Abstract
Background
Nipple discharge is the third most frequent complaint of women attending rapid diagnostic breast clinics. Nipple smear cytology remains the single most used diagnostic method for investigating fluid content. This study aimed to conduct a systematic review and meta-analysis of the diagnostic accuracy of nipple discharge fluid assessment.
Methods
The study incorporated searches for studies interrogating the diagnostic data of nipple discharge fluid cytology compared with the histopathology gold standard. Data from studies published from 1956 to 2019 were analyzed. The analysis included 8648 cytology samples of women with a presenting complaint of nipple discharge. Both hierarchical and bivariate models for diagnostic meta-analysis were used to attain overall pooled sensitivity and specificity.
Results
Of 837 studies retrieved, 45 fulfilled the criteria for inclusion. The diagnostic accuracy of the meta-analysis examining nipple discharge fluid had a sensitivity of 75 % (95 % confidence interval [CI], 0.74–0.77) and a specificity of 87 % (95 % CI, 0.86–0.87) for benign breast disease. For breast cancer, it had a sensitivity of 62 % (95 % CI, 0.53–0.71) and a specificity 71 % (95 % CI, 0.57–0.81). Furthermore, patients presenting with blood-stained discharge yielded an overall malignancy rate of 58 % (95 % CI, 0.54–0.60) with a positive predictive value (PPV) of 27 % (95 % CI, 0.17–0.36).
Conclusions
Pooled data from studies encompassing nipple discharge fluid assessment suggest that nipple smear cytology is of limited diagnostic accuracy. The authors recommend that a tailored approach to diagnosis be required given the variable sensitivities of currently available tests.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Nipple discharge may arise from both pathologic and physiologic processes and accounts for 3 % to 9 % of referrals to the breast clinic, the equivalent of 16,000 to 48,000 presentations each year in the United Kingdom.1 Spontaneous single-duct discharge is widely accepted as a clinical sign warranting further investigation, often requiring surgical management in the form of a microdochectomy or total duct excision to acquire a definitive diagnosis.2 A rising incidence of breast cancer3 has led to an urgent need for the development of rapid, reliable, and cost-effective methods of diagnosing breast cancer. Importantly, in the midst of a SARS-Cov-2 global pandemic, with everchanging hospital policies limiting exposure to various parts of the hospital, restrictions on the number of diagnostic methods offered to patients and the need to avoid unnecessary surgical intervention, a single noninvasive point-of-care diagnostic test to exclude breast carcinoma has become increasingly important.
In current practice, patients presenting with nipple discharge undergo triple assessment (clinical assessment, imaging, and pathology), which can include cytopathology prepared as a nipple smear. Clinical investigation of patients with pathologic nipple discharge (PND), defined as spontaneous single-duct and often blood-stained discharge, includes mammography, ultrasonography, magnetic resonance imaging (MRI), and even galactography to direct visualization of the ductal system ± ductal lavage. Although a recently published meta-analysis4 compared the diagnostic accuracy of different imaging methods used for the investigation of PND, the capacity of cytology to interrogate PND comprehensively for both benign and malignant diagnoses is yet to be reviewed systematically.
Nipple-smear cytology, still currently performed in many breast centers around world, is used as part of the workup for patients presenting with PND. Its role as an early detection tool for asymptomatic women also has been investigated5,6 given the feasibility of nipple aspirate fluid production by massage,7 negative suction devices (automated or manual),8 or ductal lavage.9 The diagnostic utility of nipple fluid cytology has been deliberated over the years.10,11,12 To date, however, the diagnostic accuracy of nipple fluid cytology for both benign and malignant diagnoses has not been comprehensively quantified using meta-analytical techniques.
To this end, the primary aim of this study was to perform a systematic review and meta-analysis to compute the diagnostic accuracy of nipple discharge fluid cytology for symptomatic women presenting to the breast clinic. The secondary aim was to investigate the variations in the management of PND in terms of presentation, imaging, pathology, and surgery as well as the diagnostic accuracy of other methods including ultrasound, MRI, and ductoscopy.
