Abstract
Background
Standard sentinel lymph node procedure (SNP) in pediatric cancer consists of a preoperative injection with 99mtechnetium nanocolloid in combination with an optional intraoperative injection with blue dye. However, blue dye has disadvantages, and the detection rate is low, with only 60% of sentinel lymph nodes (SLNs) staining blue. In adult oncology, fluorescence imaging using indocyanine green (ICG) has been shown to be a safe and accurate method for visual detection of SLNs, with a higher sensitivity (up to 97%) compared with blue dye. Therefore, our aim is to determine the feasibility of the addition of ICG to 99mtechnetium nanocolloid (ICG–TC) for visual detection of SLN in pediatric patients.
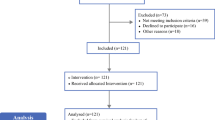
Methods
A total of 15 pediatric patients with melanoma, squamous cell carcinoma, and sarcoma were prospectively included. Preoperatively, patients were injected with ICG–TC and imaging with lymphoscintigraphy and single-photon emission computed tomography– computed tomography was performed. Intraoperatively, SLN was detected with fluorescence and the gamma probe. Postoperatively, fluorescence was quantified by tumor-to-background ratio (TBR) and surgeons evaluated the use of ICG using a standardized questionnaire.
Results
In 10/15 (67%) patients, SLNs were visible transcutaneously. Of all intraoperatively detected SLNs, 35/37 (95%) were fluorescent and 37/37 (100%) were radioactive. Furthermore, ICG–TC led to the identification of six additional SLNs as compared with preoperative imaging. The median TBR in vivo was 6.5 (IQR 5.3). The surgical evaluation showed that ICG assisted in SLN detection and was easy to use.
Conclusions
ICG–TC for the SNP is a feasible procedure in pediatric patients. It showed an accurate detection rate, was helpful for visual guidance, and no adverse events occurred.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The standard-of-care sentinel lymph node (SLN) procedure in pediatric patients with cancer consists of a preoperative intradermal or peritumoral injection with 99mtechnetium nanocolloid as radiotracer in combination with an intraoperative injection of blue dye for visual guidance. This method has been proven to accurately detect SLN in pediatric patients with melanoma and sarcoma, with a detection rate of around 95%.1,2
Successful SNP depends on SLN localization using a dye and/or radiotracer, such as 99mtechnetium-nanocolloid, that can be visualized with preoperative imaging and detected intraoperatively by a handheld gamma probe. However, disadvantages of using a radiotracer are the potential disturbance of the radioactive signal originating from the injection site, a low spatial resolution, and the fact that the surgery has to be interrupted to use the gamma probe. Consequently, detection of SLN is sometimes complicated and demanding. The radiotracer limitations can be eliminated by using an agent that could aid visual guidance simultaneously without interrupting the surgery. Therefore, when visual guidance is wanted by the surgeon, the use of blue dye is currently added to the SLN procedure. However, blue dye has evident disadvantages, such as risk of (severe) allergic reactions (2%3) and long-lasting tattooing (41% after 12 months4), in addition to the limited penetration depth and alteration of the surgical field.3,4,5 Furthermore, the efficacy is low, with only 60% of SLNs staining blue.6
In adult patients with melanoma, near-infrared (NIR) fluorescence imaging using indocyanine green (ICG) has been shown to be a safe, efficient, and accurate method for intraoperative visual detection of SLNs, with a higher sensitivity (up to 97%) compared with blue dye.6 However, in most studies ICG is used in combination with 99m technetium nanocolloid, potentially overestimating the sensitivity of ICG alone. For pediatric patients, good safety profiles for the use of ICG have been established for indications other than SLN.7
Our aim is to determine the feasibility of the addition of ICG to 99mtechnetium nanocolloid for visual detection of SLN in pediatric patients. Owing to the high sensitivity of ICG in adults and the good safety and favorable side effects profile of ICG compared with blue dye, we expect that a combined injection of ICG noncovalently bound to 99mTc nanocolloid (ICG–99m Tc nanocolloid, ICG–TC) is able to improve visual guidance during surgery, while preventing the considerable risk of side effects associated with blue dye.8
Patients and Methods
Patients
This study (NL71166.041.20) was approved by the Institutional Review Board.
