S, et al. TARGIT-R (Retrospective): 5-Year follow-up evaluation of intraoperative radiation therapy (IORT) for breast cancer performed in North America. Ann Surg Oncol. 2021;28(5):2512–21. https://doi.org/10.1245/s10434-020-09432-3.
Pez M, Keller A, Welzel G, et al. Long-term outcome after intraoperative radiotherapy as a boost in breast cancer Langzeitergebnisse nach intraoperativem Boost bei Brustkrebs. Strahlenther Onkol. 2020;196(4):349–55.
Onthong K, Chakkabat C, Nantavithya C, et al. Results of intraoperative radiotherapy given as a boost after breast conserving-surgery. Gland Surg. 2020;9(5):1389–95.
Machiels M, Weytjens R, Erven K, et al. Oncological outcome, postoperative complications, and mammographic changes after intraoperative radiotherapy with electrons (IOERT) as a boost in a large single-institution cohort of breast cancer patients. Breast J. 2020;26(10):1937–45.
König L, Lang K, Heil J, et al. Acute toxicity and early oncological outcomes after intraoperative electron radiotherapy (IOERT) as boost followed by whole breast irradiation in 157 early stage breast cancer patients-first clinical results from a single center. Front Oncol. 2019;9:384.
Ahn SG, Bae SJ, Lee HW, et al. A phase II study investigating the acute toxicity of targeted intraoperative radiotherapy as tumor-bed boost plus whole breast irradiation after breast-conserving surgery in Korean patients. Breast Cancer Res Treat. 2019;174(1):157–63.
Kaiser J, Kronberger C, Moder A, et al. Intraoperative tumor bed boost with electrons in breast cancer of clinical stages I through III: Updated 10-year results. Int J Radiat Oncol Biol Phys. 2018;102(1):92–101.
Merrick HW 3rd, Battle JA, Padgett BJ, Dobelbower RR Jr. IORT for early breast cancer: a report on long-term results. Front Radiat Ther Oncol. 1997;31:126–30.
Vaidya JS, Baum M, Tobias JS, et al. Targeted intra-operative radiotherapy (Targit): an innovative method of treatment for early breast cancer. Ann Oncol. 2001;12(8):1075–80.
Reitsamer R, Peintinger F, Sedlmayer F, et al. Intraoperative radiotherapy given as a boost after breast-conserving surgery in breast cancer patients. Eur J Cancer. 2002;38(12):1607–10.
Lemanski C, Azria D, Thezenas S, et al. Intraoperative radiotherapy given as a boost for early breast cancer: long-term clinical and cosmetic results. Int J Radiat Oncol Biol Phys. 2006;64(5):1410–5.
Ivaldi GB, Leonardi MC, Orecchia R, et al. Preliminary results of electron intraoperative therapy boost and hypofractionated external beam radiotherapy after breast-conserving surgery in premenopausal women. Int J Radiat Oncol Biol Phys. 2008;72(2):485–93.
Fussl C, Merz F, Fussl A, Fastner G, Reitsamer R, Sedlmayer F, et al. Evaluation of cosmetic Long-term results in early breast cancer after intraoperative Radiotherapy (IORT) as part of breast-conserving Therapy [Abstract]. Strahlenther Onkol. 2012;188:189.
Fastner G, Reitsamer R, Urbański B, et al. Toxicity and cosmetic outcome after hypofractionated whole breast irradiation and boost-IOERT in early stage breast cancer (HIOB): first results of a prospective multicenter trial (NCT01343459). Radiother Oncol. 2020;146:136–42.
Acknowledgment
The authors acknowledge the support of the Breast Department, Guangdong Provincial Hospital of Chinese Medicine.
Funding
None.
Author information
Authors and Affiliations
Contributions
JH and SC performed the study concept and design, literature collection, and data analysis, and wrote the manuscript. LY and YS conducted the literature screening, data collection and quality assessment. YD, XS and XL contributed to the data analysis and designed the layout of the manuscript. RX verified the data, revised the manuscript, and was responsible for the integrity of the work as a whole.
Corresponding author
Ethics declarations
Disclosure
The authors declare that they have no actual or potential conflicts of interest exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
He, J., Chen, S., Ye, L. et al. Intraoperative Radiotherapy as a Tumour-Bed Boost Combined with Whole Breast Irradiation Versus Conventional Radiotherapy in Patients with Early-Stage Breast Cancer: A Systematic Review and Meta-analysis. Ann Surg Oncol 30, 8436–8452 (2023). https://doi.org/10.1245/s10434-023-13955-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13955-w