Methods
An electronic search using MEDLINE, EMBASE, and SCOPUS was performed until March 2020. Multiple methods were used to retrieve papers, namely, submitting requests through the authors’ academic institution and the British Library, writing to the editor of the journal, contacting the corresponding author, and placing requests through ResearchGate.
Search terms included “nipple discharge fluid” and “cytology” in all their forms. The following Medical Subject headings (MeSH) and key words were used in combination with AND/ OR operators: “nipple discharge” OR “breast” adjacent to “discharge” by up to three words OR “nipple” adjacent to “discharge” by up to three words AND cytodiagnosis OR cytoproliferation OR cytolog* OR cytodiagnos* OR papanicolaou. Title and abstract review then was performed according to the predefined inclusion and exclusion criteria defined in the following sections.
Inclusion Criteria
Only clinical studies with primary data on the diagnostic accuracy of nipple discharge fluid cytology versus ductal histology were included. Foreign language studies were included if an English language translation was retrievable. Studies were included if they yielded diagnostic information on benign and/or malignant diagnoses from cytology and on pathologic nipple discharge of all clinical descriptions (i.e., single duct, blood-stained, clear). Regarding acquisition of fluid, studies that included direct expression of discharge as well as dutoscopy to retrieve a fluid sample were included if patients presented with pathologic nipple discharge.
Exclusion Criteria
Studies were excluded if a full English text was not available, or if a translation of the text into English was irretrievable. All animal studies, case reports, and male breast cancer studies were excluded. Studies with pregnancy-associated breast cancer also were excluded, as well as papers reporting on brush cytology only.
Study Quality
Study quality (Table 1, Supplement 1) was evaluated by two independent investigators (N.J and S.K) using the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) scoring system checklist.13 All QUADAS-2 questions were included in quality scoring, providing a maximum score of 14.13 Each question was given a score of 0, 1, or 2 depending on whether the question was unanswered, unclearly answered, or fully answered. For studies to be considered accurately conducted and analyzed, the they had to report patient demographics, the presenting complaint, a clear explanation of the methods of processing and analyzing the nipple fluid smear, and whether an operative histologic sample or core biopsy was used for comparison. Whether the cytopathologist was blinded to the clinical results also was documented.
Data Collection
An independent assessment by two investigators (N.J and S.K) was conducted using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia).14 Any conflicts were discussed and resolved with an explanation of “yes,” “no,” or “uncertain.” All “uncertain” cases underwent full-text screening, and justification for inclusion or exclusion was documented within the system (Fig. S1) and discussed with senior authors (H.A and D.R.L).
Demographic and accuracy data from the included studies were recorded using a predefined spreadsheet (Excel). In particular, data were extracted on the first author and year of publication, number of patients, number of cytology samples, mean age, QUADAS-2 score, method of collection, sensitivity, specificity, true-positives, false-positives, true-negatives, false-negatives, and positive predictive values.
After data extraction, the studies were subdivided by their method of collection (e.g., ductal lavage, manual compression) for subgroup analysis of sensitivity and specificity by method. Benign cytology was classified as “benign” or “Cn2,” representing “cytology for nipple fluid” adapted from the five-number grading system for fine-needle aspirate cytology of breast tissue as follows: insufficient (C1), benign (C2), atypical/equivocal (C3), suspicious (C4), or malignant (C5). Atypical and malignant cytology (including ductal carcinoma in situ [DCIS]/lobular carcinoma in situ [LCIS]) was defined using the numeric grading system Cn3–5 to calculate a relative sensitivity and specificity with an accompanying diagnostic accuracy curve and using Cn5 only to calculate the absolute sensitivity. Further analysis was performed using Cn2–3 to denote a benign diagnosis and Cn4–5 to denote a malignant diagnosis (Table 1 in Supplement 2).
Meta-Analysis
Sensitivity, specificity, true-positive, true-negative, false-positive, false-negative, and positive predictive value (PPV) of cytology results were assessed for each paper, creating an overall sensitivity and specificity for both benign and malignant diagnoses. Pooled diagnostic sensitivity and specificity were calculated using 33 of the 45 studies reporting benign outcomes and 39 of the 45 studies reporting malignant outcomes alike (all studies with sensitivities of 0 were excluded from the calculation). In addition, these papers were interrogated for all comparative imaging and diagnostic methods. In particular, the overall malignancy rate for blood-stained discharge as well as the pooled sensitivity and specificity of mammography, ultrasonography, MRI, and galactography (or ductography) all were calculated independently.