Inclusion criteria were: 1. Under the age of 18 years; 2. Diagnosis of melanoma, sarcoma or squamous cell carcinoma of extremity, head and neck, or trunk; and 3. Indication to undergo a SLN procedure. Exclusion criteria were: 1. Allergy to iodine; 2. Hypersensitivity to ICG; 3. Kidney insufficiency (eGFR < 45); and 4. Clinically manifest hyperthyroidism or autonomous thyroid adenoma. In total, 15 patients, (9 with melanoma, 4 with sarcoma, and 2 with squamous cell carcinoma) were prospectively included after giving informed consent (Table 1). All patients were clinically node negative as assessed by palpation.
Tracer Preparation, Administration, and Preoperative Imaging
Preparation and labeling of ICG–TC was performed in the UMC Utrecht according to the good manufacturing practice (GMP) guidelines. Patients received a preoperative injection of either 100 MBq 99mtechnetium nanocolloid on the day of surgery (4–6 h before surgery, 1-day protocol), or 240 MBq the day before surgery (20–24 h before surgery, 2-day protocol) premixed with 0.25 mg ICG (ICG Pulsion, Pulsion Medical Systems, Munich, Germany) The injection was given in four intradermal deposits around the scar tissue of the primary tumor in patients with melanoma and peritumoral in patients with sarcoma and squamous cell carcinoma. Afterward, dynamic and early plus late static lymphoscintigraphy, and in most cases SPECT–CT images, were acquired to identify the locations of SLNs on a Symbia Intevo 16 Bold SPECT scanner (Siemens Healthineers, Erlangen, Germany). SLN was defined as the first lymph nodes on a direct lymphatic drainage pathway from the injection site. It is important to note that this is not always just one SLN. The tumor could drain on several SLNs at the same time. The location of the SLN was verified using a handheld probe and marked on the skin using a non-fluorescent marker.
Surgical Procedure
Preoperatively, the near-infrared (NIR) fluorescence camera (Quest Spectrum 2.0, Quest Medical Imaging, the Netherlands) was used to investigate whether the SLN was detectable transcutaneously. During the operation, detection of SLNs was first assessed using a near-infrared (NIR) fluorescence camera, after which the handheld gamma probe (EuroProbe 3.2; PI-Medical, the Netherlands) was used for radioactive detection of SLNs. All lights in the operating room were dimmed and windows closed when acquiring the fluorescent images to reduce background signal. NIR images were taken with different exposure times (auto exposure, 25 ms, 50 ms, 100 ms) to capture the most optimal TBR. The wound bed was controlled for residual fluorescent or radioactive signal after SLN excision according to the same procedure as described for SLN detection. If residual signal was present, the surgeon searched for a second SLN. If no SLN could be detected by use of the gamma probe and NIR fluorescence camera, the surgeon could opt for the additional use of a peritumoral injection with blue dye.
Postoperative Analysis
NIR fluorescence and radioactivity of the excised lymph nodes was confirmed on the back table in a black box using the same detection systems as during the operation. Fluorescence was quantified by tumor-to-background ratio (TBR) using Quest Spectrum TBR tool and surgeons evaluated the use of ICG using a standardized questionnaire (Table 2).
Pathological Evaluation
The resected lymph nodes were routinely analyzed by histopathological frozen section analysis. SLNs were fixed and embedded in formalin and paraffin for hematoxylin, eosin, and immunopathological staining at multiple levels according to the national protocol.
Results
Pre- and Intraoperative Results
In 10/15 patients (67%), some or all SLNs were already visible transcutaneously (Table 1). A total of 35 SLNs were identified on preoperative imaging, including both lymphoscintigraphy and SPECT–CT. In three patients, SLNs were identified in two nodal basins, and it was decided to only remove the inguinal and axillary SLNs since only these would influence adjuvant treatment decisions. Thus, 32 out of these 35 preoperatively identified SLNs were intraoperatively assessed. A total of 29/32 (91%) were detected with fluorescence, while 31/32 (97%) could be detected on the basis of radioactivity. One SLN could not be identified intraoperatively. SLNs that were only detected with radioactivity had a low fluorescent signal as measured ex vivo in the black box, which was not sufficient to be visible against the background in vivo. However, ex vivo these SLNs were mildly or clearly fluorescent (TBR ex vivo 3.4 and 27.4, respectively). In one patient with one SLN in the elbow and two in the axilla on preoperative imaging, only two SLN could be found, one in the elbow and one in the axilla.
