Abstract
Purpose
Extended resection is required for pancreatic adenocarcinoma infiltrating adjacent organs and structures. The role of laparoscopy in this setting is unclear. In this study, the outcomes of extended laparoscopic distal pancreatectomy (ELDP) for pancreatic body/tail adenocarcinoma were examined.
Methods
Perioperative and oncologic data were analyzed in patients undergoing laparoscopic distal pancreatectomy (LDP) for adenocarcinoma at Oslo University Hospital. ELDP was defined as suggested by the International Study Group for Pancreatic Surgery. The outcomes of ELDP were compared to those following standard LDP (SLDP).
Results
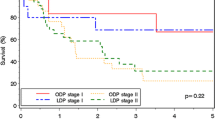
From August 2001 to June 2016, 460 consecutive patients underwent LDP for pancreatic neoplasms including 116 (25%) adenocarcinoma. SLDP and ELDP were applied in 78 and 31 patients, respectively. The adrenal gland (33%) and colon (21%) were the most frequently resected organs during ELDP. The latter was associated with larger tumor size (5.5 vs 4 cm, p = 0.03), longer operative time (236 vs 158 min, p = 0.001) and higher conversion rate (16 vs 3%, p = 0.019) compared with SLDP. Morbidity and 90-day mortality were similar. Median follow-up was 18 months. In patients with ductal adenocarcinoma, ELDP (n = 22) was associated with significantly shorter recurrence-free and overall survival than SLDP (n = 59) (6.2 vs 9.6 months, p = 0.047 and 12.9 vs 27 months, p < 0.01, respectively).
Conclusion
Although technically challenging, ELDP is feasible in patients with adenocarcinoma providing acceptable surgical outcomes. ELDP for ductal adenocarcinoma is associated with worse prognosis than SLDP, while its potential benefits over palliative care deserve further scrutiny.



Similar content being viewed by others
Abbreviations
- LDP:
-
Laparoscopic distal pancreatectomy
- SLDP:
-
Standard laparoscopic distal pancreatectomy
- ELDP:
-
Extended laparoscopic distal pancreatectomy
References
Kantor O, Bryan DS, Talamonti MS, Lutfi W, Sharpe S, Winchester DJ, Prinz RA, Baker MS (2017) Laparoscopic distal pancreatectomy for cancer provides oncologic outcomes and overall survival identical to open distal pancreatectomy. J Gastrointest Surg 21(10):1620–1625
Sahakyan MA, Kim SC, Kleive D, Kazaryan AM, Song KB, Ignjatovic D, Buanes T, Røsok BI, Labori KJ, Edwin B (2017) Laparoscopic distal pancreatectomy for pancreatic ductal adenocarcinoma: long-term oncologic outcomes after standard resection. Surgery 162(4):802–811
Sulpice L, Farges O, Goutte N, Bendersky N, Dokmak S, Sauvanet A, Delpero JR, ACHBT French Pancreatectomy Study Group (2015) Laparoscopic distal pancreatectomy for pancreatic ductal adenocarcinoma: time for a randomized controlled trial? Results of an all-inclusive national observational study. Ann Surg 262(5):868–874
Anderson KL Jr, Adam MA, Thomas S, Roman SA, Sosa JA (2017) Impact of minimally invasive vs. open distal pancreatectomy on use of adjuvant chemoradiation for pancreatic adenocarcinoma. Am J Surg 213(4):601–605
Ricci C, Casadei R, Taffurelli G, Toscano F, Pacilio CA, Bogoni S, D’Ambra M, Pagano N, di Marco MC, Minni F (2015) Laparoscopic versus open distal pancreatectomy for ductal adenocarcinoma: a systematic review and meta-analysis. J Gastrointest Surg 19(4):770–781
van Hilst J, de Rooij T, Klompmaker S et al (2017) Minimally invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): A Pan-European propensity score matched study. Ann Surg. https://doi.org/10.1097/SLA.0000000000002561
Edwin B, Sahakyan MA, Abu Hilal M et al (2017) Laparoscopic surgery for pancreatic neoplasms: the European association for endoscopic surgery clinical consensus conference. Surg Endosc 31(5):2023–2041