Summary estimates of sensitivity, specificity, and area under the curve (AUC) data were attempted using a bivariate model for diagnostic meta-analysis. Independent diagnostic metrics and their differences were calculated and pooled through DerSimonian and Laird random-effects modeling.15 This considered both between-study and within-study variances, which contributed to study-weighting. Study-specific estimates as well as 95 % confidence intervals (CIs) were computed and represented on forest plots. Statistical heterogeneity was determined by the I2 statistic whereby less than 30 % was low, 30 % to 60 % was moderate, and more than 60 % was considered high. Analyses were performed using Stata version 15 (Stata Corp LP, College Station, TX, USA). Probability values (p values) of 0.05 or lower were considered statistically significant.
Results
For initial review, 837 studies were retrieved from the databases (PRISMA diagram; Supplement 1; Fig. 1). After the abstract and title review, 213 studies met the inclusion criteria for full text-review, with 168 studies excluded. The main reasons for exclusion were no English translation of the article (n = 70), lack of nipple discharge cytology data (n = 45), abstract only (n = 15), nipple discharge cytology data without gold standard comparison (n = 14), duplication of the dataset (n = 12), and merging of fine-needle aspirate cytology and nipple smear cytology (n = 7). Other exclusions ruled out patients not presenting exclusively with nipple discharge (n = 2), ductal lavage cytology with no simple nipple discharge cytology (n = 2), paper not available (n = 2), nipple aspirate fluid cytology rather than nipple discharge cytology (n = 2), case report (n = 1), and heterogeneous analysis of both male and female cytology data (n = 1).
The meta-analysis included 45 studies, all of which contained clinical data on the diagnosis acquired from nipple discharge cytology, which was correlated with their histology. The publication dates included in these studies ranged from 1956 to 2019. The mean or median age was available for 30 of the 45 studies, with an age range of 14 to 94 years. The mean age of the included patients was 48.74 ± 4.66 years.
Overall, the analysis included 8648 cytology samples. From the available data, sensitivity and specificity for nipple fluid smear cytology was either extracted or calculated. The computed relative and absolute sensitivity, PPV, and negative predictive value (NPV) for each study are included in Table 1 for malignant diagnoses. Table 2 presents the data for all non-cytologic diagnostic methods including sensitivity, specificity, PPVs, and NPVs. The diagnostic accuracy meta-analysis of nipple aspirate fluid showed a sensitivity of 0.75 (95 % CI, 0.74–0.77) and a specificity of 0.87 (95 % CI, 0.86–0.87) for a benign diagnosis (Cn2) (Fig. 1A). For breast carcinoma (Cn3/4/5), the meta-analysis showed a relative sensitivity of 0.62 (95 % CI, 0.53–0.71) and a specificity 0.71 (95 % CI,0.57–0.81) (Fig. 1B1). When only Cn5 cytology was considered, the absolute sensitivity of cytology was 0.35 (95 % CI, 0.26–0.44), and the specificity was 1.00 (95 % CI, 1.00–1.00) (Fig. 1B2). The overall diagnostic accuracy of nipple discharge cytology for a malignant diagnosis, including both prediction and confidence contours, is depicted in Fig. 2A and B, with the size of each circle representing the weight assigned to each study.