Next to the 31/35 preoperatively identified SLNs that were detected during surgery, 6 additional SLNs in five patients were identified (all were both fluorescent and radioactive). The additional six SLNs were probably not detected preoperatively since they were in close contact with each other. For patients three and six, the additional SLNs were already visible transcutaneoulsy with ICG. The additional SLNs of patients six and seven were close to the tumor, which complicated pre- and intraoperative radioactive detection because of the high signal in the injection site. This led to a total of 37 intraoperatively detected SLNs. Of these, 35 (95%) were fluorescent and 37 (100%) were radioactive. Importantly, no adverse events occurred.
Histopathological Findings and Postoperative Analyses
Two patients (no. 10 and 12) were diagnosed with metastases in their SLN. Two patients (no. 4 and 15) had micrometastases.
We started with both a 1 or 2 day protocol for tracer injection, based on the standard-of-care 99mtechnetium nanocolloid injections. Initially, we did not expect any differences between these protocols, but after two 1-day cases, we felt that fluorescence was more apparent when using this protocol. Therefore, we performed the remaining procedures with the 1-day protocol.
All excised SLNs were fluorescent ex vivo. Ex vivo analysis showed a median TBR of 54.9 [interquartile range (IQR) 60.9; Fig. 1]. The median in vivo TBR was 6.5 (IQR 5.3) and the transcutaneous median TBR 2.0 (IQR 3.1). Images of the same SLN were made with four different exposure times. This led to four TBRs for the same SLN. In all cases, the most optimal TBR was selected for postoperative analysis. This TBR was usually based on the image generated with an exposure time of 25 ms. During surgery, the exposure time that revealed the best intraoperative image was used, which was usually the autoexposure (38 msec).
The surgical evaluation showed that ICG assisted in SLN detection, although its extent was dependent on the anatomical location of SLN. Surgeons evaluated ICG as easy to use and preferred it over blue dye. They would recommend ICG for the SNP to their colleagues and patients (Table 2).
Discussion
We showed that ICG–TC can be used for visual detection of SLN in pediatric patients. It showed an accurate detection rate of 100%, meaning that in every patient at least one SLN was detected with fluorescence. Furthermore, 91% of the preoperatively detected SLNs and 95% of the intraoperatively detected SLNs was fluorescent. Finally, no adverse events occurred.
This is the first time that the use of ICG has been investigated for the SNP in pediatric patients. Our results in terms of detection rate and occurrence of adverse events are in line with the results in adult studies.6,9,10,11,12,13,14,15,16 These studies concerned adult patients with melanoma, but the SNP can also be of use in pediatric patients with sarcoma and squamous cell carcinoma.1,17 Our identified transcutaneous detection rate of 67% was higher compared with adult studies that ranged between 21 and 63%,10,14,15 most likely due to the amount of subcutaneous adipose tissue.14 Some adult studies also compared the use of ICG as visual tracer with blue dye. They all identified a higher detection rate of ICG.6,9,10,11,12,13,15 We did not compare ICG directly with blue dye. Nevertheless, we gave the surgeons the option to use blue dye if they expected ICG to be insufficient, which proved to be unnecessary.
The current study method was designed to investigate the feasibility of using ICG for visual detection of SLN in addition to 99mtechnetium nanocolloid in pediatric patients. ICG was therefore coupled with 99mtechnetium nanocolloid, resulting in the fact that we cannot draw conclusions on ICG or 99mtechnetium nanocolloid alone. Nonetheless, we chose this study design because we believe that ICG can be of additive value to a radiocolloid, but is not its replacement.15,18,19,20 99mtechnetium nanocolloid is known to stain the SLN, so an advantage of ICG coupled with 99mtechnetium nanocolloid is that they both stain the SLN. Uncoupled ICG, however, travels easily to subsequent lymph nodes, increasing the chance of missing the SLN and unnecessary removal of non-SLNs.14,21 Perfect timing of the LN visualization is therefore crucial when ICG alone is used. On the other side, a potential downside of 99mtechnetium nanocolloid, and therefore also of ICG–TC, is that it might not be able to stain lymphatics and SLNs that are obstructed by tumor because of its molecular size.22,23 However, obviously involved nodes on preoperative imaging are often a contraindication to performing a SNP, or they are resected in addition to the SNP.
On the basis of this feasibility study, we expect that ICG as addition to 99mtechnetium nanocolloid could potentially lead to an improved detection rate, which could reduce false negatives, thereby further improving the diagnostic value of the SNP. The systematic review of Lafreniere et al. showed that ICG contributed to the identification of 2% of the total number of SLNs harvested.19 We noted that in five cases, the use of ICG led to the identification of six additional SLNs in total that would not have been identified with 99mtechnetium nanocolloid alone because they were either in close proximity to each other or to the injection site, causing disturbance of the radioactive signal. Furthermore, three of our four cases with metastatic disease had SLNs that were both detected preoperatively and intraoperatively. In the fourth case, an additional SLN was found next to the two preoperatively identified SLNs. However, we do not know whether the metastatic SLN was seen on the preoperative images.
