Abstract
Background
Consensus guidelines discourage resection of poorly differentiated pancreatic neuroendocrine carcinoma (panNEC) given its association with poor long-term survival. This study assessed treatment patterns and outcomes for this rare malignancy using the National Cancer Database (NCDB).
Methods
Patients with non-functional pancreatic neuroendocrine tumors in the NCDB (2004–2016) were categorized based on pathologic differentiation. Logistic and Cox proportional hazard regressions identified associations with resection and overall survival (OS). Survival was compared using Kaplan-Meier and log-rank tests.
Results
Most patients (83%) in the cohort of 8560 patients had well-differentiated tumors (panNET). The median OS was 47 months (panNET, 63 months vs panNEC, 17 months; p < 0.001). Surgery was less likely for older patients (odds ratio [OR], 0.97), patients with panNEC (OR, 0.27), and patients with metastasis at diagnosis (OR, 0.08) (all p < 0.001). After propensity score-matching of these factors, surgical resection was associated with longer OS (82 vs 29 months; p < 0.001) and a decreased hazard of mortality (hazard ratio [HR], 0.37; p < 0.001). Surgery remained associated with longer OS when stratified by differentiation (98 vs 41 months for patients with panNET and 36 vs 8 months for patients with panNEC). Overall survival did not differ between patients with panNEC who underwent surgery and patients with panNET who did not (both 39 months; p = 0.294).
Conclusions
Poorly differentiated panNEC exhibits poorer survival than well-differentiated panNET. In the current cohort, surgical resection was strongly and independently associated with improved OS, suggesting that patients with panNEC who are suitable operative candidates should be considered for multimodality therapy, including surgery.


Similar content being viewed by others
References
Cloyd JM, Poultsides GA. The Landmark Series: pancreatic neuroendocrine tumors. Ann Surg Oncol. 2020;28:1039–49. https://doi.org/10.1245/s10434-020-09133-x.
Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3:1335. https://doi.org/10.1001/jamaoncol.2017.0589.
Guilmette JM, Nosé V. Neoplasms of the neuroendocrine pancreas: an update in the classification, definition, and molecular genetic advances. Adv Anatomic Pathol. 2019;26:13–30. https://doi.org/10.1097/PAP.0000000000000201.
Rindi G, Klimstra DS, Abedi-Ardekani B, et al. A common classification framework for neuroendocrine neoplasms: an International Agency for Research on Cancer (IARC) and World Health Organization (WHO) expert consensus proposal. Mod Pathol. 2018;31:1770–86. https://doi.org/10.1038/s41379-018-0110-y.
Howe JR, Merchant NB, Conrad C, et al. The North American neuroendocrine tumor society consensus paper on the surgical management of pancreatic neuroendocrine tumors. Pancreas. 2020;49:1–33. https://doi.org/10.1097/MPA.0000000000001454.
National Comprehensive Cancer Network (NCCN). NCCN clinical practice guidelines in oncology: neuroendocrine and adrenal tumors. NCCN Clinical Practice Guidelines in OncologyCCN. Published 2021. Retrieved 29 June 2021 at https://www.nccn.org/professionals/physician_gls/pdf/neuroendocrine.pdf.
Ballian N, Loeffler AG, Rajamanickam V, Norstedt PA, Weber SM, Cho CS. A simplified prognostic system for resected pancreatic neuroendocrine neoplasms. HPB. 2009;11:422–8. https://doi.org/10.1111/j.1477-2574.2009.00082.x.
Fischer L, Bergmann F, Schimmack S, et al. Outcome of surgery for pancreatic neuroendocrine neoplasms. British Journal of Surgery. 2014;101(11):1405–12. https://doi.org/10.1002/bjs.9603..
Haugvik SP, Janson ET, Österlund P, et al. Surgical treatment as a principle for patients with high-grade pancreatic neuroendocrine carcinoma: a Nordic multicenter comparative study. Ann Surg Oncol. 2016;23:1721–8. https://doi.org/10.1245/s10434-015-5013-2.
Feng T, Lv W, Yuan M, Shi Z, Zhong H, Ling S. Surgical resection of the primary tumor leads to prolonged survival in metastatic pancreatic neuroendocrine carcinoma. World J Surg Oncol. 2019;17:54. https://doi.org/10.1186/s12957-019-1597-5.
American College of Surgeons. National Cancer Database. Published 2020. Retrieved 10 November 2020 at https://www.facs.org/quality-programs/cancer/ncdb/about.
World Health Organization. International Classification of Diseases for Oncology. 3rd ed. Fritz A, Percy C, Jack A, et al (eds). World Health Organization, 2013. Retrieved 10 November 2020 at https://apps.who.int/iris/bitstream/handle/10665/96612/9789241548496_eng.pdf.
Rubin DB. Using propensity scores to help design observational studies: application to the tobacco litigation. Health Serv Outcomes Res Methodol. 2001. https://doi.org/10.1023/A:1020363010465.
Assi HA, Mukherjee S, Kunz PL, et al. Surgery versus surveillance for well-differentiated, nonfunctional pancreatic neuroendocrine tumors: an 11-year analysis of the National Cancer Database. Oncologist. 2020;25:276–83. https://doi.org/10.1634/theoncologist.2019-0466.
