Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic increased the use of telehealth within medicine. Data on sociodemographic and clinical characteristics associated with telehealth utilization among cancer surgical patients have not been well-defined.
Methods
Cancer patients who had a surgical oncology visit at the James Cancer Hospital in March 2020–May 2021 were included. Patient demographic and clinical characteristics were recorded; access to modern information technology was measured using the Digital Divide Index (DDI). A logistic regression model was used to assess odds of receiving a telehealth.
Results
Among 2942 patients, median DDI was 18.2 (interquartile range 17.4–22.1). Patients were most often insured through managed care (n = 1459, 49.6%), followed by Medicare (n = 1109, 37.7%) and Medicaid (n = 267, 9.1%). Overall, 722 patients (24.5%) received at least one telehealth visit over the study period. On multivariable analysis, age (odds ratio [OR] 0.89, 95% confidence interval [CI] 0.80–0.98 per 10-year increase), sex (male vs. female: OR 1.83, 95% CI 1.45–2.32), cancer type (pancreatic vs. breast: OR 9.19, 95% CI 6.38–13.23; colorectal vs. breast: OR 5.31, 95% CI 3.71–7.58), insurance type (Medicare vs. Medicaid: OR 1.58, 95% CI 1.04–2.41) and county of residence (distant vs. neighboring: OR 1.33, 95% CI 1.06–1.66) were associated with increased odds of receiving a telehealth visit. Patients from high DDI counties were not less likely to receive telehealth visits versus patients from low DDI counties (OR 1.15, 95% CI 0.85–1.57).
Conclusions
Several patient sociodemographic and clinical characteristics had an impact on the likelihood of receiving a telehealth visit versus an in-person visit, suggesting that telehealth may not be equally accessible to all surgical oncology patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has had a dramatic impact on health care delivery, causing a surge in the utilization of telehealth services.1 Telemedicine has been touted as a way to minimize patient exposure to the pandemic without compromising care. In turn, regulatory agencies have facilitated the increased implementation of telehealth during the ongoing public health crisis.2,3,4 As a result, the weekly number of Medicare beneficiaries who received telehealth services skyrocketed from approximately 13,000 prior to the pandemic to nearly 1.7 million in April 2020.5 While the sudden increase in telemedicine utilization was a response to the COVID-19 outbreak, it has reshaped the US health care delivery systems in ways that are likely to have lingering effects long after the ongoing pandemic has waned.6 In fact, some temporary measures implemented to broaden the accessibility of telehealth by the Centers of Medicare and Medicaid Services have since become permanent.7
The expansion of telehealth services has involved multiple surgical specialties, which have traditionally been reluctant to adopt newer information technology in health care delivery.8 While examples of the use of telemedicine in pre- and postoperative care prior to the COVID-19 pandemic exist, data on this topic have been sparce.9,10 The implementation of telemedicine in surgical care may offer several potential advantages, especially within the context of surgical oncology. For example, surgical oncology patients have been reported to have a higher likelihood of optimal outcomes when treated at high-volume centers.11,12,13 However, the resulting regionalization of surgical cancer care to large, high-volume hospitals often requires patients to travel longer distances to obtain high-quality care.14 Telemedicine holds the promise of allowing high-volume centers to more easily evaluate and follow-up with patients from distant areas, thus avoiding fragmentation of postoperative care.15
The ability of telehealth services to reach certain populations of patients, including individuals from rural and socially disadvantaged areas, has however been a growing concern.16,17 In particular, the impact of the digital divide on the ability to access telehealth services has been a topic of interest.18,19 The digital divide is defined as the gap between populations and regions that have access to modern information technology and those individuals who do not. The potential role of the digital divide to perpetuate health inequities has caused the American Medical Informatics Association to call for its inclusion as a social determinant of health.20 However, little is known about the effect of the digital divide on the ability of surgical oncology patients to access telehealth services. Therefore, the objective of the current study was to define the impact of sociodemographic and clinical characteristics relative to utilization of telehealth visits among cancer patients at a large comprehensive cancer center. In particular, the effect of the digital divide on the likelihood to access telehealth services was assessed.