A Forest plots depicting the overall sensitivity (left) and specificity (right) of nipple discharge fluid cytology for patients with benign diagnoses classified as Cn2. B1 Forest plots demonstrating the overall relative sensitivity (left) and specificity (right) of nipple discharge fluid cytology for patients with a malignancy (Cn3–5). B2 Absolute sensitivity (left) and specificity (right) of nipple discharge cytology for Cn5 alone
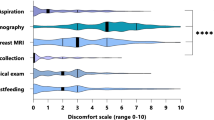
Other diagnostic methods yielded a range of sensitivities, specificities, and PPVs. Ultrasound was observed to have a pooled sensitivity of 0.70 (95 % CI, 0.60–0.80) and a lower pooled specificity of 0.58 (95 % CI, 0.24–0.75), with a PPV of 0.78 (95 % CI, 0.56–0.99) (Fig. 3A). Mammogram yielded a low pooled sensitivity of 0.38 (95 % CI, 0.23–0.52), a higher pooled specificity of 0.79 (95 % CI, 0.69–0.90), and a PPV of 0.49 (95 % CI, 0.24–0.75) (Fig. 3 B). For MRI, a pooled sensitivity of 0.70 (95 % CI, 0.61–0.78) and a pooled specificity of 0.45 (95 % CI, 0.20–0.70) together with a PPV of 0.57 (95 % CI, 0.55–0.79) were observed (Fig. 3C). Galactography yielded a pooled sensitivity of 0.62 (95 % CI, 0.13–1.11), a pooled specificity of 0.52 (95 % CI, 0.04–1.00), and a PPV of 0.48 (95 % CI, 0.00–0.95) (Fig. 3D). Finally, for blood-stained discharge, the malignancy rate was 0.57 (95 % CI, 0.54–0.60), signifying that 57 % of those presenting with a blood-stained nipple discharge went on to receive a malignant diagnosis. Moreover, the calculated PPV of a blood-stained nipple discharge cytology was 0.27 (95 % CI, 0.17–0.36) (Supplement 1; Fig. 2).
Forest plots depicting the individual pooled sensitivity and specificity of other diagnostic methods: ultrasonography (8 studies), mammography (8 studies), magnetic resonance imaging (MRI) (8 studies), galactrography (8 studies). A1 Sensitivity of ultrasound. A2 Specificity of ultrasound. B1 Sensitivity of mammogram. B2 Specificity of mammogram. C1 Sensitivity of magnetic resonance imaging (MRI). C2 Specificity of MRI. D1 Sensitivity of galactography. D2 Specificity of galactography
Discussion
This meta-analysis integrated the diagnostic accuracy of nipple discharge fluid cytology and diagnostic imaging across published clinical studies. The primary finding was that the sensitivity of PND evaluation for the detection of both benign disease and breast cancer is poor. The sensitivity was respectively 75 % (95 % CI, 0.74–0.77) and 62 % (95 % CI, 053–0.71), and the specificity was respectively 87 % (95 % CI, 0.86–0.88) and 71 % (95 % CI, 0.57–0.81). Overall, these specificity and sensitivity data are echoed across individual studies of patients presenting with symptomatic nipple discharge.16,17 Interestingly, the diagnostic accuracy of nipple cytologic analysis of patients with PND is similar to that of other diagnostic tests, with sensitivities ranging from a high of 70 % for both ultrasound and MRI to a specificity high of 79 % for mammography. Critically, in the case of a patient whose sole symptom is nipple discharge, no individual diagnostic test, whether imaging or cytologic, yielded a sensitivity or specificity high enough for its use as a stand-alone test.
Interestingly, the presence of blood did not appear to predict a breast cancer diagnosis (PPV, 27 %; 95 % CI, 0.17–0.36), and the high association of blood and malignancy (57 %) may be confounded by studies including only data on patients with blood and malignancy.18,19 Therefore, despite reports suggesting the importance of color or presence of blood,18,20 the clinical utility of nipple fluid assessment is limited. For both benign and malignant diagnoses, the frequent lack of cellular material makes it difficult to analyze abnormalities. Nipple fluid cytology of the breast is deemed increasingly difficult because cancer cells from the breast tend to be both smaller and less pleomorphic than their counterparts from other parts of the body.21 Moreover, cytologic criteria for malignancy are less obvious in nipple discharge smears because they have a tendency to contain degenerated cells.22 In addition, interpretation may be subject to inter-reporter variability or relative inexperience, as well as the presence of atypical cellular changes unrelated to a malignancy, leading to either a higher degree of false-positive or false-negative findings.
