Abstract
Background
Increased time to surgery (TTS) is associated with decreased survival in patients with breast cancer. In early 2020, elective surgeries were canceled to preserve resources for patients with coronavirus disease 2019 (COVID-19). This study attempts to measure the effect of mandated operating room shutdowns on TTS in patients with breast cancer.
Patients and Methods
This multicenter retrospective study compares 51 patients diagnosed with breast cancer at four public hospitals from January to June 2020 with 353 patients diagnosed from January 2017 to June 2018. Demographics, tumor characteristics, treatment regimens, and TTS for patients were statistically compared using parametric, nonparametric, and Cox proportional hazards regression modeling.
Results
Across all centers, there was a non-statistically significant increase in median TTS from 59 days in the pre-COVID period to 65 days during COVID (p = 0.9). There was, however, meaningful variation across centers. At center A, the median TTS decreased from 57 to 51 days, center C’s TTS decreased from 83 to 64 days, and in center D, TTS increased from 42 to 129 days. In a multivariable Cox proportional hazards model for the pre-COVID versus COVID period effect on TTS, center was an important confounding variable, with notable differences for centers C and D compared with the referent category of center A (p = 0.04, p = 0.006).
Conclusion
Data suggest that, while mandated operating room shutdowns did not result in an overall statistically significant delay in TTS, there were important differences between centers, indicating that, even in a unified multicenter public hospital system, COVID-19 may have resulted in delayed and potentially disparate care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
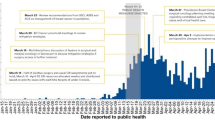
In March 2020, New York City became the first American epicenter of the COVID-19 pandemic. It has been documented that, from March to May 2020, 203,000 confirmed COVID-19 cases were documented by the New York City Department of Health and Mental Hygiene.1 Of these, 18,679 patients, or 9.2% of patients with positive COVID-19 tests reported, died, resulting in a death rate of 198 deaths per 100,000 people in New York City’s population.1 To combat this death rate, hospitals were converted into large-capacity intensive care units (ICUs) to manage the influx of critically ill patients with COVID-19.
On 12 March 2020, New York City mandated that all elective surgeries be postponed to preserve resources, mainly ventilators, for patients with COVID-19. Patients with breast cancer requiring disease-slowing and curative procedures faced a unique conundrum in that their surgeries, though necessary and lifesaving, were not deemed emergent and became susceptible to postponement through this mandate. Despite multiple studies demonstrating that prolonged time to surgery in patients with breast cancer is associated with decreased survival,2 when the COVID-19 pandemic struck New York City and elective surgeries were canceled to preserve ventilators, staff, and ICU capacity for patients with COVID-19, patients with breast cancer soon faced the brunt of these limitations.
Since March 2020, there have many more large spikes in COVID cases and mortalities attributed to new variants of the virus: Delta and Omicron. In early December 2021, cases began to surge, increasing from approximately 100,000 new cases per day in the USA to over 400,000 new daily cases.3,4 New York again declared a state of emergency with the mandate that, if necessary, nonessential procedures would be shut down to conserve resources for the treatment of the increased patients with COVID-19.5 As many scientists agree, there will likely be more variants to come with the potential for further operating room shutdowns. This study attempts to elucidate the effect of the mandatory operating room shutdown due to the COVID-19 pandemic throughout the spring of 2020 on time to surgery in patients with breast cancer.
Patients and Methods
This is a retrospective cohort study of patients identified from a multicenter tumor registry and chart review. This study was approved by the institutional review board (IRB) and carried out in accordance with the approved guidelines. Fifty-one patients diagnosed with breast cancer via biopsy at four New York City public hospitals from 1 January to 30 June 2020 were included in this study as the COVID cohort. This cohort was compared with patients with breast cancer diagnosed at the same four public hospitals from 1 January to 30 June 2017, and 1 January to 30 June 2018, n = 353. All COVID cohort patient data were collected in real time by the breast cancer teams at each study center, recorded into the Health Insurance Portability and Accountability Act (HIPAA) compliant REDCap portal, and then analyzed using R statistical software. Pre-COVID, control, and cohort data were collected using an IRB-approved chart review.
All patients with a new breast cancer diagnosis confirmed by biopsy at a study center from 1 January to 30 June 2017, 2018, or 2020 were eligible for inclusion. Patients who discontinued care at a study center were removed from subsequent study, including patients who refused treatment, were lost to follow-up, or transferred their oncologic and surgical care to another hospital. Patients diagnosed at nonstudy centers and later referred for care at a study center were also removed. Patients diagnosed outside of New York State who then moved to New York to seek care were also excluded from the study. Patients who received neoadjuvant therapy were not included in the calculation of time to surgery unless their neoadjuvant therapy was explicitly initiated due to a COVID delay of primary surgery. Neoadjuvant therapy consists of chemotherapy and/or endocrine therapy initiated prior to surgery. American Joint Committee on Cancer (AJCC) pathologic and clinical tissue (T) and node (N) staging was used to characterize tumors of each patient with cancer included in the study. AJCC mastectomy staging was not included because this information was not yet available for the COVID cohort.