Methods
Patient Population
All cancer patients who had a date of first contact with the Ohio State University Wexner Medical Center/James Cancer Center between 1 March 2019 and 1 May 2021 were included in the initial cohort. Patients were retained in the final cohort if the individual had at least one completed encounter with a surgical oncology specialty department during the study period. The cancer diagnosis codes used to identify the patients are provided in electronic supplementary Table S1. Prisoners and patients under 18 years of age at the time of the cancer diagnosis were excluded per institutional policy. As telehealth visits could only be reliably identified after 16 March 2020 following changes in state regulations and coding practices, patients with no visits after this date were also excluded.21 This exclusion criterion allowed for the assessment of the outcome of interest (i.e., receipt of a telehealth visit) ensuring only patients whose telehealth visits could be reliably identified were included in the analytic cohort.
Variables, Definitions and Outcomes
Variables of interest included age, sex, race, preferred language in interactions with providers, and type of health insurance. Patient cancer type was defined as the cancer diagnosis at the time of the first surgical oncology visit during the study period. Patient ZIP code of residence was converted into county of residence using the relevant US Department of Housing and Urban Development’s ZIP code crosswalk files.22 Patients were considered to be from a neighboring county if they resided in the same county as the hospital (Franklin County, OH) or in one of the adjacent counties (Union County, Delaware County, Licking County, Fairfield County, Pickaway County, or Madison County). The county-level Digital Divide Index (DDI) was used to measure patient ease of access to modern information technology. DDI is calculated based on 10 metrics that include information on local broadband infrastructure and adoption, as well as socioeconomic factors that are known to impact technology adoption23 More specifically, the DDI is composed of two separate scores—the Infrastructure/Adoption score (IFNA) and the Socioeconomic score (SE), each ranging from 0 to 100. The IFNA is calculated based on five variables related to broadband infrastructure and adoption, namely the proportion of the population with access to fixed broadband of at least 100 Mbps download and 20 Mbps upload, the percentage of homes without a computing device, the percentage of homes without internet access, and the median advertised download and upload speeds. In contrast, SE is calculated based on five socioeconomic variables known to impact technology adoption, namely the percentage of the population 65 years of age and over, the percentage of the population 25 years of age or older with less than high school education, the individual poverty rate, the percentage of noninstitutionalized civilian population with a disability, and an internet-income ratio measure. The overall DDI ranges in value from 0 to 100, with higher values indicating lower availability of modern information technology. County-level DDI scores were categorized into low (first quartile), medium (second and third quartiles) and high (fourth quartile) for purpose of analyses. The main outcome of interest was receipt of a telehealth visit over the study period, defined as an audio-only or audio and video virtual communication between patient and provider.
Statistical Analysis
Descriptive statistics were presented as median (interquartile range [IQR]) for continuous variables and frequency (relative frequency, %) for categorical variables. Bivariate associations between patient sociodemographic and clinical characteristics and the outcome of interest were assessed using the Mann–Whitney test for continuous variables and the Chi-square test for categorical variables. A multivariable logistic regression model was developed to assess the possible association of patient characteristics with the likelihood of receiving a telehealth visit over the study period. Results were then stratified by neighboring county status. A sensitivity analysis only involving patients who had at least one visit between 1 March 2020 and 31 May 2020 to predict receipt of telehealth visits within this time frame was also performed. All analyses were performed using SPSS version 28 (IBM Corporation, Armonk, NY, USA). Statistical significance was assessed at α = 0.05.