Despite the challenges associated with nipple cytologic analysis and notwithstanding the small proportion of patients presenting with PND who will go on to receive a breast cancer diagnosis,23 it may be the only presenting clinical symptom of a breast cancer and therefore cannot be dismissed. Although cytology is no longer used in some centers, nipple smear cytology continues to be used in clinical practice globally. The rationale behind its use is that the majority of breast cancers arise from the epithelial lining of the terminal ducts and thus are denoted as invasive ductal carcinomas.24 Therefore, it is accepted that nipple discharge fluid directly reflects the tumor microenvironment and for high-risk individuals indicates the lead up to cancer.25 However, it also has been shown that not all ducts drain to the nipple surface,26 suggesting that even if adequate, cytologic analysis could miss a proportion of breast cancers.
A further challenge is the range of cellular findings and whether this is representative of benign or malignant disease. For example, papillary clusters can be a cytologic finding of both benign and malignant pathologies.27,28
Because the reviewed diagnostic methods have limited ability to confirm or exclude a breast cancer diagnosis for patients presenting with PND, surgical intervention in the form of a microdochectomy or total duct excision is required for a definitive diagnosis or adequate reassurance. Indeed, the findings of this meta-analysis might suggest that such patients could undergo imaging to exclude mass lesions, including possibly MRI.29 However, a large proportion of patients go on to have a microdochectomy because a normal MRI does not exclude an adjacent or underlying malignancy.29 Therefore, it may be argued in light of the results from the current meta-analysis that cytology is no longer necessary because it adds very little further diagnostic information. An alternative pathway for the management of single-duct nipple discharge could instead rely on clinical assessment using ultrasound ± mammogram followed by an MRI, with a diagnostic microdochectomy if radiologic findings are unremarkable.
Moreover, our review suggests that no single diagnostic technique can be used in isolation, even amid these changing times, with the need to minimize hospital appointments and unnecessary surgery. It does, however, suggest scope for development of a more comprehensive diagnostic tool to assess nipple discharge. With the explosion of metabolomics during the last decade yielding promising results,7,30,31,32 the interrogation of tiny amounts of fluid such as nipple discharge fluid using newer technology must be investigated, with awareness of the need for high diagnostic accuracy, fast turnaround time, and reproducibility.
The great strength of this meta-analysis was its comprehensive review of nipple cytology diagnostics toward pooled diagnostic accuracy. The decision to include cytology papers from such a large time span was intended to reflect the longevity of the technique’s use and its diagnostic accuracy in the context of evolving diagnostic practices. Moreover, this is the first review to interrogate the use of nipple smear cytology to detect both benign and malignant breast disease and to compare its performance with that of other breast imaging methods. The most recently published comparable review by Filipe et al.4 considers only malignant diagnostics and independently compares other imaging methods for which only histopathology is available. In addition, their study overlooked literature from which guidelines were drawn.33,34,35 Comparing other imaging methods and cytology within the same patient cohorts reduces patient selection bias and therefore reflects more accurately on the diagnostic capabilities of each technique in the same settings during the time period.
A potential limitation of the current review was in the quality of the papers retrieved. The QUADAS scoring ranged from 4 to 14 and reflected the variable nature of the study design and its relevance to the review question. For example, the study included papers reporting only the cytology results of patients presenting with bloody nipple discharge who had a cancer diagnosis. It is evident that the sensitivity was falsely elevated because the negative results are not disclosed in the paper.36 Similarly, not all papers had a strict definition of what was considered as a pathologic nipple discharge, so higher rates of “physiologic” discharge may have been included within the presenting numbers.
Conclusions
Pooled data from the included studies demonstrated that the diagnostic accuracy of nipple discharge cytology is limited and has poor sensitivity for symptomatic women. The color of nipple discharge fluid, although yielding a high positive malignancy rate, demonstrated a poor PPV. Emerging technologies for analysis of nipple fluid must have a higher diagnostic accuracy than nipple cytology while offering advantages in terms of cost, reproducibility, user dependency, and turnaround time.
References
Clark S, Agrawal A, Scutt F, Laws S, Graga T, Laban CJ. The investigation and management of unilateral nipple discharge by breast units across Wessex. EJSO. 2019;45:904.
