Abstract
Background
Laparoscopic radical antegrade modular pancreatosplenectomy (Lap-RAMPS) for left-sided pancreatic cancer remains a technically challenging procedure. How to approach the splenic artery in laparoscopic surgery has not been discussed in adequate detail, and the implications of an artery-first approach in left-sided pancreatic cancer remain unclear.
Patients and Methods
Forty-five consecutive patients with left-sided resectable pancreatic cancer underwent Lap-RAMPS between July 2018 and September 2020. They were divided according to whether Lap-RAMPS was performed using an anterocranial splenic artery-first (ASF) approach (ASF group, n = 23) or via another approach (non-ASF group, n = 22). Clinical, pathological, and short-term outcomes were reviewed and compared between the groups.
Results
The ASF approach was performed safely in all patients with resectable left-sided pancreatic cancer, and none required conversion to laparotomy. The ASF group had better outcomes in terms of conspicuous bleeding from the spleen during splenic mobilization (P = 0.016) and blood pooling during posterior dissection (P = 0.035). Consequently, blood loss was significantly less and operation time was significantly shorter in the ASF group than in the non-ASF group. There was no significant between-group difference in other short-term outcomes, including mortality, length of hospital stay, or Clavien–Dindo classification.
Conclusions
The ASF approach was safe when performed for resectable left-sided pancreatic cancer and may help to prevent congestion of the pancreas and lessen intraoperative blood loss.




Similar content being viewed by others
References
Pericleous S, Middleton N, McKay SC, Bowers KA, Hutchins RR. Systematic review and meta-analysis of case-matched studies comparing open and laparoscopic distal pancreatectomy is it a safe procedure? Pancreas. 2012;41(7):993–1000.
Nakamura M, Wakabayashi G, Miyasaka Y, et al. Multicenter comparative study of laparoscopic and open distal pancreatectomy using propensity score-matching. J Hepato-Bil-Pan Sci. 2015;22(10):731–6.
Balduzzi A, van Hilst J, Korrel M, et al. Laparoscopic versus open extended radical left pancreatectomy for pancreatic ductal adenocarcinoma: an international propensity-score matched study. Surg Endosc. 2021;35:6949–59.
Venkat R, Edil BH, Schulick RD, Lidor AO, Makary MA, Wolfgang CL. Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique a systematic review and meta-analysis. Ann Surg. 2012;255(6):1048–59.
Strasberg SM, Drebin JA, Linehan D. Radical antegrade modular pancreatosplenectomy. Surgery. 2003;133(5):521–7.
Kantor O, Bryan DS, Talamonti MS, et al. Laparoscopic distal pancreatectomy for cancer provides oncologic outcomes and overall survival identical to open distal pancreatectomy. J Gastrointest Surg. 2017;21(10):1620–5.
Sulpice L, Farges O, Goutte N, et al. Laparoscopic Distal Pancreatectomy for pancreatic ductal adenocarcinoma time for a randomized controlled trial? Results of an all-inclusive national observational study. Ann Surg. 2015;262(5):868–74.
Sahakyan MA, Kleive D, Kazaryan AM, et al. Extended laparoscopic distal pancreatectomy for adenocarcinoma in the body and tail of the pancreas: a single-center experience. Langenbeck Arch Surg. 2018;403(8):941–8.
Yang DJ, Xiong JJ, Lu HM, et al. The oncological safety in minimally invasive versus open distal pancreatectomy for pancreatic ductal adenocarcinoma: a systematic review and meta-analysis. Sci Rep. 2019;9(1):1159.
de Rooij T, van Hilst J, van Santvoort H, et al. Minimally invasive versus open distal pancreatectomy (LEOPARD): a multicenter patient-blinded randomized controlled trial. Ann Surg. 2019;269(1):2–9.