Results
Demographic and Clinical Characteristics of the Patient Population
Among 2942 patients with a cancer diagnosis who had a surgical oncology visit during the study period, the median age was 61.0 years (IQR 51.0–69.0) and more than two-thirds were female (n = 2319, 78.8%) or White (n = 2565, 87.2%) (Table 1). Almost all patients used English as their preferred language in interactions with providers (n = 2900, 98.6%). Patients were most commonly insured through a managed care plan (n = 1459, 49.6%), followed by Medicare (n = 1109, 37.7%), and Medicaid (n = 267, 9.1%). About half of all patients resided in the same county as the hospital or in a neighboring county (n = 1458, 49.6%); the median DDI was 18.2 (IQR 17.4–22.1). Based on county-level DDI, patients were subclassified into low (n = 736, 25.0%), medium (n = 1534, 52.1%), or high (n = 669, 22.7%) DDI categories. The most common cancer diagnosis was breast cancer (n = 1509, 51.3%), followed by colorectal cancer (n = 222, 7.5%) and pancreatic cancer (n = 212, 7.2%).
Nearly one in four patients received at least one telehealth visit over the course of the study (n = 722, 24.5%). Patients who had telehealth visits were older (62.5 years vs. 61.0 years; p = 0.003) and more often male (43.9% vs. 13.8%; p < 0.001) than patients who had no telehealth visits. Additionally, patients who received telehealth visits were more likely to be insured through Medicare (42.9% vs. 36.0%) and less likely to be insured through managed care (44.6% vs. 51.2%) or Medicaid (7.8% vs. 9.5%) compared with patients who had no telehealth visits (p < 0.001). Of note, patients with at least one telehealth visit over the study period were less often residents of a neighboring county (40.0% vs. 52.7%) or residents of a county with a low (23.0% vs. 25.7%) or medium (47.2% vs. 53.7%) DDI compared with patients with no telehealth visits (p < 0.001). In addition, patients who had telehealth visits were substantially less likely to be diagnosed with breast cancer (16.8% vs. 62.5%) than patients who had no telehealth visits. In contrast, patients diagnosed with endocrine tumors (12.2% vs. 2.3%), colorectal cancer (10.9% vs. 6.4%), liver and biliary tract cancers (7.8% vs. 3.0%), lung cancer (2.6% vs. 1.3%), or cancers of the urinary tract (1.7% vs. 0.3%) were more likely to have had at least one telehealth visit (all p < 0.001).
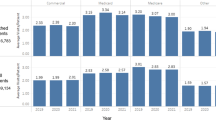
Trends in Telehealth Utilization Over Time
Following the introduction of new guidelines for the use of telehealth in March 2020, use of telehealth for surgical oncology visits at our institution rapidly increased and peaked in April (n = 161, or 36.5% of all visits) and May 2020 (n = 149, or 29.6% of all visits) (Fig. 1). As the number of in-person visits increased towards June 2020, telehealth visits gradually decreased (June 2020: n = 98, 8.5% of total; July 2020: n = 95, 8.2%; August 2020: n = 70, 6.1% of total) and reached a plateau around September 2020 (n = 62, 8.9% of total). After September 2020, the number of telehealth visits remained relatively stable, amounting to 64 monthly visits (9.9% of total visits) by the end of the study period in April 2021.