Chen L, Zhou W-B, Zhao Y, et al. Bloody nipple discharge is a predictor of breast cancer risk: a meta-analysis. Breast Cancer Rest Treat. 2012;132:9–14.
Cancer Research UK. Breast Cancer Statistics. Retrieved 30 January 2021 at https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer#heading-Five.
Filipe MD, Patuleia SI, de Jong VM, Vriens MR, van Diest PJ, Witkamp AJ. A network meta-analysis for the diagnostic approach to pathological nipple discharge. Clin Breast Cancer. 2020;20(6):e723–48.
Wrensch MR, Petrakis NL, Miike R, et al. Breast cancer risk in women with abnormal cytology in nipple aspirates of breast fluid. J Natl Cancer Inst. 2001;93:1791–8.
Wrensch MR, Petrakis NL, King EB, et al. Breast cancer incidence in women with abnormal cytology in nipple aspirates of breast fluid. Am J Epidemiol. 1992;135:130–41.
Shaheed SU, Tait C, Kyriacou K, Linforth R, Salhab M, Sutton C. Evaluation of nipple aspirate fluid as a diagnostic tool for early detection of breast cancer. Clin Proteomics. 2018;15:3.
Chen SC, Johncox VE, Godoski J, Quay SC. Analytical validation of the forecyte breast health test. J Am Soc Cytopathol. 2013;2(1 Suppl 1):S10.
Twelves D, Nerurkar A, Osin P, Ward A, Isacke CM, Gui GP. The feasibility of nipple aspiration and duct lavage to evaluate the breast duct epithelium of women with increased breast cancer risk. Eur J Cancer. 2013;49:65–71.
Morrogh M, Park A, Elkin EB, King TA. Lessons learned from 416 cases of nipple discharge of the breast. Am J Surg. 2010;200:73–80.
Dolan RT, Butler JS, Kell MR, Gorey TF, Stokes MA. Nipple discharge and the efficacy of duct cytology in evaluating breast cancer risk. Irish J Med Sci. 2011;180:252–8.
Kooistra B, Wauters C, Van de Ven S, Strobbe L. The diagnostic value of nipple discharge cytology in 618 consecutive patients. EJSO. 2009;35:573–7.
Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36.
Covidence systematic review software [program]: Veritas Health Innovation, Melbourne, Australia.
DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28:105–14.
Dinkel H-P, Gassel AM, Müller T, et al. Galactography and exfoliative cytology in women with abnormal nipple discharge. Obstet Gynecol. 2001;97:625–9.
Kan W, Chen C, Kwong AJHKMJ. Implications of nipple discharge in Hong Kong Chinese women. Hong Kong Med J. 2018;24:18–24.
El-Daly H, Gudi M. Evaluation of nipple discharge cytology and diagnostic value of red blood cells in cases with negative cytology: a cytohistologic correlation. Acta Cytologica. 2010;54:560–2.
Kaplan R, Hoda SA, Hoda RS. Cytological evaluation of bloody nipple discharge fluid. Diagn Cytopathol. 2013;41:183–5.
Cabioglu N, Hunt KK, Singletary SE, et al. Surgical decision-making and factors determining a diagnosis of breast carcinoma in women presenting with nipple discharge. J Am Coll Surg. 2003;196:354–64.
Sakorafas G. Nipple discharge: current diagnostic and therapeutic approaches. Cancer Treat Rev. 2001;27:275–82.
Dunn J, Lucarotti M, Wood S, Mumford A, Webb A. Exfoliative cytology in the diagnosis of breast disease. Br J Surg. 1995;82:789–91.
Seltzer MH. Breast complaints, biopsies, and cancer correlated with age in 10,000 consecutive new surgical referrals. Breast J. 2004;10:111–7.
Wellings S, Jensen HM. On the origin and progression of ductal carcinoma in the human breast. J Natl Cancer Inst. 1973;50:1111–8.
Djuric Z, Chen G, Ren J, et al. Effects of high fruit-vegetable and/or low-fat intervention on breast nipple aspirate fluid micronutrient levels. Cancer Epidemiol Biomarkers Prev. 2007;16:1393–9.
