Abstract
Background
As the population ages, more elderly patients are receiving surgery for retroperitoneal sarcoma (RPS). However, high-quality data investigating associations between ageing and prognosis are lacking. Our study aimed to investigate whether ageing is associated with inferior short-term survival outcomes after RPS surgery.
Patients and Methods
Patients undergoing surgery for primary RPS between 2008 and 2019 at two tertiary sarcoma centres were analysed. The primary outcome was 1-year mortality, and the primary explanatory variable was patient age, classified as: < 55, 55–64, 65–74 or 75+ years.
Results
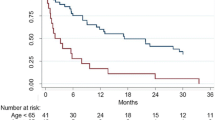
The 692 patients undergoing surgery (mean age 60.8 ± 13.8 years) had a 1-year mortality rate of 9.4%, which differed significantly by age (p < 0.001), with rates of 7.2%, 6.9%, 8.7% and 22.8% for the < 55, 55–64, 65–74 and 75+ years groups, respectively. The distribution of causes of death also differed significantly by age (p = 0.023), with 22% and 28% of deaths in the 65–74 and 75+ years groups caused by post-operative complications, versus none in the < 55 and 55–64 years groups. On multivariable analysis, age of 75+ years (versus < 55 years) was a significant independent predictor of 1-year mortality [odds ratio (OR) 7.05, 95% confidence interval (CI) 2.63–18.9, p < 0.001]; no significant increase in risk was observed in the 55–64 (OR 0.72, 95% CI 0.28–1.87) or 65–74 (OR 0.89, 95% CI 0.37–2.15) years groups.
Conclusions
Post-operative complications are an important cause of deaths in elderly patients. These findings are relevant to decision-making and counselling when surgery is considered for patients with RPS.



Similar content being viewed by others
References
Stiller CA, Trama A, Serraino D, et al. Descriptive epidemiology of sarcomas in Europe: report from the RARECARE project. Eur J Cancer. 2013;49(3):684–95. https://doi.org/10.1016/j.ejca.2012.09.011.
Antonescu CR, WHO, Classification of Tumours Editorial Board. Soft tissue and bone tumours. Lyon: International Agency for Research on Cancer; 2020.
Gronchi A, Miah AB, Dei Tos AP, et al. Soft tissue and visceral sarcomas: ESMO-EURACAN-GENTURIS Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021;32(11):1348–65. https://doi.org/10.1016/j.annonc.2021.07.006.
Swallow CJ, Strauss DC, Bonvalot S, et al. Management of primary retroperitoneal sarcoma (rps) in the adult: an updated consensus approach from the transatlantic australasian RPS working group. Ann Surg Oncol. 2021;28(12):7873–88. https://doi.org/10.1245/s10434-021-09654-z.
MacNeill AJ, Gronchi A, Miceli R, et al. Postoperative morbidity after radical resection of primary retroperitoneal sarcoma. Ann Surg. 2018;267(5):959–64. https://doi.org/10.1097/SLA.0000000000002250.
Tirotta F, Parente A, Hodson J, et al. Cumulative burden of postoperative complications in patients undergoing surgery for primary retroperitoneal sarcoma. Ann Surg Oncol. 2021;28(12):7939–49. https://doi.org/10.1245/s10434-021-10059-1.
United Nations. World Population Prospects: The 2017 Revision, World Population 2017 Wallchart; Department of Economic and Social Affairs: New York, NY, USA, 2017.
Hoven-Gondrie ML, Bastiaannet E, Ho VK, et al. Worse survival in elderly patients with extremity soft-tissue sarcoma. Ann Surg Oncol. 2016;23(8):2577–85. https://doi.org/10.1245/s10434-016-5158-7.
Acem I, Verhoef C, Rueten-Budde AJ, et al. Age-related differences of oncological outcomes in primary extremity soft tissue sarcoma: a multistate model including 6260 patients. Eur J Cancer. 2020;141:128–36. https://doi.org/10.1016/j.ejca.2020.09.021.