Sociodemographic and Clinical Factors Associated with Receipt of Telehealth
On multivariable logistic regression, several sociodemographic and clinical factors were associated with an increased likelihood of receiving a telehealth visit over the course of the study. Specifically, older patients were less likely to have a telehealth visit (odds ratio [OR] 0.89, 95% confidence interval [CI] 0.80–0.98 per 10-year increase), while male patients were decidedly more likely to have a telehealth visit than female patients (OR 1.83, 95% CI 1.45–2.32) (Table 2). Additionally, health insurance status was associated with an increased likelihood of receiving telehealth services. In particular, patients insured through Medicare had 58% increased odds of having a telehealth visit compared with patients insured through Medicaid (OR 1.58, 95% CI 1.04–2.41). Patient county of residence also had an influence on the odds of receiving telehealth visits, with patients from non-neighboring counties having 33% increased odds of at least one telehealth visit over the study period compared with patients from neighboring counties (OR 1.33, 95% CI 1.06–1.66). Interestingly, county-level DDI had no discernible impact on the odds of having a telehealth visit (medium vs. low DDI: OR 0.99, 95% CI 0.78–1.26; high vs. low DDI: OR 1.15, 95% CI 0.85–1.57). Of note, cancer diagnosis had the most pronounced effect on the likelihood of having telehealth visits. Specifically, patients diagnosed with endocrine tumors were much more likely to have received a telehealth care than patients diagnosed with breast cancer (OR 16.83, 95% CI 11.24–25.19). Similarly, patients diagnosed with urinary tract cancers (OR 14.91, 95% CI 5.56–39.98), pancreatic cancer (OR 9.19, 95% CI 6.38–13.23), liver or biliary tract cancer (OR 6.78, 95% CI 4.39–10.49), lung cancer (OR 5.74, 95% CI 3.04–10.86), colorectal cancer (OR 5.31, 95% CI 3.71–7.58), cancers of the female reproductive system (OR 4.24, 95% CI 2.33–7.74), lymphoma or leukemia (OR 4.00, 95% CI 1.46–10.96), or skin cancer (OR 2.47, 95% CI 1.34–4.54) all had higher odds of having a telehealth visit than patients diagnosed with breast cancer. Results of the sensitivity analysis to assess receipt of telehealth visits during the height of telehealth use (1 March 2020–31 May 2020) are shown in electronic supplementary Table S2.
Results of the multivariable logistic regression model were then stratified by neighboring county status. Among patients who resided in a neighboring county, older age was associated with lower odds of receiving telehealth visits (OR 0.83, 95% CI 0.72–0.97 per 10-year increase) (Table 3). Conversely, male sex (OR 2.56, 95% CI 1.77–3.70) and Medicare beneficiary status (vs. Medicaid beneficiary: OR 2.18, 95% CI 1.14–4.18) were associated with higher odds of receiving telehealth visits. The factor most strongly associated with the receipt of telehealth visits was cancer diagnosis. Specifically, patients diagnosed with endocrine tumors (OR 13.43, 95% CI 7.43–24.27), liver and biliary tract cancers (OR 11.33, 95% CI 5.25–24.46), cancers of the urinary tract (OR 10.45, 95% CI 2.43–45.04), pancreatic cancer (OR 6.49, 95% CI 3.53–11.95), colorectal cancer (OR 4.40, 95% CI 2.70–7.17), or cancers of the female reproductive system (OR 3.95, 95% CI 1.78–8.77) all had higher odds of receiving telehealth visits compared with patients diagnosed with breast cancer. Among patients who resided in non-neighboring counties, only cancer diagnosis was associated with the likelihood to receive telehealth visits (Table 4). In particular, patients diagnosed with urinary tract cancers (OR 22.92, 95% CI 5.71–91.97), endocrine tumors (OR 20.95, 95% CI 11.89–36.91), pancreatic cancer (OR 11.83, 95% CI 7.38–18.96), lung cancer (OR 7.72, 95% CI 3.69–16.14), colorectal cancer (OR 6.96, 95% CI 4.07–11.90), liver and biliary tract cancers (OR 5.79, 95% CI 3.36–10.00), cancers of the female reproductive system (OR 4.59, 95% CI 1.81–11.62), lymphomas or leukemias (OR 4.51, 95% CI 1.29–15.75), or skin cancers (OR 2.50, 95% CI 1.04–6.01) all had higher odds of receiving telehealth visits compared with patients diagnosed with breast cancer.