Wang SC, Gombos E, Birdwell RL, Berg WA. Diagnostic Imaging Breast. 3rd edn. London: Elsevier; 2019.
Ueng SH, Mezzetti T, Tavassoli FA. Papillary neoplasms of the breast: a review. Arch PatholLabMed. 2009;133:893–907.
Pal SK, Lau SK, Kruper L, et al. Papillary carcinoma of the breast: an overview. Breast Cancer Res Treat. 2010;122:637–45.
Lanitis S, Filippakis G, Thomas J, Christofides T, Al Mufti R, Hadjiminas DJ. Microdochectomy for single-duct pathologic nipple discharge and normal or benign imaging and cytology. The Breast. 2008;17:309–13.
Do Matos CL, Marian C, Varghese RS, et al. Metabolomic profiling of breast tumors using ductal fluid. Int J Oncol. 2016;49:2245–54.
Sauter ER, Wagner-Mann C, Ehya H, Klein-Szanto A. Biologic markers of breast cancer in nipple aspirate fluid and nipple discharge are associated with clinical findings. Cancer Detect Prev. 2007;31:50–8.
Chan AA, Bashir M, Rivas MN, et al. Characterization of the microbiome of nipple aspirate fluid of breast cancer survivors. Sci Rep. 2016;6:150.
Walker J, Sanclison A. The cytological examination of nipple discharges as a diagnostic aid. Scot Med J. 1958;3:297–304.
Rimsten A, Skoog V, Stenkvist B. On the significance of nipple discharge in the diagnosis of breast disease. Acta Chir Scand. 1976;142:513.
Leis HP. Management of nipple discharge. World J Surg. 1989;13:736–42.
Markopoulos C, Mantas D, Kouskos E, et al. Surgical management of nipple discharge. Eur J Gynaecol Oncol. 2006;27:275–8.
Alcock C, Layer GT. Predicting occult malignancy in nipple discharge. ANZ J Surg. 2010;80:646–9.
Bauer RL, Eckhert KH, Nemoto T. Ductal carcinoma in situ-associated nipple discharge: a clinical marker for locally extensive disease. Ann Surg Oncol. 1998;5:452–5.
Cabioglu N, Krishnamurthy S, Kuerer HM, et al. Feasibility of breast-conserving surgery for patients with breast carcinoma associated with nipple discharge. Cancer. 2004;101:508–17.
Carty N, Mudan S, Ravichandran D, Royle G, Taylor I. Prospective study of outcome in women presenting with nipple discharge. Ann R Coll Surg Engl. 1994;76:387.
Çetin K, Sıkar HE. Evaluation and management of pathological nipple discharges without using intraductal imaging methods. Irish J Med Sci (1971–). 2019;2:1–10.
Ciatto S, Bravetti P, Cariaggi P. Significance of nipple discharge clinical patterns in the selection of cases for cytologic examination. Acta Cytologica. 1986;30:17–20.
Cilotti A, Campassi C, Bagnolesi P, Moretti M, Macaluso A, Bartolozzi C. Pathologic nipple discharge: high-resolution vs conventional ultrasound in the evaluation of ductal disease. Breast Dis. 1996;1:1–13.
Denewer A, El-Etribi K, Nada N, El-Metwally M. The role and limitations of mammary ductoscope in management of pathologic nipple discharge. Breast J. 2008;14:442–9.
Florio MG, Manganaro T, Pollicino A, Scarfo P, Micali B. Surgical approach to nipple discharge: a ten-year experience. J Surg Oncol. 1999;71:235–8.
Fung A, Rayter Z, Fisher C, King D, Trott P. Preoperative cytology and mammography in patients with single-duct nipple discharge treated by surgery. Br J Surg. 1990;77:1211–2.
Funovics M, Philipp M, Lackner B, Fuchsjaeger M, Funovics P, Metz V. Galactography: method of choice in pathologic nipple discharge? Eur Radiol. 2003;13:94–9.
Groves A, Carr M, Wadhera V, Lennard T. An audit of cytology in the evaluation of nipple discharge: a retrospective study of 10 years’ experience. The Breast. 1996;5:96–9.
