Abstract
Background
Lymph node invasion is associated with poor outcome in patients with renal cell carcinoma (RCC).
Patients and Methods
Patients with RCC within a single center from 2001 to 2018 were retrospectively obtained from the Chang Gung Research Database. Patient gender, physical status, Charlson Comorbidity Index, tumor side, histology, age at diagnosis, and body mass index (BMI) were compared. The overall survival (OS) and cancer-specific survival (CSS) of each group were estimated using the Kaplan–Meier method. Log-rank tests were used to compare between the subgroups.
Results and Conclusions
A total of 335 patients were enrolled, of whom 76 had pT3N0M0, 29 had pT1–3N1M0, 104 had T1–4N0M1, and 126 had T1–4N1M1 disease. Significant OS difference was noted between pT3N0M0 and pT1–3N1M0 groups with 12.08 years [95% confidence interval (CI), 8.33–15.84] versus 2.58 years (95% CI, 1.32–3.85), respectively (P < 0.005). No significant difference was observed in OS between pT1–3N1M0 and T1–4N0M1 groups with 2.58 years (95% CI, 1.32–3.85) versus 2.50 years (95% CI, 1.85–3.15, P = 0.72). The OS of N1M1 group was worse than that of N0M1 group with 1.00 year (95% CI, 0.74–1.26) versus 2.50 years (95% CI, 1.85–3.15, P < 0.05). Similar results were also observed in CSS. In summary, we claim that RCC with lymph node (LN) invasion should be reclassified as stage IV disease in terms of survival outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
According to the eighth edition of the American Joint Committee on Cancer (AJCC) tumor–node–metastasis (TNM) staging system,1 patients with renal cell carcinoma (RCC) with T1–3N1M0 or T3N0M0 status are classified as stage III, while T4 and M1 status are classified as stage IV. A recent study reported that the overall survival (OS) of patients with stage III cancer with pathologic nodal involvement and those without was 2.4 years [95% confidence interval (CI) 1.7–4.1 years] and 10.2 years (95% CI, 8.7 years–not applicable), respectively.2 The study also pointed out that the survival rate of patients with node-positive RCC was similar to that of patients with stage IV disease instead of stage III.
Lymph node (LN) invasion is present in about 4.7% of patients with RCC.3 As a vital prognostic predictor in patients with RCC, LN invasion affects the survival outcome and disease aggressiveness.4,5 According to current guidelines, LN dissection (LND) does not improve oncological outcomes in patients with clinically node-positive disease; however, it may be beneficial for precise staging.6,7
Survival impact of LN invasion was noted in other genitourinary tract malignancies, such as bladder cancer, and it was also the pivot for the success of treatment.8 Studies that focus on whether LN invasion has impact on survival must be conducted precisely to find out the divergent presentation according to treatment stratification. As the most recognized staging system, TNM classification is consistently revised via including more stratification to reflect the outcomes according to the rapid pace of modern treatment.9 As the third most common genitourinary tract malignancy, approximately 403,262 RCC cases were newly diagnosed globally, with 175,098 deaths in 2018,10 and incidence exhibiting an increasing trend as well.11 With rapid eruption of systemic treatment in the recent decade, continuous monitoring and revision of the staging system is mandatory to provide most updated treatment guidance and risk stratification accordingly.12
Currently, there is only one study advocating that LN invasion should be considered as stage IV, and more than 70% of the study population was Caucasian.2 The result was not formally verified in the Asian population, and previous studies reported the difference of survival between races with RCC.13 Our study provides the result for Asian patients and verifies the detrimental impact of LN invasion on survival outcome in RCC.
Patients and Methods
Data Collection
Data for this study were retrospectively collected from the Chang Gung Research Database (CGRD) after obtaining approval from the Institutional Review Board of the Chang Gung Medical Foundation. The CGRD, an encrypted database of electronic medical records from Chang Gung Memorial Hospital, covers approximately 6% and 10% of outpatient and hospitalized patients, respectively, in Taiwan.14 The CGRD is more accurate than other nationwide databases in terms of information; for instance, it contains complete pathological and laboratory reports.15 In addition, the CGRD provides key information such as diagnostic codes from both outpatient and inpatient departments, pathological reports, records of medical orders, procedures, recorded vital signs, nursing records, and perioperative condition during anesthesia. In this study, we recorded and stored all essential information by using the structured query language database. We excluded duplicated data by following a standard quality control process.