The analysis consisted of overall comparisons of patient demographics, treatment regimens, and time to surgery in patients diagnosed with breast cancer between 2017 and 2018, pre-COVID-19, versus patients diagnosed with breast cancer during the COVID-19 pandemic at four New York City public hospitals. Demographics, tumor characteristics, treatments received, and time to surgery for patients were compared between the two cohorts using chi-squared tests for categorical variables and t-tests for continuous variables. Age was broken down by decade to further deidentify data and remain compliant with IRB protocols with RedCap. All analyses were conducted in the R statistical software system.6 Time to surgery was compared for the pre-COVID cohort versus the COVID cohort with Kaplan–Meier curves and Cox proportional hazards methods to model the effect of the COVID time period on time to surgery. Both a simple, dichotomous regression estimating the effect of COVID on the pre-COVID and COVID cohorts as well as a multivariate Cox proportional hazards model controlling for age, race, and facility were used to model the effect of COVID on time to surgery. Time to surgery was calculated as the time in days from the day of diagnosis via biopsy to the day of surgery.
Results
A total of 51 patients met inclusion criteria and were enrolled in the COVID cohort. The most common age group (33.3%) of the COVID cohort was 51–60 years old, the largest ethnic racial group was Hispanic or Latino (39.2%), and all were female (Table 1). In total, 353 female patients were included in the pre-COVID cohort; the largest age category was 51–60 years (28.9%), and the most common ethnic racial groups were other/unknown (35.1%) and Black (30.3%) (Table 1).
As presented in Table 2, treatment regimens of patients in the pre-COVID cohort and the COVID cohort varied. Number of lumpectomies increased from 39.5% of breast surgeries in the pre-COVID cohort to 49.0% of breast surgeries in the COVID cohort (p = 0.011). Similarly, in the pre-COVID cohort, simple mastectomies accounted for only 23.5% of the breast surgeries, increasing to 32.7% in the COVID cohort (p = 0.011). Additionally, the neoadjuvant chemotherapy regimen was altered due to COVID in 34.8% of the COVID cohort patients (95% CI 18.7–45.6) and increased from 19.8% in the pre-COVID cohort to 47.1% in the COVID cohort (p < 0.001).
In total, 49% of the COVID cohort was treated at center A, 0% at center B, 31.4% at center C, and 19.6% at center D. For the pre-COVID cohort, 34.8% were treated at center A, 16.4% at center B, 26.1% at center C, and 22.7% at center D. The majority of pre-COVID patients treated at center A were aged 51–60 years and were other/unknown or Asian/Pacific Islander, while the majority of center A’s COVID cohort was aged 51–60 years and were Hispanic or Latino. The majority of center B’s pre-COVID patients were aged 61–70 years and were white, and there were no COVID patients at this center. The majority of center C’s pre-COVID patients were 51–60 years and Black, while the majority of the COVID cohort was aged 51–60 years and Hispanic or Latino. Finally, the majority of center D’s pre-COVID cohort was aged 51–60 years and Black, while the COVID cohort mainly was 61–80 years and Black (Table 4).
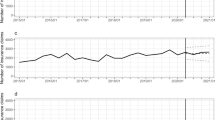
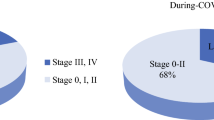
Out of 49 surgeries performed on patients with breast cancer during the pandemic, 15 were delayed because of the COVID-19 pandemic (95% CI 18.7–45.6). Across all four centers combined, the median time to surgery increased from 59 days in the pre-COVID period to 64 days during the COVID lockdown period (Fig. 1), though this result was not statistically significant (p = 0.9). When comparing tumor characteristics, pathologic and clinical stages T1 and N0 remained the most common in the pre-COVID and COVID cohorts. However, the was a significant increase in the pathologic and clinical T4 stage when comparing the pre-COVID with the COVID cohort (1.4% versus 10.4%, p < 0.001) (Table 3).