The additive value of ICG for the SNP will also depend on the anatomical location of the SLN. We noted that ICG is more of value in the inguinal area and in transit sites compared with the axilla, probably due to the amount of adipose tissue covering the SLN in combination with the maximum depth penetration of ICG. This was also noted by Namikawa et al., who showed that a higher BMI and the axillary node field were factors predicting SLN detection failure.14 In addition, the head and neck area, which is known to be a difficult area for SLN harvesting, may benefit relatively more from ICG.19,20,24 SLNs in this area are often bilateral, located in multiple LN basins and with many LNs clustered together.25,26 Additionally, the primary tumor is often in close proximity, disturbing the radioactive signal. Nevertheless, the advantage of 99mtechnetium nanocolloid is the preoperative SLN localization, which may be bilateral. Therefore, a combination of ICG–TC again seems to be most optimal.
Next to improving the detection rate, ICG could, in cases of transcutaneous visibility, allow for a smaller incision and a more selective dissection with limited disruption of the lymphatics. This has the potential to reduce morbidity at the operation site, which was already shown by Korn et al., who needed less drains postoperatively.13 Additionally, the improved SLN visualization by use of ICG might reduce operating time,13 but this is probably also dependent on the anatomical location of the SLN. In this study we have not measured operating time. ICG could also potentially improve the flow of the surgery, since the camera could be placed in a position that allows for continuous visualization. However, in this situation only the camera’s light source can be used for surgery, as other light sources in the operating theater contain NIR light that disturbs the fluorescence signal.
Introducing a novel tool in the operation room is only valuable if surgeons are convinced of the added value. We used questionnaires that gave insight into the perspective of the surgeons on fluorescence for the SNP. Overall, they were positive with regard to the visual guidance of ICG in SLN detection and they would recommend the use of ICG to their colleagues and patients. The answers given in the questionnaire, as well as the SLN detection, could have been influenced by the fact that adaptation to a novel technique and learning curve could differ per surgeon. In this study, the use of ICG for SLN detection was new for four out of five surgeons. Nevertheless, all surgeons preferred the use of ICG over blue dye and they were able to identify fluorescent SLNs in all cases.
It should be clear that this study concerns small patient numbers, as it is a feasibility study. However, our identified detection rate of ICG-TC is promising and in line with detection rates of 99mtechnetium nanocolloid reported in literature. Currently, we cannot conclude whether this method improves the diagnostic accuracy of the SNP, and/or influences the surgery time, complication rate, and facilitation of the operation. There are also some general limitations when using fluorescence. First of all, it might be necessary to disturb the surgical procedure when the lights have to be turned off and the camera positioned. As already mentioned, fluorescence has a maximum depth penetration leading to reduced utility for deeper-lying SLNs. Finally, ICG cannot be used to localize SLN with preoperative imaging.
Altoghether, we expect that ICG–TC is the best tracer to use for the SNP. Larger, well-designed studies are needed to investigate the implications of fluorescence as an addition to 99mtechnetium nanocolloid on the SNP diagnostic accuracy by measuring the false negative rates. Its implications for facilitating surgery, reducing surgery time, and reducing the number of complications should also be explored.
However, there are institutes in which radioactive tracers are not available. In these institutes, blue dyes are most commonly used. Adult studies indicate that ICG alone performs better than blue dye,6,9,10,11,12,13,15 so a well-designed study to compare the use of ICG with blue dye in pediatric patients is needed. It can be hypothesized that ICG performs even better in this patient population since skin thickness and average BMI of pediatric patients is often lower compared with adult patients. Yet, for these institutes it might be wise to combine ICG with blue dye in cases with a high BMI and/or axillary node field, since these are factors predicting SLN detection failure with ICG. This should be decided preoperatively, as the lymphatics may have been disrupted if the procedure has already started.
In conclusion, ICG–TC for the SNP is a feasible procedure in pediatric patients. It showed an accurate detection rate, was helpful for visual guidance, and did not lead to tattooing or any other adverse events.
References
Parida L, Morrisson GT, Shammas A, et al. Role of Lymphoscintigraphy and Sentinel Lymph Node Biopsy in the Management of Pediatric Melanoma and Sarcoma. Pediatr Surg Int. 2012;28(6):571–8. https://doi.org/10.1007/s00383-012-3066.