Methods
From the CGRD, we retrospectively obtained the data of patients with RCC from one center between 2001 and 2018. The diagnosis of RCC was reviewed and identified according to the International Classification of Disease, Clinical Modification, Ninth Revision (ICD-9-CM) code 189* and the International Classification of Disease, Clinical Modification, Tenth Revision (ICD-10-CM) code C64* assigned by physicians. We only included patients with stage III or IV RCC in this study. The eighth edition of the 2018 AJCC staging system was used for the TNM staging of patients.1 We excluded patients with missing information for diagnosis or surgery in the database. The flow of our study design is displayed in our CONSORT diagram (Fig. 1). Our study design was reviewed and approved by the Center for Big Data Analytics and Statistics (Grant CLRPG3D0045) at Chang Gung Memorial Hospital.
In this study, patient characteristics are summarized as numerical and categorical variables, namely the American Society of Anesthesiologists (ASA) physical status classification, Eastern Cooperative Oncology Group Performance Status (ECOG-PS) score, and Charlson Comorbidity Index. In line with other methodological studies, the Charlson Comorbidity Index was calculated using ICD-9-CM and ICD-10-CM codes in both outpatient and inpatient departments.16,17
Statistical Analysis
We used R (version 3.3.0, 2016-05-03) to perform statistical analyses. To compare patient characteristics between subgroups, we used Fisher’s exact test for categorical variables, namely sex, American Society of Anesthesiologists (ASA) physical status classification, ECOG-PS score, Charlson comorbidity index, tumor side, and cell type, and the Mann–Whitney–Wilcoxon test for continuous and ordinal variables, namely age at diagnosis and body mass index (BMI). OS was defined as the interval between date of RCC diagnosis and date of death from any cause or last follow-up date for patients who were still alive. Cancer-specific survival (CSS) was defined as the interval between date of RCC diagnosis and date of death due to RCC. Patients who died of other causes were censored at date of death, whereas patients who were alive were censored at last follow-up date. The OS and CSS of each group were estimated using the Kaplan–Meier method. The Mantel–Cox log-rank test was performed to compare OS and CSS between subgroups. Finally, for OS and CSS, we used the univariate Cox proportional-hazards model for important clinical variables. Subsequently, we included statistically significant variables (P < 0.05) in the multivariate Cox proportional-hazards model.
Results
Patient Characteristics
Of the 335 patients included in this study, 76 had pT3N0M0, 29 had pT1–3N1M0, and 230 had metastatic disease (104 and 126 had T1–4N0M1 and T1–4N1M1 disease, respectively). The median age of patients was 60 years, and the median Charlson Comorbidity Index was 4. Most patients had an ECOG-PS score of 0 or 1 (87% in total). Table 1 summarizes the characteristics of subgroups included in this study.
Throughout the parameters we have collected in the study, no statistically significant difference was noted between the PT1–3N1M0 versus M1 group. No significant difference was observed between patients with pT3N0M0 and those with pT1–3N1M0. However, a significant difference in the cell type was noted between the pT1–3N1M0 and metastatic (M1) groups (P = 0.002); patients in the metastatic group had more clear cell tumors. The distribution of demographics, including median age, sex, and comorbidities, was similar among the subgroups.
Overall Survival
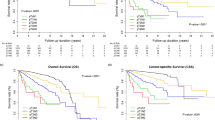
Figure 2 shows the Kaplan–Meier estimates of OS in the four subgroups, and Table 2 presents the results of the comparison of median OS and CSS among the four subgroups. The median OS was 2.41 years (95% CI, 1.90–2.93 years). In total, 217 deaths occurred during follow-up. A significant difference was observed in OS among the four subgroups (P < 0.005).
Among patients with stage III disease, the pT1–3N1M0 group had a median OS of 2.58 years (95% CI, 1.42 years to not estimable), which was shorter than that of patients without nodal involvement (pT3N0M0 group, median OS, 12.08 years, 95% CI, 9.83 years to not estimable, P < 0.005). However, the difference in OS between the pT1–3N1M0 and T1–4N0M1 groups was nonsignificant (P = 0.72), with OS of 2.58 years (95% CI, 1.42 years to not estimable) and 2.50 years (95% CI, 1.75–3.75 years), respectively. Thus, the OS of the pT1–3N1M0 group was similar to that of the metastatic group rather than the pT3N0M0 group.
Even within the metastatic group, patients with LN invasion (T1–4N1M1) exhibited poorer survival outcomes than did those without (T1–4N0M1), with a median OS of 1.00 year (95% CI, 0.75–1.42 years) versus 2.50 years (95% CI, 1.75–3.75 years, P < 0.05). These findings indicate that pathologic LN invasion resulted in poorer clinical outcomes in the metastatic groups.