Rosok BI, de Rooij T, van Hilst J et al (2017) Minimally invasive distal pancreatectomy. HPB (Oxford) 19(3):205–214
Klompmaker S, van Zoggel D, Watkins AA et al (2017) Nationwide evaluation of patient selection for minimally invasive distal pancreatectomy using American College of Surgeons’ National Quality Improvement Program. Ann Surg 266(6):1055–1061
Hua Y, Javed AA, Burkhart RA, Makary MA, Weiss MJ, Wolfgang CL, He J (2017) Preoperative risk factors for conversion and learning curve of minimally invasive distal pancreatectomy. Surgery 162(5):1040–1047
Dokmak S, Fteriche FS, Aussilhou B et al (2017) The largest European single-center experience: 300 laparoscopic pancreatic resections. J Am Coll Surg 225(2):226–234.e2
Sahakyan MA, Rosok BI, Kazaryan AM et al (2016) Impact of obesity on surgical outcomes of laparoscopic distal pancreatectomy: a Norwegian single-center study. Surgery 160(5):1271–1278
Sahakyan MA, Edwin B, Kazaryan AM, Barkhatov L, Buanes T, Ignjatovic D, Labori KJ, Røsok BI (2017) Perioperative outcomes and survival in elderly patients undergoing laparoscopic distal pancreatectomy. J Hepatobiliary Pancreat Sci 24(1):42–48
de Rooij T, Besselink MG, Shamali A, Butturini G, Busch OR, Edwin B, Troisi R, Fernández-Cruz L, Dagher I, Bassi C, Abu Hilal M, DIPLOMA trial group (2016) Pan-European survey on the implementation of minimally invasive pancreatic surgery with emphasis on cancer. HPB (Oxford) 18(2):170–176
van Hilst J, de Rooij T, Abu Hilal M, Asbun HJ, Barkun J, Boggi U, Busch OR, Conlon KCP, Dijkgraaf MG, Han HS, Hansen PD, Kendrick ML, Montagnini AL, Palanivelu C, Røsok BI, Shrikhande SV, Wakabayashi G, Zeh HJ, Vollmer CM, Kooby DA, Besselink MGH (2017) Worldwide survey on opinions and use of minimally invasive pancreatic resection. HPB (Oxford) 19(3):190–204
Marangos IP, Buanes T, Rosok BI et al (2012) Laparoscopic resection of exocrine carcinoma in central and distal pancreas results in a high rate of radical resections and long postoperative survival. Surgery 151(5):717–723
Hartwig W, Vollmer CM, Fingerhut A, Yeo CJ, Neoptolemos JP, Adham M, Andrén-Sandberg A, Asbun HJ, Bassi C, Bockhorn M, Charnley R, Conlon KC, Dervenis C, Fernandez-Cruz L, Friess H, Gouma DJ, Imrie CW, Lillemoe KD, Milićević MN, Montorsi M, Shrikhande SV, Vashist YK, Izbicki JR, Büchler MW, International Study Group on Pancreatic Surgery (2014) Extended pancreatectomy in pancreatic ductal adenocarcinoma: definition and consensus of the International Study Group for Pancreatic Surgery (ISGPS). Surgery 156(1):1–14
Strasberg SM, Linehan DC, Hawkins WG (2009) The accordion severity grading system of surgical complications. Ann Surg 250(2):177–186
Mise Y, Day RW, Vauthey JN, Brudvik KW, Schwarz L, Prakash L, Parker NH, Katz MHG, Conrad C, Lee JE, Fleming JB, Aloia TA (2016) After pancreatectomy, the “90 days from surgery” definition is superior to the “30 days from discharge” definition for capture of clinically relevant readmissions. J Gastrointest Surg 20(1):77–84
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M, International Study Group on Pancreatic Surgery (ISGPS) (2016) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161(3):584–591
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Büchler MW (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142(1):20–25
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474
de Rooij T, Tol JA, van Eijck CH et al (2016) Outcomes of distal pancreatectomy for pancreatic ductal adenocarcinoma in the Netherlands: a nationwide retrospective analysis. Ann Surg Oncol 23(2):585–591