Jeremiasse B, van den Bosch CH, Wijnen MWHA, Terwisscha van Scheltinga CEJ, Fiocco MF, van der Steeg AFW. Systematic Review and Meta-Analysis Concerning Near-Infrared Imaging with Fluorescent Agents to Identify the Sentinel Lymph Node in Oncology Patients. Eur J Surg Oncol. 2020;46(11):2011–22. https://doi.org/10.1016/j.ejso.2020.07.012.
Cimmino VM, Brown AC, Szocik JF, et al. Allergic Reactions to Isosulfan Blue During Sentinel Node Biopsy - A Common Event. Surgery. 2001;130(3):439–42. https://doi.org/10.1067/msy.2001.116407.
Govaert GAM, Oostenbroek RJ, Plaisier PW. Prolonged Skin Staining After Intradermal Use of Patent Blue in Sentinel Lymph Node Biopsy for Breast Cancer. Eur J Surg Oncol. 2005;31(4):373–5. https://doi.org/10.1016/j.ejso.2004.12.009.
Mertes PM, Malinovsky JM, Mouton-Faivre C, et al. Anaphylaxis to Dyes During the Perioperative Period: Reports of 14 Clinical Cases. J Allergy Clin Immunol. 2008;122(2):348–52. https://doi.org/10.1016/j.jaci.2008.04.040.
Van Den Berg NS, Brouwer OR, Schaafsma BE, et al. Multimodal Surgical Guidance During Sentinel Node Biopsy for Melanoma: Combined Gamma Tracing and Fluorescence Imaging of the Sentinel Node Through Use of the Hybrid Tracer Indocyanine Green-99mTc-Nanocolloid. Radiology. 2015;275(2):521–9. https://doi.org/10.1148/radiol.14140322.
FDA. Product Information: IC-GREEN(R) intravenous injection, indocyanine green intravenous injection. Prod. Inf. 201AD. https://www.accessdata.fda.gov/drugsatfda_docs/label/2006/011525s017lbl.pdf
Neves RI, Reynolds BQ, Hazard SW, Saunders B, Mackay DR. Increased Post-Operative Complications with Methylene Blue Versus Lymphazurin in Sentinel Lymph Node Biopsies for Skin Cancers. J Surg Oncol. 2011;103(5):421–5. https://doi.org/10.1002/jso.21845.
Brouwer OR, Klop WMC, Buckle T, et al. Feasibility of Sentinel Node Biopsy in Head and Neck Melanoma Using a Hybrid Radioactive and Fluorescent Tracer. Ann Surg Oncol. 2012;19(6):1988–94. https://doi.org/10.1245/s10434-011-2180-7.
Pameijer CR, Leung A, Neves RI, Zhu J. Indocyanine Green and Fluorescence Lymphangiography for Sentinel Node Identification in Patients with Melanoma. Am J Surg. 2018;216(3):558–61. https://doi.org/10.1016/j.amjsurg.2018.01.009.
Cloyd JM, Wapnir IL, Read BM, Swetter S, Greco RS. Indocyanine Green and Fluorescence Lymphangiography for Sentinel Lymph Node Identification in Cutaneous Melanoma. J Surg Oncol. 2014;110(7):888–92. https://doi.org/10.1002/jso.23745.
Knackstedt R, Couto RA, Ko J, Cakmakoglu C, Wu D, Gastman B. Indocyanine Green Fluorescence Imaging with Lymphoscintigraphy for Sentinel Node Biopsy in Melanoma: Increasing the Sentinel Lymph Node-Positive Rate. Ann Surg Oncol. 2019;26(11):3550–60. https://doi.org/10.1245/s10434-019-07617-z.
Korn JM, Tellez-Diaz A, Bartz-Kurycki M, Gastman B. Indocyanine Green SPY Elite-Assisted Sentinel Lymph Node Biopsy in Cutaneous Melanoma. Plast Reconstr Surg. 2014;133(4):914–22. https://doi.org/10.1097/PRS.0000000000000006.
Namikawa K, Tsutsumida A, Tanaka R, Kato J, Yamazaki N. Limitation of Indocyanine Green Fluorescence in Identifying Sentinel Lymph Node Prior to Skin Incision in Cutaneous Melanoma. Int J Clin Oncol. 2014;19(1):198–203. https://doi.org/10.1007/s10147-013-0524-y.