Cancer-Specific Survival
As shown in Fig. 3, the CSS results were similar to those for OS. The median CSS was 4.67 (95% CI, 1.67–7.67) years in the whole cohort. However, the median CSS and its 95% CI could not be calculated for the pT3N0M0 and pT1–3N1M0 groups, as they did not reach median survival. Similar to the results for OS, the difference in CSS between the pT1–3N1M0 and T1–4N0M1 groups was nonsignificant (P = 0.52), with a CSS of 4.08 years (95% CI, 2.58 years to not estimable) versus 3.5 years (95% CI, 2.5 years to not estimable); by contrast, the CSS of the pT1–3N1M0 group was significantly shorter than that of the pT3N0M0 group (P < 0.05), with a CSS of 4.08 years (95% CI, 2.58 years to not estimable) versus not estimable years (95% CI, 12.08 years to not estimable). The pairwise comparisons of each group are presented in Table 2. Similar patterns of discrimination in CSS were observed between the pT3N0M0 and T1–4N0M1 groups and between the two metastatic groups.
Univariate and Multivariate Cox Proportional-Hazards Models
Tables 3 and 4 present the fit univariate and multivariate Cox models for OS and CSS in our patients, respectively. This is done by only a subset of patients (N = 105, instead of 335) due to the limitation of the database. We found that the ASA physical status, Charlson Comorbidity Index, and pathological nodal disease (pN1) were significantly associated with poor OS. Moreover, only the Charlson Comorbidity Index and pN1 were predictive of poor CSS.
Discussion
In clinical practice, an accurate staging system such as TMN staging can help in decision-making for treatment, assessing prognosis and treatment outcomes, and stratifying patients in different treatment modality cohorts.18 An updated and well-validated staging system should be established for disease stratification in terms of recurrence or progression risk and for individualized adjuvant therapy plans. The results in the present study revealed that patients with stage III RCC with pathological LN invasion demonstrated poorer OS and CSS than did those without nodal disease. In addition, we found that the survival outcome of patients with stage III RCC with pathological LN invasion was similar to that of patients with stage IV RCC. There are still some points in argument under current practice. First, the number of LNs to be removed was determined according to the template chosen by surgeons for different clinical scenarios, and the number of positive LNs removed depended on the pathologist’s diligence. In addition, LND was not routinely performed with nephrectomy in low-risk patients, and the recent meta-analysis by Wei et al. even demonstrated that unnecessary LND could be detrimental and shorten the CSS if all nonmetastatic patients with RCC underwent LND during radical nephrectomy (HR 1.22, 95% CI 1.05–1.43).19 On the contrary, although cytoreductive nephrectomy was no longer the gold standard operation for mRCC in the era of targeted therapy, according to the results from the CARMENA study, it is worth paying attention to the observation that lymph node yield via meticulous dissection could prolong OS in the setting of cytoreductive nephrectomy in patients with mRCC (HR 0.97; 95% CI 0.95–0.99).20,21 Thus, surgeons’ selection bias can substantially undermine the clinical application of LND. Accordingly, LN staging can be reliable only if every part of the process is standardized.
Given the advanced nature of nodal disease in RCC, many centers identify patients with a high risk of LN invasion either perioperatively or preoperatively to optimize the efficacy of retroperitoneal LND during nephrectomy. A study proposed that, on the basis of age, symptom classification, and tumor size, the predictive accuracy for pathologic nodal disease was 78.4%.22 Another study standardized a pre-surgery model involving a scoring system with four independent predictors, namely tumor stage (cT3–4 versus cT1–2, score 1 versus 0), clinical nodal status (cN1 versus cN0, score 1 versus 0), metastasis at diagnosis (cM1 versus cM0, score 1 versus 0), and clinical tumor size (2–20 cm, score 60–220); the predictive accuracy of the model was reported to be 86.9%.4 Another study defined the predictors of LN involvement as follows: intraoperative pathologic feature with nuclear grade 3 or 4, presence of a sarcomatoid component, tumor size ≥ 10 cm, tumor stage of pT3 or pT4, and histological tumor necrosis.23
One important study compared OS and CSS between patients with node-positive stage III and stage IV disease.2 The median OS of patients with T1–3N1M0 and patients with stage IV cancer in the aforementioned study was 2.4 years (95% CI, 1.7–4.1 years, respectively). Their results are similar to those of our study, in which the OS of the pT3N1M0 group was 2.58 years (95% CI, 1.42 years to not estimable). These similar findings may indicate that the OS of patients with RCC and node-positive stage III cancer approximates that of patients with stage IV cancer.