Bjornsson B, Larsson AL, Hjalmarsson C, Gasslander T, Sandstrom P. Comparison of the duration of hospital stay after laparoscopic or open distal pancreatectomy: randomized controlled trial. Br J Surg. 2020;107(10):1281–8.
van Hilst J, de Rooij T, Klompmaker S, et al. Minimally invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): a pan-European propensity score matched study. Ann Surg. 2019;269(1):10–7.
Ban D, Garbarino GM, Ishikawa Y, et al. Surgical approaches for minimally invasive distal pancreatectomy: a systematic review. J Hepatobiliary Pancreat Sci. 2021;29:151–60.
Lee SH, Kang CM, Hwang HK, Choi SH, Lee WJ, Chi HS. Minimally invasive RAMPS in well-selected left-sided pancreatic cancer within Yonsei criteria: long-term (>median 3 years) oncologic outcomes. Surg Endosc. 2014;28(10):2848–55.
Kawabata Y, Hayashi H, Kaji S, Fujii Y, Nishi T, Tajima Y. Laparoscopic versus open radical antegrade modular pancreatosplenectomy with artery-first approach in pancreatic cancer. Langenbecks Arch Surg. 2020;405(5):647–56.
Zhang H, Li Y, Liao Q, et al. Comparison of minimal invasive versus open radical antegrade modular pancreatosplenectomy (RAMPS) for pancreatic ductal adenocarcinoma: a single center retrospective study. Surg Endosc. 2021;35(7):3763–73.
Pessaux P, Varma D, Arnaud JP. Pancreaticoduodenectomy: superior mesenteric artery first approach. J Gastrointestl Surg. 2006;10(4):607–11.
Ohigashi H, Ishikawa O, Eguchi H, et al. Early ligation of the inferior pancreaticoduodenal artery to reduce blood loss during pancreaticoduodenectomy. Hepato-Gastroenterol. 2004;51(55):4–5.
Inoue Y, Saiura A, Yoshioka R, et al. Pancreatoduodenectomy with systematic mesopancreas dissection using a supracolic anterior artery-first approach. Ann Surg. 2015;262(6):1092–101.
Sanjay P, Takaori K, Govil S, Shrikhande SV, Windsor JA. ‘Artery-first’ approaches to pancreatoduodenectomy. Brit J Surg. 2012;99(8):1027–35.
Morikawa T, Ishida M, Takadate T, et al. The superior approach with the stomach roll-up technique improves intraoperative outcomes and facilitates learning laparoscopic distal pancreatectomy: a comparative study between the superior and inferior approach. Surg Today. 2020;50(2):153–62.
Inoko K, Ebihara Y, Sakamoto K, et al. Strategic Approach to the splenic artery in laparoscopic spleen-preserving distal pancreatectomy. Surg Laparosc Endosc Percutan Tech. 2015;25(4):e122-125.
Yamamoto M, Zaima M, Yamamoto H, et al. New laparoscopic procedure for left-sided pancreatic cancer-artery-first approach laparoscopic RAMPS using 3D technique. World J Surg Oncol. 2017;15:213.
Ome Y, Hashida K, Yokota M, Nagahisa Y, Michio O, Kawamoto K. Laparoscopic radical antegrade modular pancreatosplenectomy for left-sided pancreatic cancer using the ligament of Treitz approach. Surg Endosc. 2017;31(11):4836–7.
Nagai K, Kiguchi G, Yogo A, et al. Left-posterior approach for artery-first en bloc resection in laparoscopic distal pancreatectomy for left-sided pancreatic cancer. Langenbeck Arch Surg. 2020;405(8):1251–8.
Abu Hilal M, Richardson JR, de Rooij T, Dimovska E, Al-Saati H, Besselink MG. Laparoscopic radical ‘no-touch’ left pancreatosplenectomy for pancreatic ductal adenocarcinoma: technique and results. Surg Endosc. 2016;30(9):3830–8.
Sato T, Saiura A, Inoue Y, Takahashi Y, Arita J, Takemura N. Distal pancreatectomy with en bloc resection of the celiac axis with preservation or reconstruction of the left gastric artery in patients with pancreatic body cancer. World J Surg. 2016;40(9):2245–53.