Discussion
The COVID-19 pandemic triggered sweeping restrictions in the delivery of healthcare in an effort to avoid unnecessary exposure to the pandemic, as well as to reduce utilization of limited medical resources. In turn, the exploration of telehealth modalities in the form of audio and audio/video healthcare visits was accelerated to bridge these gaps and to provide necessary medical care to those in need. Although implemented broadly across medicine and lauded for its benefits, implementation in the surgical setting has been relatively slow with greater adoption since the pandemic due to leniency in the guidelines governing telehealth use.24 However, telehealth services may not be equally accessible to all patients. In fact, in parallel with telehealth implementation, regional and socioeconomic disparities in the availability of modern information technology (the so-called ‘digital divide’) in access to telehealth services has come to light.25,26 As such, increased reliance on telehealth services may run the risk of widening, rather than narrowing, existing disparities in access to telehealth resources in the care of the surgical patient.27 In this context, the current study was important because we assessed the sociodemographic and clinical factors influencing patient access to telehealth visits among a cohort of surgical oncology patients treated at a single large academic center. Moreover, we used a validated measure of the availability of modern information technology (the DDI) to examine its impact on the likelihood to receive telehealth visits. Of note, patients who were younger, male, insured through Medicare, or resided in counties distant from the hospital had as much as 83% increased odds of receiving telehealth visits. Additionally, the likelihood of utilizing telehealth services varied substantially by the primary site of cancer. In contrast, county-level DDI had no impact on the odds of receiving telehealth visits, regardless of whether patients resided in neighboring counties.
Despite the abrupt transition to telehealth services during the COVID-19 pandemic, sociodemographic barriers to telehealth services have persisted.28,29 The current study demonstrated that patients were more likely to receive surgical oncology-related telehealth visits when the patient was younger/male versus older/female. Furthermore, patients insured through Medicare had 58% increased odds of receiving telehealth visits compared with patients who received Medicaid. Discrepancies in telehealth utilization may exist secondary to a lack of access to digital media platforms. Roberts and Mehrotra reported that 26.3% of Medicare beneficiaries lacked any form of digital access. Furthermore, the proportion of individuals without digital access was higher among widowed, less educated, disabled, Black or Hispanic individuals.30,31 Similarly, Javier-DesLoges et al. studied 2516 urology patients at a large academic institution and noted that patients who were Hispanic or had Medicaid insurance were less likely to access telemedicine during the pandemic.32 Results of the current study are consistent with these previous findings and suggest that telemedicine utilization may have a harder time gaining traction among more socially vulnerable surgical patients such as Medicaid beneficiaries. Of note, we did not note disparities in access to telemedicine among surgical oncology patients relative to race/ethnicity. While likely multifactorial, the lack of an impact of race/ethnicity on telehealth use may have been related to the current cohort being racially/ethnically and linguistically homogeneous, as the majority of patients were White with English as their preferred language.
Utilization of telehealth visits varied considerably based on cancer diagnosis. Specifically, compared with patients with breast cancer, patients diagnosed with urinary tract and endocrine cancers had much higher odds of receiving telehealth visits. Chao et al. had previously noted that utilization of telemedicine varied substantially by surgical subspecialty. Specifically, neurosurgery and urology were the surgical subspecialties with the highest telehealth conversion rates at 13.8% and 14.3%, respectively. Conversely, ophthalmology and orthopedics were the two surgical subspecialties with the lowest telehealth conversion rates at 0.3% and 2.3%, respectively.33 Variation in adoption of telemedicine across surgical subspecialties may be due at least in part to differences in practice patterns predating the pandemic. In a study using the American Medical Association’s 2016 Physician Practice Benchmark Survey, Kane and Gillis identified considerable variability in the proportion of surgeons using telehealth across surgical subspecialties, ranging from 9.3% of obstetricians and gynecologists to 15.0% of dermatologic surgeons.34 It is likely that providers who relied on previous experience providing telehealth services adapted more quickly to the increased need for telemedicine brought about by the pandemic. In addition, certain patients, such as women with breast cancer, may strongly prefer in-person clinical appointments. Taken together, the data highlight how different clinical contexts can influence the utilization of telehealth services.