Kamarajah SK, Gujjuri RR, Elhadi M, et al. Elderly patients have increased perioperative morbidity and mortality from oesophagectomy for oesophageal cancer: A systematic review and meta-analysis. Eur J Surg Oncol. 2021;47(8):1828–35. https://doi.org/10.1016/j.ejso.2021.02.030.
Hashimoto T, Kurokawa Y, Mikami J, et al. postoperative long-term outcomes in elderly patients with gastric cancer and risk factors for death from other diseases. World J Surg. 2019;43(11):2885–93. https://doi.org/10.1007/s00268-019-05109-5.
van Tuil T, Dhaif AA, Te Riele WW, et al. Systematic review and meta-analysis of liver resection for colorectal metastases in elderly patients. Dig Surg. 2019;36(2):111–23. https://doi.org/10.1159/000487274.
Millan M, Merino S, Caro A, et al. Treatment of colorectal cancer in the elderly. World J Gastrointest Oncol. 2015;7(10):204–20. https://doi.org/10.4251/wjgo.v7.i10.204.
Oliveira-Cunha M, Malde DJ, et al. Results of pancreatic surgery in the elderly: is age a barrier? HPB. 2013;15(1):24–30. https://doi.org/10.1111/j.1477-2574.2012.00549.x.
Oken M, Creech R, Tormey D, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.
ASA House of Delegates. ASA physical status classification system. 2014. https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system . Accessed 5 January 2022.
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82. https://doi.org/10.1093/aje/kwq433.
Coindre JM, Trojani M, Contesso G, et al. Reproducibility of a histopathologic grading system for adult soft tissue sarcoma. Cancer. 1986;58(2):306–9. https://doi.org/10.1002/1097-0142(19860715)58:2%3c306::aid-cncr2820580216%3e3.0.co;2-7.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Slankamenac K, Graf R, Barkun J, et al. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258(1):1–7. https://doi.org/10.1097/SLA.0b013e318296c732.
Trevor Hastie, gam: Generalized Additive Models. R package version 1.20. https://CRAN.R-project.org/package=gam. Accessed 5 January 2022 (2020).
R Core Team, R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/. Accessed 5 January 2022 (2021).
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2007;18(6):800–4. https://doi.org/10.1097/EDE.0b013e3181577654.
Sourrouille I, Macovei R, Faron M, et al. Long-term outcome after surgery for a localized retroperitoneal soft tissue sarcoma in elderly patients: results from a retrospective, single-center study. Ann Surg Oncol. 2018;25(8):2201–8. https://doi.org/10.1245/s10434-018-6529-z.
Smith HG, Thomas JM, Smith MJ, et al. Multivisceral resection of retroperitoneal sarcomas in the elderly. Eur J Cancer. 2016;69:119–26. https://doi.org/10.1016/j.ejca.2016.09.037.
Tirotta F, Parente A, Richardson T, et al. Comparison of comprehensive complication index and Clavien-Dindo classification in patients with retroperitoneal sarcoma. J Surg Oncol. 2021;124(7):1166–72. https://doi.org/10.1002/jso.26612.
Tosato M, Zamboni V, Ferrini A, et al. The aging process and potential interventions to extend life expectancy. Clin Interv Aging. 2007;2(3):401–12.
Partridge J, Sbai M, Dhesi J. Proactive care of older people undergoing surgery. Aging Clin Exp Res. 2018;30(3):253–7. https://doi.org/10.1007/s40520-017-0879-4.
Harari D, Hopper A, Dhesi J, et al. Proactive care of older people undergoing surgery ('POPS’): designing, embedding, evaluating and funding a comprehensive geriatric assessment service for older elective surgical patients. Age Ageing. 2007;36(2):190–6. https://doi.org/10.1093/ageing/afl163.