Kaplan–Meier curve comparing pre-COVID cohort (blue) with COVID cohort (red). Median time to surgery for the pre-COVID cohort of all centers combined was 59 (95% CI 55–66) days compared with 65 (95% CI 55–129) days for the COVID cohort. There is no statistical significance in the differences of time to surgery between the two cohorts on the basis of a log-rank test (p = 0.9)
Time to surgery differed by study center. At center A, the median time to surgery decreased from 57 to 51 days, center C’s time to surgery decreased from 83 to 64 days, and at center D, time to surgery increased from 42 to 129 days (Table 4). Center A experienced a 79.7% decrease in cases during the pandemic compared with center B’s 100% decrease, center C’s 82.6% decrease, and center D’s 87.5% decrease. In a multivariable Cox proportional hazards model for the effect of pre-COVID versus COVID period on time to surgery, center was an important confounding variable, with notable differences for centers C and D compared with the referent category of center A (Table 6).
Not only did the change in median time to surgery vary between study centers, but the impact of the COVID-19 pandemic and the operating shutdown also impacted treatment regimens differently across the centers (Table 5). At centers A and B, the percentage of lumpectomies increased compared with the pre-COVID cohort. At center A, the percentage of modified radical mastectomies increased in the COVID cohort compared with the pre-COVID cohort, while the percentage of simple mastectomies decreased compared with the pre-COVID cohort. The opposite trend was seen at centers C and D, where the percentage of modified radical mastectomies decreased and the percentage of simple mastectomies increased when comparing the COVID cohort with the pre-COVID cohort. At center A, the use of neoadjuvant therapy increased from 23.5% to 40%, center C experienced an increase from 23.0% to 50.0%, and at center D neoadjuvant therapy use increased from 6.5% to 60.0% (Table 5). Finally, at centers A and C, the percentage of patients who did not undergo reconstruction increased in the COVID cohort.
Discussion
It is widely known that increased time to surgery increases patient mortality in patients with breast cancer.2,7 Thus, there was great concern about potentially increased mortality in patients with breast cancer during the government-mandated operating room shutdown in spring 2020. Our multicenter analysis found that, when combining data across four different public hospitals, the 2020 COVID-19 pandemic and operating room shutdown were not associated with statistically significant delays in surgery for patients with breast cancer, as measured through a simple dichotomous Cox proportional hazard model. This statistical result should be approached with caution, as patients at centers B and D did experience meaningful delays in their time to surgery, and it may mask potential disparities present within individual hospitals.
The multivariable Cox proportional hazards model (Table 6), which included hospital center as a potentially confounding variable, indicated clinically significant heterogeneity within the united New York City public hospital system and potential disparities in patient care between different New York City public hospitals. The difference, and potential disparity, between the different public hospitals are largely due to size and resources prior to COVID. While some of these centers have only one breast surgeon to care for their patients with breast cancer, others have an entire multidisciplinary team of breast surgeons, plastic surgeons, and genetic counselors to care for them. Additionally, smaller hospitals have fewer operating rooms, thus these centers and their patients are more affected by a reduced operating room capacity.
Two of the hospitals, center A and C, even had improved time to surgery during the COVID-19 pandemic. This decreased time to surgery highlights the impact that more resources prior to the start of the pandemic, including a surgical team with multiple surgeons, allowed these hospitals to strictly adhere to the American College of Surgery (ACS) COVID-19 Guidelines for Triage of Breast Cancer Patients and triage patients for surgery quickly.8 In accordance with these guidelines, only patients who met ACS surgical criteria were promptly scheduled for surgery, while all others were referred back to their medical oncologists for possible initiation of neoadjuvant chemotherapy and/or endocrine therapy as they waited for their surgery. This is demonstrated by the decreased time to surgery seen at some of the study centers, as well as the increase in neoadjuvant therapy in the COVID cohort compared with the pre-COVID cohort, as surgical patients were able to be “fast-tracked” to an OR date.
Moreover, the type of surgery performed was adjusted using a multidisciplinary approach between breast surgeons and plastic surgeons to minimize patient admission times. For example, the number of lumpectomies increased while the number of modified radical mastectomies, a much more invasive procedure often requiring multiday hospital admissions, decreased (Tables 2 and 5). Furthermore, reconstruction was often delayed so that patients could be discharged after their mastectomies. To illustrate, at center A, the center with the highest number of reconstructions prior to the pandemic, 75% of patients in the COVID-19 cohort did not receive reconstruction after their surgery.
It has been widely documented that there are disparities present in the care of patients with COVID-19 and that both Black and Hispanic patients have a higher incidence of infection and increased mortality.9,10,11,12 Moreover, due to a multitude of reasons such as lack of access, insurance, and socioeconomic status, underrepresented patients with breast cancer diagnoses are more commonly diagnosed at more aggressive cancer stages and face increased mortality rates compared with insured white patients with breast cancer.13,14,15,16,17,18 These patients often receive care at smaller public hospitals, which have fewer resources than larger public hospitals and private hospitals. Thus, the significant difference between New York City public hospitals and time to surgery in our analysis serves as a call to action to ensure that all public hospitals, no matter their size or location, should be given adequate resources to ensure their ability to safely provide care for their particularly vulnerable patients.