The digital divide is often referenced as a barrier to the expansion of telehealth services. Alarmingly, as of 2019, as many as one in four of all individuals in the US still lack fixed home broadband, although several national efforts have more recently sought to reduce this disparity in access to telehealth services.25 In turn, concerns exist that heavier reliance on telehealth services may exacerbate existing inequalities in access to care.35 The expansion of telemedicine in the surgical setting holds the promise of improving access to healthcare. However, barriers to its implementation exist at the national and institutional level, such as the cost savings for the healthcare system and appropriate training and education of healthcare providers.36 As such, many major payers of health services, including Medicare and Medicaid, have begun to help bridge this gap through policy change, grant funding, and technical assistance, as these payers view telehealth as a cost effective method of healthcare delivery.37 Of note, consistent with these efforts, data from the current study demonstrated that surgical oncology patients residing in counties of medium or high DDI had similar odds of receiving telehealth visits compared with patients from counties of low DDI. The ubiquitous nature of mobile phones may have also helped close some of the digital divide. In particular, mobile phones are extremely accessible, with Pew Research reporting that more than 95% of Americans younger than 49 years of age own a smartphone, allowing users to more easily reach clinicians through secure mobile-friendly web portals.38 Taken together, the data suggest that certain demographic factors (i.e., age, etc.) may impact telehealth use more than access to the internet/mobile services.
Several limitations should be considered when interpreting the results of the current study. The study involved only one large academic institution, thus limiting generalizability. However, the current study did include a large cohort from a comprehensive cancer center to define utilization of telehealth services among cancer patients at a high-volume center. It is possible that patients who would have otherwise had a surgical oncology visit during the study period did not due to an unwillingness or impossibility to receive telehealth care. Such patients were not considered in the current analysis, as they would have been ‘missing’ from the cohort. In addition, as telehealth visits could not be reliably identified prior to 16 March 2020, comparisons of telehealth utilization patterns before and after this date were not possible. Since DDI values were reported at the county level, variability in access to information technology within counties almost certainly existed. As such, county-level DDI values may not necessarily reflect the ability of any given individual patient to access information technology. However, the goal of the current study was to establish whether residing in areas with more limited access to information technology may have an impact on the ability to receive telehealth services. As such, inferences at the individual patient level may not be appropriate. The majority of patients also came from counties within a narrow range of DDI scores. In turn, it is possible that the lack of variability in county-level DDI scores influenced the ability to detect an effect of DDI on the likelihood to receive telehealth visits. Of note, patient ZIP code of residence was converted into the county to which the highest proportion of residential addresses within each ZIP code belonged. As such, inaccuracies in the conversion of ZIP codes into counties, while rare, may have been possible.
Conclusion
Several sociodemographic and clinical characteristics were associated with the likelihood of receiving a surgical oncology telehealth visit during the COVID-19 pandemic, including age, sex, insurance status, and primary site of cancer. In contrast, county-level DDI had no discernible impact on the likelihood of receiving telehealth visits. Taken together, these results suggest that while certain sociodemographic characteristics may contribute to the likelihood of receiving telehealth visits in this population, the impact of the digital divide was not as impactful. Clinicians need to recognize and address sociodemographic barriers that impede the use of telehealth services in the surgical oncologic setting to ensure equal access to care for all.
References
Webster P. Virtual health care in the era of COVID-19. Lancet. 2020;395(10231):1180–1. https://doi.org/10.1016/S0140-6736(20)30818-7.
Centers for medicare and medicaid services. Trump administration makes sweeping regulatory changes to help U.S. healthcare system address COVID-19 patient surge. Available at: https://www.cms.gov/newsroom/press-releases/trump-administration-makes-sweeping-regulatory-changes-help-us-healthcare-system-address-covid-19. Accessed 14 Feb 2022.
Federation of state medical boards. US States and territories modifying requirements for telehealth in response to COVID-19. Available at: http://www.fsmb.org/siteassets/advocacy/pdf/states-waiving-licensure-requirements-for-telehealth-in-response-to-covid-19.pdf. Accessed 14 Feb 2022.
Augenstein, J. Opportunities to expand telehealth use amid the coronavirus pandemic. Available at: https://www.healthaffairs.org/do/https://doi.org/10.1377/forefront.20200315.319008/full/. Accessed 15 Feb 2022.