Concordantly, our results indicated that, within the metastatic group, the T1–4N1M1 group had poorer OS and CSS than did the T1–4N0M1 group. This finding has not been reported in previous studies and indicates that LN invasion exerted a detrimental effect on survival outcomes even in patients who already had distant metastasis. Although the advantage of LND on survival outcome is still under investigation, and most retrospective reviews did not support the necessity in combination with all nephrectomies, the survival outcome and aggressiveness of disease progression were apparently associated with nodal metastasis.24,25,26 The association of tumor characteristics and lymph node invasion also revealed that the percentage of pathologic nodal disease was higher in advanced tumor stage, with 1.1% in stage T1, 4.5% in T2, and 12.3% in T3.27 Interestingly, another study by Sun et al. concluded from the multivariate analysis with the SEER database enrolling 11,374 patients with nonmetastatic RCC who underwent LND that the mortality rate declined from pT1 to pT4 patients with nodal metastases as 6.0-, 3.6-, 3.2-, and 2.0-fold after nephrectomy, respectively (all P < 0.001).28 These findings verified the lethality of lymph node invasion and it deserved clinical attention as much as other predictors leading to poor outcomes. It is also confirmed in the multivariate Cox model that the Charlson Comorbidity Index and pathological LN invasion are associated with OS and CSS. On the basis of this finding, LN invasion should be considered an independent marker of poor survival outcomes.
Although clinical guidelines indicate LND application in patients with RCC with clinically node-positive disease, the extent of LND and its standard protocol remain controversial due to the complexity of the disease and lack of consensus on dissection. Several studies have demonstrated that LND provides a long-term survival benefit when LN invasion is clinically evident.29 In contrast, the results of a randomized phase III trial published in 2009 by the European Organization for Research and Treatment of Cancer Genitourinary Group declared no survival benefit in 30,881 patients who underwent LND in conjunction with radical nephrectomy.30 However, criticism regarding the small number of high-risk patients included in the trial undermined its clinical contribution.31
Even if a meta‐analysis in 2018 revealed that the relevant literature did not report a survival benefit of LND for M0 or M1 RCC, evidence on this topic for patients with high‐risk M0 RCC has still been inconclusive.19 In addition, another review showed no or uncertain therapeutic benefit regarding LND in different groups of patients.32 Moreover, recent studies have revealed that LND in RCC did not increase the incidence of surgical complications or major perioperative complications, with only a slight increase in Clavien grade 2 complications.12,25,33 Considering the poor OS and CSS of patients with nodal disease, routine LND may still be valuable to make precise staging of patients with clinically high-risk RCC. Additional prospective studies on LND for patients with cT1–3N1M0 are in great need of outcome surveillance to further validate this hypothesis.
Our study has several limitations based on its retrospective nature. First, although patients in our study were treated in one single center, controversy regarding the template indicated that each surgeon’s LND policy might be different. Although most surgeons in our center tended to perform LND in patients with clinical nodal disease according to most experts’ opinion, not all patients in our study underwent adequate dissection. Second, the current study included data from only one tertiary center, and it would be more influential if we could include the whole patient data from all our local branches. It is not open for access currently, but we will initiate further analysis for external validation once the limitation is dismissed. Now that in this present study we analyzed a smaller cohort, it was relatively more unified in terms of the principle of LND than all branch hospitals included.
Regarding the diversity of histology, pathologic grade, age at diagnosis, and underlying diseases in patients with RCC, LN invasion should be taken as an indicator and more attention should be paid in the same way we did for distant metastasis. The detrimental effect could be verified not only for patients with stage III disease, but also for those with distant metastatic disease. Prognostic systems such as TNM staging must be continually revised on the basis of currently available evidence.34,35 Our study supported the hypothesis that LN invasion should be reclassified as stage IV disease in RCC.
LN invasion in patients with renal cell carcinoma indicates poor clinical outcome. Stage III patients with pathologic nodal disease should be reclassified as stage IV metastatic disease according to this clinical marker verified with poor outcome.
References
AJCC Cancer Staging Manual | Mahul B. Amin | Springer. Accessed July 15, 2019. https://www.springer.com/gp/book/9783319406176
Yu KJ, Keskin SK, Meissner MA, et al. Renal cell carcinoma and pathologic nodal disease: implications for American Joint Committee on Cancer staging. Cancer. 2018;124(20):4023–31. https://doi.org/10.1002/cncr.31661.