Carli F, Bousquet-Dion G, Awasthi R, et al. Effect of multimodal prehabilitation vs postoperative rehabilitation on 30-day postoperative complications for frail patients undergoing resection of colorectal cancer: a randomized clinical trial. JAMA Surg. 2020;155(3):233–42. https://doi.org/10.1001/jamasurg.2019.5474.
Kehlet H. Prehabilitation in surgery—need for new strategies? Eur J Surg Oncol. 2021;47(5):929–30. https://doi.org/10.1016/j.ejso.2020.11.124.
Gillis C, Fenton TR, Gramlich L, et al. Older frail prehabilitated patients who cannot attain a 400 m 6-min walking distance before colorectal surgery suffer more postoperative complications. Eur J Surg Oncol. 2021;47(4):874–81. https://doi.org/10.1016/j.ejso.2020.09.041.
Argillander TE, Heil TC, Melis RJF, et al. Preoperative physical performance as predictor of postoperative outcomes in patients aged 65 and older scheduled for major abdominal cancer surgery: a systematic review. Eur J Surg Oncol. 2021. 1;S0748-7983(21)00746-0. https://doi.org/10.1016/j.ejso.2021.09.019.
Ljungqvist O. ERAS—enhanced recovery after surgery. J Parenter Enteral Nutr. 2014;38(5):559–66. https://doi.org/10.1177/0148607114523451.
Fearon KC, Ljungqvist O, Meyenfeldt M, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24(3):466–77. https://doi.org/10.1016/j.clnu.2005.02.002.
Anderson AD, McNaught CE, MacFie J, et al. Randomized clinical trial of multimodal optimization and standard perioperative surgical care. Br J Surg. 2003;90(12):1497–504. https://doi.org/10.1002/bjs.4371.
Delaney CP, Zutshi M, Senagore AJ, et al. Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative care after laparotomy and intestinal resection. Dis Colon Rectum. 2003;46(7):851–9. https://doi.org/10.1007/s10350-004-6672-4.
Gatt M, Anderson AD, Reddy BS, et al. Randomized clinical trial of multimodal optimization of surgical care in patients undergoing major colonic resection. Br J Surg. 2005;92(11):1354–62. https://doi.org/10.1002/bjs.5187.
Lv L, Shao YF, Zhou YB. The enhanced recover after surgery (ERAS) pathway for patients undergoing colorectal surgery: an update of meta-analysis of randomized controlled trials. Int J Colorectal Dis. 2012;27(12):1549–54. https://doi.org/10.1007/s00384-012-1577-5.
Lyu HG, Saadat LV, Bertagnolli MM, et al. Enhanced recovery after surgery pathway in patients with soft tissue sarcoma. Br J Surg. 2020;107(12):1667–72. https://doi.org/10.1002/bjs.11758.
Gutierrez JC, Perez EA, Moffat FL, et al. Should soft tissue sarcomas be treated at high-volume centres? An analysis of 4205 patients. Ann Surg. 2007;245(6):952–8. https://doi.org/10.1097/01.sla.0000250438.04393.a8.
Keung EZ, Chiang YJ, Cormier JN, et al. Treatment at low-volume hospitals is associated with reduced short-term and long-term outcomes for patients with retroperitoneal sarcoma. Cancer. 2018;124(23):4495–503. https://doi.org/10.1002/cncr.31699.
Vos M, Blaauwgeers HGT, Ho VKY, et al. Increased survival of non-low-grade and deep-seated soft tissue sarcoma after surgical management in high-volume hospitals: a nationwide study from the Netherlands. Eur J Cancer. 2019;110:98–106. https://doi.org/10.1016/j.ejca.2019.01.005.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
DISCLOSURE
The authors declare no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tirotta, F., Fadel, M.G., Hodson, J. et al. Association Between Ageing and Short-Term Survival Outcomes in Patients Undergoing Surgery for Primary Retroperitoneal Sarcoma. Ann Surg Oncol 29, 7320–7330 (2022). https://doi.org/10.1245/s10434-022-12231-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12231-7