Verma, S. Early impact of CMS expansion of medicare telehealth during COVID-19. Available at: https://www.healthaffairs.org/do/https://doi.org/10.1377/forefront.20200715.454789/full/. Accessed 14 Feb 2022.
Weiner, S. What happens to telemedicine after COVID-19? Available at: http://www.aamc.org/news-insights/what-happens-telemedicine-after-covid-19. Accessed 15 Feb 2022.
Centers for medicare and medicaid services. Calendar year (CY) 2022 medicare physician fee schedule final rule. Centers for medicare and medicaid services; 2021.
Grenda TR, Whang S, Evans NR. Transitioning a surgery practice to telehealth during COVID-19. Ann Surg. 2020;272(2):e168–9. https://doi.org/10.1097/SLA.0000000000004008.
Kummerow Broman K, Roumie CL, Stewart MK, et al. Implementation of a telephone postoperative clinic in an integrated health system. J Am Coll Surg. 2016;223(4):644–51. https://doi.org/10.1016/j.jamcollsurg.2016.07.010.
Williams AM, Bhatti UF, Alam HB, Nikolian VC. The role of telemedicine in postoperative care. Mhealth. 2018;4:11. https://doi.org/10.21037/mhealth.2018.04.03.
Kulshrestha S, Sweigert PJ, Tonelli C, et al. Textbook oncologic outcome in pancreaticoduodenectomy: do regionalization efforts make sense? J Surg Oncol. 2022;125(3):414–24. https://doi.org/10.1002/jso.26712.
Levy J, Gupta V, Amirazodi E, et al. Gastrectomy case volume and textbook outcome: an analysis of the population registry of esophageal and stomach tumours of ontario (PRESTO). Gastric Cancer. 2020;23(3):391–402. https://doi.org/10.1007/s10120-019-01015-w.
Mehta R, Tsilimigras DI, Paredes AZ, et al. Dedicated cancer centers are more likely to achieve a textbook outcome following hepatopancreatic surgery. Ann Surg Oncol. 2020;27(6):1889–97. https://doi.org/10.1245/s10434-020-08279-y.
Diaz A, Schoenbrunner A, Pawlik TM. Trends in the geospatial distribution of adult inpatient surgical cancer care across the united states. J Gastrointest Surg. 2020;24(9):2127–34. https://doi.org/10.1007/s11605-019-04343-5.
Dalmacy DM, Tsilimigras DI, Hyer JM, Paro A, Diaz A, Pawlik TM. Social vulnerability and fragmentation of postoperative surgical care among patients undergoing hepatopancreatic surgery. Surgery. 2022;171(4):1043–50. https://doi.org/10.1016/j.surg.2021.08.030.
Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375(2):154–61. https://doi.org/10.1056/NEJMra1601705.
Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4–12. https://doi.org/10.1177/1357633X16674087.
Mishori R, Antono B. Telehealth, rural america, and the digital divide. J Ambul Care Manage. 2020;43(4):319–22. https://doi.org/10.1097/JAC.0000000000000348.
Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020;27(7):1147–8. https://doi.org/10.1093/jamia/ocaa078.
American medical informatics association. AMIA responds to FCC notice on broadband enabled technology. Available at: https://amia.org/public-policy/public-comments/amia-responds-fcc-notice-broadband-enabled-health-technology. Accessed 15 Feb 2022.
State medical board of ohio. Telemedicine guidance. Available at: http://www.med.ohio.gov/telemedicine-guidance. Accessed 11 Feb 2022.
US Department of housing and urban development. Office of policy development and research. HUD USPS ZIP code crosswalk files. Available at: https://www.huduser.gov/portal/datasets/usps_crosswalk.html. Accessed 27 Jan 2022.
Gallardo R. Digital divide index. Available at: http://pcrd.purdue.edu/ddi. Accessed 27 Jan 2022,
Evans H, Yeo HL, Zhao J, et al. Adopting telemedicine in surgical care: what you need to know. American college of surgeons. Available at: https://bulletin.facs.org/2021/04/adopting-telemedicine-in-surgical-care-what-you-need-to-know/. Accessed 30 Mar 2022
Eyrich NW, Andino JJ, Fessell DP. Bridging the digital divide to avoid leaving the most vulnerable behind. JAMA Surg. 2021;156(8):703–4. https://doi.org/10.1001/jamasurg.2021.1143.