European temporal trends in the use of lymph node dissection in patients with renal cancer—ScienceDirect. Accessed June 28, 2021. https://www.sciencedirect.com/science/article/pii/S0748798317306005
Capitanio U, Suardi N, Matloob R, et al. Extent of lymph node dissection at nephrectomy affects cancer-specific survival and metastatic progression in specific sub-categories of patients with renal cell carcinoma (RCC). BJU Int. 2014;114(2):210–5. https://doi.org/10.1111/bju.12508.
Liao X, Qiu S, Zheng X, et al. Lymph node density as an independent prognostic factor in node-positive renal-cell carcinoma: results from the Surveillance, Epidemiology, and End Results Program. Clin Genitourin Cancer. 2019;17(5):e968–80. https://doi.org/10.1016/j.clgc.2019.05.011.
Ljungberg B, Albiges L, Abu-Ghanem Y, et al. European Association of Urology Guidelines on renal cell carcinoma: the 2019 Update. Eur Urol. 2019;75(5):799–810. https://doi.org/10.1016/j.eururo.2019.02.011.
Campbell S, Uzzo RG, Allaf ME, et al. Renal mass and localized renal cancer: AUA Guideline. J Urol. 2017;198(3):520–9. https://doi.org/10.1016/j.juro.2017.04.100.
Stein JP, Lieskovsky G, Cote R, et al. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol. 2001;19(3):666–75. https://doi.org/10.1200/JCO.2001.19.3.666.
Reim D, Loos M, Vogl F, et al. Prognostic implications of the seventh edition of the international union against cancer classification for patients with gastric cancer: the Western experience of patients treated in a single-center European institution. J Clin Oncol. 2013;31(2):263-271. https://doi.org/10.1200/JCO.2012.44.4315
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Ljungberg B, Campbell SC, Cho HY, et al. The epidemiology of renal cell carcinoma. Eur Urol. 2011;60(4):615–21. https://doi.org/10.1016/j.eururo.2011.06.049.
Gospodarowicz MK, Miller D, Groome PA, Greene FL, Logan PA, Sobin LH. The process for continuous improvement of the TNM classification. Cancer. 2004;100(1):1–5. https://doi.org/10.1002/cncr.11898.
Stafford HS, Saltzstein SL, Shimasaki S, Sanders C, Downs TM, Sadler GR. Racial/ethnic and gender disparities in renal cell carcinoma incidence and survival. J Urol. 2008;179(5):1704–8. https://doi.org/10.1016/j.juro.2008.01.027.
Shao SC, Chan YY, Kao Yang YH, et al. The Chang Gung Research Database—a multi-institutional electronic medical records database for real-world epidemiological studies in Taiwan. Pharmacoepidemiol Drug Saf. 2019;28(5):593–600. https://doi.org/10.1002/pds.4713.
Tsai MS, Lin MH, Lee CP, et al. Chang Gung Research Database: a multi-institutional database consisting of original medical records. Biomed J. 2017;40(5):263–9. https://doi.org/10.1016/j.bj.2017.08.002.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–94. https://doi.org/10.1016/j.jclinepi.2004.03.012.
Huang SH, Xu W, Waldron J, et al. Refining American Joint Committee on Cancer/Union for International Cancer Control TNM stage and prognostic groups for human papillomavirus–related oropharyngeal carcinomas. J Clin Oncol. 2015;33(8):836–45. https://doi.org/10.1200/JCO.2014.58.6412.
Bhindi B, Wallis CJD, Boorjian SA, et al. The role of lymph node dissection in the management of renal cell carcinoma: a systematic review and meta-analysis. BJU Int. 2018;121(5):684–98. https://doi.org/10.1111/bju.14127.
Méjean A, Ravaud A, Thezenas S, et al. Sunitinib alone or after nephrectomy in metastatic renal-cell carcinoma. N Engl J Med. 2018;379(5):417–27. https://doi.org/10.1056/NEJMoa1803675.
Bai Y, Li S, Jia Z, Ding Y, Gu C, Yang J. Adjuvant therapy for locally advanced renal cell carcinoma: a meta-analysis and systematic review. Urol Oncol Semin Orig Investig. 2018;36(2):79.e1-79.e10. https://doi.org/10.1016/j.urolonc.2017.10.001.