Stoffels I, Dissemond J, Pöppel T, Schadendorf D, Klode J. Intraoperative Fluorescence Imaging for Sentinel Lymph Node Detection: Prospective Clinical Trial to Compare the Usefulness of Indocyanine Green vs Technetium Tc 99m for Identification of Sentinel Lymph Nodes. JAMA Surg. 2015;150(7):617–23. https://doi.org/10.1001/jamasurg.2014.3502.
Knackstedt RW, Couto RA, Gastman B. Indocyanine Green Fluorescence Imaging with Lymphoscintigraphy for Sentinel Node Biopsy in Head and Neck Melanoma. J Surg Res. 2018;228:77–83. https://doi.org/10.1016/j.jss.2018.02.064.
Jeremiasse B, van der Steeg AFW, Fiocco M, et al. Value of the Sentinel Node Procedure in Pediatric Extremity Rhabdomyosarcoma: A Systematic Review and Retrospective Cohort Study. Ann Surg Oncol. 2021;28(13):9048–59. https://doi.org/10.1245/s10434-021-10035-9.
de Carvalho CEB, Capuzzo R, Crovador C, et al. Near Infrared (NIR) Fluorescence is not a Substitute for Lymphoscintigraphy and Gamma Probe for Melanoma Sentinel Node Detection: Results from a Prospective Trial. Ann Surg Oncol. 2020;27(8):2906–12. https://doi.org/10.1245/s10434-020-08409-6.
Lafreniere AS, Shine JJ, Nicholas CR, Temple-Oberle CF. The Use of Indocyanine Green and Near-Infrared Fluorescence Imaging to Assist Sentinel Lymph Node Biopsy in Cutaneous Melanoma: A Systematic Review. Eur J Surg Oncol. 2021;47(5):935–41. https://doi.org/10.1016/j.ejso.2020.10.027.
Patel N, Allen M, Arianpour K, Keidan R. The Utility of ICG Fluorescence for Sentinel Lymph Node Identification in Head and Neck Melanoma. Am J Otolaryngol Head Neck Med Surg. 2021;42(5):103–47. https://doi.org/10.1016/j.amjoto.2021.103147.
Niebling MG, Pleijhuis RG, Bastiaannet E, Brouwers AH, Van Dam GM, Hoekstra HJ. A Systematic Review and Meta-Analyses of Sentinel Lymph Node Identification in Breast Cancer and Melanoma, a Plea for Tracer Mapping. Eur J Surg Oncol. 2016;42(4):466–73. https://doi.org/10.1016/j.ejso.2015.12.007.
Klode J, Poeppel T, Boy C, et al. Advantages of Preoperative Hybrid SPECT/CT in Detection of Sentinel Lymph Nodes in Cutaneous Head and Neck Malignancies. J Eur Acad Dermatology Venereol. 2011;25(10):1213–21. https://doi.org/10.1111/j.1468-3083.2010.03954.x.
Morton DL, Thompson JF, Cochran AJ, Mozzillo N, Elashoff R, Essner R. Sentinel-Node Biopsy or Nodal Observation in Melanoma. N Engl J Med. 2006;355(13):1307–17.
Norman J, Cruse CW, Espinosa C, et al. Redefinition of Cutaneous Lymphatic Drainage with the Use of Lymphoscintigraphy for Malignant Melanoma. Am J Surg. 1991;162(5):432–7. https://doi.org/10.1016/0002-9610(91)90255-C.
Alex JC, Krag DN, Harlow SP, et al. Localization of Regional Lymph Nodes in Melanomas of the Head and Neck. Arch Otolaryngol Head Neck Surg. 1998;124(2):135–40. https://doi.org/10.1001/archotol.124.2.135.
Wells KE, Rapaport DP, Cruse CW, et al. Sentinel Lymph Node Biopsy in Melanoma of the Head and Neck. Plast Reconstr Surg. 1997;100(3):591–4. https://doi.org/10.1097/00006534-199709000-00006.
Acknowledgment
We thank Ceder van den Bosch and Myrthe Buser for their valuable help in data acquisition.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
DISCLOSURE
The authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jeremiasse, B., van Scheltinga, C.E.J.T., Smeele, L.E. et al. Sentinel Lymph Node Procedure in Pediatric Patients with Melanoma, Squamous Cell Carcinoma, or Sarcoma Using Near-Infrared Fluorescence Imaging with Indocyanine Green: A Feasibility Trial. Ann Surg Oncol 30, 2391–2398 (2023). https://doi.org/10.1245/s10434-022-12978-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12978-z