There are multiple limitations to this study. First, to highlight the effect of the operating room shutdown, only data from January to June 2020 were included, resulting in a very small number of patients in the COVID-19 cohort. Secondly, one of the hospital centers, center B, could not accommodate any non-COVID19 patients, and therefore they did not treat or diagnose any patient with breast cancer from January to June 2020, inhibiting the computation of p-values in the descriptive statistics analyses. Third, given the relatively small number of cases during the COVID period, our study is likely underpowered to demonstrate statistically significant differences that may be present.
Conclusions
Though the long-term effects of the operating room shutdown due to the initial surge of COVID-19 cases in 2020 remain unknown, this study suggests that the operating room shutdown was not associated with an overall significant increase in time to surgery across four New York City public hospitals. However, when individual centers were taken into consideration, there were apparent significant differences in time to surgery, which illustrate potential disparities in the care of breast cancer during the COVID-19 lockdown period.
References
Thompson CN BJ, Pichardo C, et al. COVID-19 Outbreak—New York City, February 29–June 1, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1725–1729. DOI: https://doi.org/10.15585/mmwr.mm6946a2.
Bleicher RJ, Ruth K, Sigurdson ER, et al. Time to surgery and breast cancer survival in the United States. JAMA Oncol. 2016;2(3):330–9.
Johns Hopkins Coronavirus Resource Center. Covid-19 United States Cases by country. Available at: https://coronavirus.jhu.edu/us-map. Accessed on 29 December 2021.
Singhal T. The Emergence of Omicron: challenging times are here again! [published online ahead of print, 13 January 2022]. Indian J Pediatr. 2022;1–7. doi: https://doi.org/10.1007/s12098-022-04077-4
New York Declares State of Emergency Amid Variant Threat [press release]. Bloomberg.com, 26 November 2021.
R Core Team (2021). R: a language and environment for statistical computing. R foundation for statistical computing, Vienna, Austria. URL https://www.R-project.org/.
Waks AG, King TA, Winer EP. Timeliness in breast cancer treatment—the sooner, the better. JAMA Oncol. 2016;2(3):302–4.
COVID-19 guidelines for triage of breast cancer patients. https://www.facs.org/covid-19/clinical-guidance/elective-case/breast-cancer. Published 2020. Updated 07 May 2020. Accessed 01 February 2022.
Mackey K, Ayers CK, Kondo KK, et al. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: a systematic review. Ann Intern Med. 2021;174(3):362–73. https://doi.org/10.7326/M20-6306.
Feldman JM, Bassett MT. Variation in COVID-19 Mortality in the US by race and ethnicity and educational attainment. JAMA Netw Open. 2021;4(11):e2135967. Published 1 Nov 2021. doi:https://doi.org/10.1001/jamanetworkopen.2021.35967
Wadhera RK, Wadhera P, Gaba P, et al. Variation in COVID-19 hospitalizations and deaths across New York City Boroughs. JAMA. 2020.
Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020.
Babatunde OA, Eberth JM, Felder T, et al. Social determinants of racial disparities in breast cancer mortality among Black and white women. J Racial Ethn Health Disparities. 2020.
Coburn N, Fulton J, Pearlman DN, Law C, DiPaolo B, Cady B. Treatment variation by insurance status for breast cancer patients. Breast J. 2008;14(2):128–34.
Elmore JG, Nakano CY, Linden HM, Reisch LM, Ayanian JZ, Larson EB. Racial inequities in the timing of breast cancer detection, diagnosis, and initiation of treatment. Medical Care. 2005;43(2):141–8.
Lovejoy LA, Eaglehouse YL, Hueman MT, Mostoller BJ, Shriver CD, Ellsworth RE. Evaluation of surgical disparities between African American and European American women treated for breast cancer within an equal-access military hospital. Ann Surg Oncol. 2019;26(12):3838–45.
Pocock B, Nash S, Klein L, El-Tamer M, Schnabel FR, Joseph KA. Disparities in time to definitive surgical treatment between Black and White women diagnosed with ductal carcinoma in situ. Am J Surg. 2007;194(4):521–3.
Smith ER, Adams SA, Das IP, Bottai M, Fulton J, Hebert JR. Breast cancer survival among economically disadvantaged women: the influences of delayed diagnosis and treatment on mortality. Cancer Epidemiol Biomarkers Prev. 2008;17(10):2882.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Escobar, N., DiMaggio, C., Pocock, B. et al. Effects of COVID-19 on Surgical Delays in Patients with Breast Cancer in NYC Public Hospitals: A Multicenter Study. Ann Surg Oncol 30, 23–30 (2023). https://doi.org/10.1245/s10434-022-12491-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12491-3