Watanabe G, Ito H, Sato T, et al. Left kidney mobilization technique during radical antegrade modular pancreatosplenectomy (RAMPS). Langenbeck Arch Surg. 2019;404(2):247–52.
Inoue Y, Saiura A, Sato T, et al. Details and outcomes of distal pancreatectomy with celiac axis resection preserving the left gastric arterial flow. Ann Surg Oncol. 2021;28:8283–94.
Nishino H, Nagakawa Y, Takishita C, et al. Safe exposure of the left renal vein during laparoscopic distal pancreatectomy for pancreatic ductal adenocarcinoma: anatomical variations and pitfalls. Surg Today. 2020;50(12):1664–71.
Takeda Y, Saiura A, Takahashi Y, Inoue Y, Mise Y, Ito H. Conservative drain management increases the incidence of grade B postoperative pancreatic fistula without increasing serious complications: does persistent drainage reflect the quality of pancreatic surgery or institutional policy? J Hepatobiliary Pancreat Sci. 2020;27(12):1011–8.
Takeda Y, Saiura A, Inoue Y, Mise Y, Ishizawa T, Takahashi Y, Ito H. Early fistulography can predict whether biochemical leakage develops to clinically relevant postoperative pancreatic fistula. World J Surg Oncol. 2019;44(9):1252–9.
Ishikawa Y, Ban D, Watanabe S, et al. Splenic artery as a simple landmark indicating difficulty during laparoscopic distal pancreatectomy. Asian J Endosc Surg. 2019;12(1):81–7.
Ohtsuka T, Ban D, Nakamura Y, et al. Difficulty scoring system in laparoscopic distal pancreatectomy. J Hepato-Bil-Pan Sci. 2018;25(11):489–97.
Cuschieri A. Laparoscopic pancreatic resections. Semin Laparosc Surg. 1996;3(1):15–20.
Takaori K, Uemoto S. Artery-first distal pancreatectomy. Digest Surg. 2016;33(4):314–9.
Sato T. Color atlas of applied anatomy of lymphatics. Japan: Nankodo; 1997.
Ott DE. Abdominal compliance and laparoscopy: a review. JSLS. 2019;23(1):e2018.00080.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interests for any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
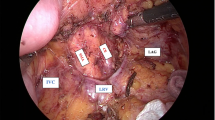
This video shows the details of laparoscopic radical antegrade modular pancreatosplenectomy (Lap-RAMPS) in a standard case. The patient was a 58-year-old man with cancer in the pancreatic tail (case 1). The tumor was located far from the superior mesenteric artery and the root of the splenic artery. The patient was diagnosed to have resectable pancreatic ductal adenocarcinoma. He was placed in the supine position with legs open, and the operation was performed using five trocars. The left adrenal gland was resected in this case to obtain sufficient tumor-free margins (MOV 177020 KB)
This video shows the details of laparoscopic radical antegrade modular pancreatosplenectomy (Lap-RAMPS) in a difficult case. The patient was a 53-year-old woman with cancer in the pancreatic body (case 2). The tumor was suspected to have invaded the splenic artery, splenic vein, and retroperitoneum but was not close to the superior mesenteric artery, celiac artery, common hepatic artery, or portal vein. The splenic artery was difficult to ligate because its origin was located deep in the peripancreatic fat. We devised the following surgical strategy: double ligation and division of the splenic artery after transection of the pancreas with addition of an extra epigastric port to adjust the angle of the approach to the splenic artery. (MOV 59947 KB)
Rights and permissions
About this article
Cite this article
Kato, T., Inoue, Y., Oba, A. et al. Laparoscopic Radical Antegrade Modular Pancreatosplenectomy with Anterocranial Splenic Artery-First Approach for Left-Sided Resectable Pancreatic Cancer (with Videos). Ann Surg Oncol 29, 3505–3514 (2022). https://doi.org/10.1245/s10434-022-11382-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-11382-x