Benda NC, Veinot TC, Sieck CJ, Ancker JS. Broadband internet access is a social determinant of health! Am J Public Health. 2020;110(8):1123–5. https://doi.org/10.2105/AJPH.2020.305784.
Wong JH, Irish WD, DeMaria EJ, et al. Development and assessment of a systematic approach for detecting disparities in surgical access. JAMA Surg. 2021;156(3):239–45. https://doi.org/10.1001/jamasurg.2020.5668.
Annapragada AV, Meshram P, Jenkins SG, et al. Age and racial disparities in telemedicine utilization in an academic orthopedic surgery department. Telemed J E Health. 2022;28(7):970–5. https://doi.org/10.1089/tmj.2021.0330.
Ryskina KL, Shultz K, Zhou Y, Lautenbach G, Brown RT. Older adults’ access to primary care: gender, racial, and ethnic disparities in telemedicine. J Am Geriatr Soc. 2021;69(10):2732–40. https://doi.org/10.1111/jgs.17354.
Roberts ET, Mehrotra A. Assessment of disparities in digital access among medicare beneficiaries and implications for telemedicine. JAMA Intern Med. 2020;180(10):1386–9. https://doi.org/10.1001/jamainternmed.2020.2666.
Pew research center. Internet/Broadband fact sheet. Available at: http://www.pewresearch.org/internet/fact-sheet/internet-broadband/. Accessed 17 Feb 2022
Javier-DesLoges J, Meagher M, Soliman S, et al. Disparities in telemedicine utilization for urology patients during the covid-19 pandemic. Urology. 2022;163:80–6. https://doi.org/10.1016/j.urology.2021.11.037.
Chao GF, Li KY, Zhu Z, et al. Use of telehealth by surgical specialties during the COVID-19 pandemic. JAMA Surg. 2021;156(7):620–6. https://doi.org/10.1001/jamasurg.2021.0979.
Kane CK, Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Aff (Millwood). 2018;37(12):1923–30. https://doi.org/10.1377/hlthaff.2018.05077.
Mullangi S, Kaushal R, Ibrahim SA. Equity in the age of health care information technology and innovation: addressing the digital divide. Med Care. 2019;57(Suppl 2):S106–7. https://doi.org/10.1097/MLR.0000000000001033.
Asiri A, AlBishi S, AlMadani W, ElMetwally A, Househ M. The use of telemedicine in surgical care: a systematic review. Acta Inform Med. 2018;26(3):201–6. https://doi.org/10.5455/aim.2018.26.201-206.
Lin CC, Dievler A, Robbins C, Sripipatana A, Quinn M, Nair S. Telehealth in health centers: key adoption factors, barriers and opportunities. Health Aff (Millwood). 2018;37(12):1967–74. https://doi.org/10.1377/hlthaff.2018.05125.
Making telehealth accessible to underserved communities requires a multifaceted approach. Available at: https://hitconsultant.net/2021/05/28/making-telehealth-accessible-to-underserved-communities/. Accessed 21 Apr 2022
Acknowledgment
The authors would like to thank Dr. Roberto Gallardo and his team for providing us with the nationwide county-level DDI data used in the analysis.
Funding
No sources of funding were used to assist in the preparation of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Alessandro Paro, Daniel R. Rice, J. Madison Hyer, Elizabeth Palmer, Aslam Ejaz, Chanza Fahim Shaikh, and Timothy M. Pawlik have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Paro, A., Rice, D.R., Hyer, J.M. et al. Telehealth Utilization Among Surgical Oncology Patients at a Large Academic Cancer Center. Ann Surg Oncol 29, 7267–7276 (2022). https://doi.org/10.1245/s10434-022-12259-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12259-9