Mao R, Zhao H, Li K, et al. Outcomes of lymph node dissection for non-metastatic pancreatic neuroendocrine tumors: a propensity score-weighted analysis of the National Cancer Database. Ann Surg Oncol. 2019;26:2722–9. https://doi.org/10.1245/s10434-019-07506-5.
Concors SJ, Sinnamon AJ, Ecker BL, et al. The impact of surgery for metastatic pancreatic neuroendocrine tumor: a contemporary evaluation matching for chromogranin a level. HPB. 2020;22:83–90. https://doi.org/10.1016/j.hpb.2019.05.011.
Bilimoria KY, Talamonti MS, Tomlinson JS, et al. Prognostic score predicting survival after resection of pancreatic neuroendocrine tumors analysis of 3851 patients. Ann Surg. 2008;247:490–500. https://doi.org/10.1097/SLA.0b013e31815b9cae.
Vaghaiwalla T, Keutgen XM. Surgical management of pancreatic neuroendocrine tumors. Surg Oncol Clin North Am. 2020;29:243–52. https://doi.org/10.1016/j.soc.2019.11.008.
Hill JS, McPhee JT, McDade TP, et al. Pancreatic neuroendocrine tumors. Cancer. 2009;115:741–51. https://doi.org/10.1002/cncr.24065.
Keutgen XM, Nilubol N, Glanville J, et al. Resection of primary tumor site is associated with prolonged survival in metastatic nonfunctioning pancreatic neuroendocrine tumors. Surgery. 2016;159:311–9. https://doi.org/10.1016/j.surg.2015.05.042.
Hüttner FJ, Schneider L, Tarantino I, et al. Palliative resection of the primary tumor in 442 metastasized neuroendocrine tumors of the pancreas: a population-based, propensity score-matched survival analysis. Langenbeck’s Arch Surg. 2015;400:715–23. https://doi.org/10.1007/s00423-015-1323-x.
Chivukula SV, Tierney JF, Hertl M, Poirier J, Keutgen XM. Operative resection in early-stage pancreatic neuroendocrine tumors in the United States: are we over- or undertreating patients? Surgery. 2020;167:180–6. https://doi.org/10.1016/j.surg.2019.04.061.
Alese OB, Jiang R, Shaib W, et al. High-grade gastrointestinal neuroendocrine carcinoma management and outcomes: a National cancer database study. Oncologist. 2020;25:911–20. https://doi.org/10.1634/theoncologist.2020-0135.
Thornblade LW, Warner SG, Melstrom L, et al. Does surgery provide a survival advantage in non-disseminated poorly differentiated gastroenteropancreatic neuroendocrine neoplasms? Surgery. 2021;169(6):1417–23. https://doi.org/10.1016/j.surg.2021.01.026.
Chan H, Zhang L, Choti MA, et al. Recurrence patterns after surgical resection of gastroenteropancreatic neuroendocrine tumors: analysis from the National comprehensive cancer network oncology outcomes database. Pancreas. 2021;50:506–12. https://doi.org/10.1097/MPA.0000000000001791.
Tierney JF, Chivukula SV, Wang X, et al. Resection of primary tumor may prolong survival in metastatic gastroenteropancreatic neuroendocrine tumors. Surgery. 2019;165:644–51. https://doi.org/10.1016/j.surg.2018.09.006.
Manasanch EE, Smith JK, Bodnari A, et al. Tumor registry versus physician medical record review: a direct comparison of patients with pancreatic neuroendocrine tumors. J Oncol Pract. 2011;7:111–6. https://doi.org/10.1200/JOP.2010.000097.
Bilimoria KY, Tomlinson JS, Merkow RP, et al. Clinicopathologic features and treatment trends of pancreatic neuroendocrine tumors: analysis of 9821 patients. J Gastrointest Surg. 2007;11:1460–9. https://doi.org/10.1007/s11605-007-0263-3.
Conrad C, Kutlu OC, Dasari A, et al. Prognostic value of lymph node status and extent of lymphadenectomy in pancreatic neuroendocrine tumors confined to and extending beyond the pancreas. J Gastrointest Surg. 2016;20:1966–74. https://doi.org/10.1007/s11605-016-3243-7.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was presented at the Americas Hepato-Pancreato-Biliary Association 2021 Annual Meeting, August 2–5, 2021 in Miami, Florida.
Supplementary Information
Below is the link to the electronic supplementary material.
10434_2022_11477_MOESM2_ESM.png
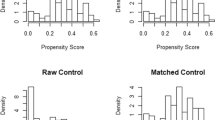
FIG. S1 Covariate balance before propensity score-matching (entire cohort) and in the propensity score-matched cohort (PNG 28 kb)
Rights and permissions
About this article
Cite this article
Kaslow, S.R., Vitiello, G.A., Prendergast, K. et al. Surgical Treatment of Patients with Poorly Differentiated Pancreatic Neuroendocrine Carcinoma: An NCDB Analysis. Ann Surg Oncol 29, 3522–3531 (2022). https://doi.org/10.1245/s10434-022-11477-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-11477-5