Hutterer GC, Patard JJ, Perrotte P, et al. Patients with renal cell carcinoma nodal metastases can be accurately identified: external validation of a new nomogram. Int J Cancer. 2007;121(11):2556–61. https://doi.org/10.1002/ijc.23010.
Blute ML, Leibovich BC, Cheville JC, Lohse CM, Zincke H. A protocol for performing extended lymph node dissection using primary tumor pathological features for patients treated with radical nephrectomy for clear cell renal cell carcinoma. J Urol. 2004;172(2):465–9. https://doi.org/10.1097/01.ju.0000129815.91927.85.
Gershman B, Thompson RH, Moreira DM, et al. Lymph node dissection is not associated with improved survival among patients undergoing cytoreductive nephrectomy for metastatic renal cell carcinoma: a propensity score based analysis. J Urol. 2017;197(3 Pt 1):574–9. https://doi.org/10.1016/j.juro.2016.09.074.
Crispen PL, Breau RH, Allmer C, et al. Lymph node dissection at the time of radical nephrectomy for high-risk clear cell renal cell carcinoma: indications and recommendations for surgical templates. Eur Urol. 2011;59(1):18–23. https://doi.org/10.1016/j.eururo.2010.08.042.
Delacroix SE, Chapin BF, Chen JJ, et al. Can a durable disease-free survival be achieved with surgical resection in patients with pathological node positive renal cell carcinoma? J Urol. 2011;186(4):1236–41. https://doi.org/10.1016/j.juro.2011.05.051.
Capitanio U, Jeldres C, Patard JJ, et al. Stage-specific effect of nodal metastases on survival in patients with non-metastatic renal cell carcinoma. BJU Int. 2009;103(1):33–7. https://doi.org/10.1111/j.1464-410X.2008.08014.x.
Sun M, Bianchi M, Hansen J, et al. Nodal involvement at nephrectomy is associated with worse survival: a stage-for-stage and grade-for-grade analysis. Int J Urol. 2013;20(4):372–80. https://doi.org/10.1111/j.1442-2042.2012.03170.x.
Canfield SE, Kamat AM, Sánchez-Ortiz RF, Detry M, Swanson DA, Wood CG. Renal cell carcinoma with nodal metastases in the absence of distant metastatic disease (clinical stage TxN1-2M0): the impact of aggressive surgical resection on patient outcome. J Urol. 2006;175(3 Pt 1):864–9. https://doi.org/10.1016/S0022-5347(05)00334-4.
Blom JHM, van Poppel H, Maréchal JM, et al. Radical nephrectomy with and without lymph-node dissection: final results of European Organization for Research and Treatment of Cancer (EORTC) randomized phase 3 trial 30881. Eur Urol. 2009;55(1):28–34. https://doi.org/10.1016/j.eururo.2008.09.052.
Whitson JM, Harris CR, Reese AC, Meng MV. Lymphadenectomy improves survival of patients with renal cell carcinoma and nodal metastases. J Urol. 2011;185(5):1615–20. https://doi.org/10.1016/j.juro.2010.12.053.
Patel HD, Karam JA, Allaf ME. Surgical management of advanced kidney cancer: the role of cytoreductive nephrectomy and lymphadenectomy. J Clin Oncol. 2018. https://doi.org/10.1200/JCO.2018.79.0246.
Gershman B, Moreira DM, Thompson RH, Boorjian SA, Lohse CM, Costello BA, et al. Perioperative morbidity of lymph node dissection for renal cell carcinoma: a propensity score–based analysis. Eur Urol. 2018;73(3):469–75. https://doi.org/10.1016/j.eururo.2017.10.020.
Ficarra V, Galfano A, Mancini M, Martignoni G, Artibani W. TNM staging system for renal-cell carcinoma: current status and future perspectives. Lancet Oncol. 2007;8(6):554–8. https://doi.org/10.1016/S1470-2045(07)70173-0.
Kim MK, Warner RRP, Roayaie S, et al. Revised staging classification improves outcome prediction for small intestinal neuroendocrine tumors. J Clin Oncol. 2013;31(30):3776–81. https://doi.org/10.1200/JCO.2013.51.1477.
Acknowledgement
The authors would like to thank Linkou Chang Gung Memorial Hospital for support via Grant CORPG3K0151.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure
The authors have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yu, KJ., Chen, SY., Lin, PH. et al. Should Patients with Renal Cell Carcinoma and Pathological Nodal Invasion Be Classified As Having Stage IV Disease?. Ann Surg Oncol 30, 5286–5294 (2023). https://doi.org/10.1245/s10434-022-12979-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12979-y