Hartwig W, Gluth A, Hinz U, Koliogiannis D, Strobel O, Hackert T, Werner J, Büchler MW (2016) Outcomes after extended pancreatectomy in patients with borderline resectable and locally advanced pancreatic cancer. Br J Surg 103(12):1683–1694
Paye F, Micelli Lupinacci R, Bachellier P, Boher JM, Delpero JR, the French Surgical Association (AFC) (2015) Distal pancreatectomy for pancreatic carcinoma in the era of multimodal treatment. Br J Surg 102(3):229–236
Sahakyan MA, Kazaryan AM, Rawashdeh M, Fuks D, Shmavonyan M, Haugvik SP, Labori KJ, Buanes T, Røsok BI, Ignjatovic D, Abu Hilal M, Gayet B, Kim SC, Edwin B (2016) Laparoscopic distal pancreatectomy for pancreatic ductal adenocarcinoma: results of a multicenter cohort study on 196 patients. Surg Endosc 30(8):3409–3418
Panzeri F, Marchegiani G, Malleo G, Malpaga A, Maggino L, Marchese T, Salvia R, Bassi C, Butturini G (2017) Distal pancreatectomy associated with multivisceral resection: results from a single Centre experience. Langenbeck's Arch Surg 402(3):457–464
Roch AM, Singh H, Turner AP, Ceppa EP, House MG, Zyromski NJ, Nakeeb A, Schmidt CM (2015) Extended distal pancreatectomy for pancreatic adenocarcinoma with splenic vein thrombosis and/or adjacent organ invasion. Am J Surg 209(3):564–569
Shoup M, Conlon KC, Klimstra D, Brennan MF (2003) Is extended resection for adenocarcinoma of the body or tail of the pancreas justified? J Gastrointest Surg 7(8):946–952 discussion 52
Conroy T, Desseigne F, Ychou M, Bouché O, Guimbaud R, Bécouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de la Fouchardière C, Bennouna J, Bachet JB, Khemissa-Akouz F, Péré-Vergé D, Delbaldo C, Assenat E, Chauffert B, Michel P, Montoto-Grillot C, Ducreux M, Groupe Tumeurs Digestives of Unicancer, PRODIGE Intergroup (2011) FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 364(19):1817–1825
Christein JD, Kendrick ML, Iqbal CW et al (2005) Distal pancreatectomy for resectable adenocarcinoma of the body and tail of the pancreas. J Gastrointest Surg 9(7):922–927
Kleeff J, Diener MK, Z'Graggen K et al (2007) Distal pancreatectomy: risk factors for surgical failure in 302 consecutive cases. Ann Surg 245(4):573–582
Goh BK, Tan YM, Cheow PC et al (2008) Outcome of distal pancreatectomy for pancreatic adenocarcinoma. Dig Surg 25(1):32–38
Hartwig W, Hackert T, Hinz U, Hassenpflug M, Strobel O, Büchler MW, Werner J (2009) Multivisceral resection for pancreatic malignancies: risk-analysis and long-term outcome. Ann Surg 250(1):81–87
Seeliger H, Christians S, Angele MK, Kleespies A, Eichhorn ME, Ischenko I, Boeck S, Heinemann V, Jauch KW, Bruns CJ (2010) Risk factors for surgical complications in distal pancreatectomy. Am J Surg 200(3):311–317
Hasselgren K, Halldestam I, Fraser MP et al (2016) Does the introduction of laparoscopic distal pancreatectomy jeopardize patient safety and well-being? Scand J Surg 105(4):223–227
Author information
Authors and Affiliations
Contributions
Study conception and design: M.A.S., K.J.L., B.I.R., B.E.; acquisition of data: M.A.S., D.K., A.M.K., D.L.A., D.I.; analysis and interpretation of data: M.A.S., D.K., K.J.L., B.E.; drafting of manuscript: M.A.S., B.E.; critical revision of manuscript: D.K., A.M.K., D.L.A., D.I., K.J.L., B.I.R.
Corresponding author
Ethics declarations
The study was approved by the Institutional Data Protection Officer.
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Sahakyan, M.A., Kleive, D., Kazaryan, A.M. et al. Extended laparoscopic distal pancreatectomy for adenocarcinoma in the body and tail of the pancreas: a single-center experience. Langenbecks Arch Surg 403, 941–948 (2018). https://doi.org/10.1007/s00423-018-1730-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1730-x