Grunwald S, Bojahr B, Schwesinger G, et al. Mammary ductoscopy for the evaluation of nipple discharge and comparison with standard diagnostic techniques. J Minim Invasive Gynecol. 2006;13:418–23.
Hahn M, Fehm T, Solomayer EF, et al. Selective microdochectomy after ductoscopic wire marking in women with pathological nipple discharge. BMC Cancer. 2009;9:151.
Hou M, Tsai K, Lin H, Chai C, Liu C, Huang T. A simple intraductal aspiration method for cytodiagnosis in nipple discharge. Acta Cytologica. 2000;44:1029–34.
Hou M-F, Tsai K-B, Ou-Yang F, et al. Is a one-step operation for breast cancer patients presenting nipple discharge without palpable mass feasible? The Breast. 2002;11:402–7.
Hünerbein M, Dubowy A, Raubach M, Gebauer B, Topalidis T, Schlag P. Gradient index ductoscopy and intraductal biopsy of intraductal breast lesions. Am J Surg. 2007;194:511–4.
Jacobs VR, Kiechle M, Plattner B, Fischer T, Paepke S. Breast ductoscopy with a 0.55-mm mini-endoscope for direct visualization of intraductal lesions. J Minim Invasive Gnecol. 2005;12:359–64.
Kalu ON, Chow C, Wheeler A, Kong C, Wapnir I. The diagnostic value of nipple discharge cytology: breast imaging complements predictive value of nipple discharge cytology. J Surg Oncol. 2012;106:381–5.
Kjellgren O. Cytologic studies of nipple discharge. Acta Radiol. 1956;3:753–67.
Kuroi K, Osaki A, Kawami H, Murakami S, Toge T. Usefulness of endoscopic examination for patients with nipple discharge. The Cancer J. 1997;10:112–5.
Lee WY. Cytology of abnormal nipple discharge: a cyto-histological correlation. Cytopathology. 2003;14:19–26.
Matsunaga T, Misaka T, Hosokawa K, et al. Intraductal approach to the detection of intraductal lesions of the breast. Breast Cancer Res Treat. 2009;118:9–13.
Montroni I, Santini D, Zucchini G, et al. Nipple discharge: is its significance as a risk factor for breast cancer fully understood? Observational study including 915 consecutive patients who underwent selective duct excision. Breast Cancer Res Treat. 2010;123:895–900.
Ohlinger R, Stomps A, Paepke S, et al. Ductoscopic detection of intraductal lesions in cases of pathologic nipple discharge in comparison with standard diagnostics: the German multicenter study. Oncol Res Treat. 2014;37:628–32.
Pritt B, Pang Y, Kellogg M, St. John T, Elhosseiny A. Diagnostic value of nipple cytology: study of 466 cases. Cancer. 2004;102:233–8.
Simmons R, Adamovich T, Brennan M, et al. Nonsurgical evaluation of pathologic nipple discharge. Ann Surg Oncol. 2003;10:113–6.
Shen K-W, Wu J, Lu J-S, et al. Fiberoptic ductoscopy for breast cancer patients with nipple discharge. Surg Endosc. 2001;15(11):1340–5.
Yang X, Li H, Gou J, et al. The role of breast ductoscopy in evaluation of nipple discharge: a Chinese experience of 419 patients. Breast J. 2014;20:388–93.
Yamamoto D, Shoji T, Kawanishi H, et al. A utility of ductography and fiberoptic ductoscopy for patients with nipple discharge. Breast Cancer Res Treat. 2001;70:103–8.
Grunwald S, Heyer H, Paepke S, et al. Diagnostic value of ductoscopy in the diagnosis of nipple discharge and intraductal proliferations in comparison to standard methods. Onkologie. 2007;30:243–8.
Castellano I, Metovic J, Balmativola D, et al. The impact of malignant nipple discharge cytology (NDc) in surgical management of breast cancer patients. PLoS One. 2017;12:e0182073.
Acknowledgments
The research was funded by the NIHR Imperial Biomedical Research Centre (BRC). The study had no commercial interest and no external financial or material support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Natasha Jiwa is a PhD candidate investigating nipple biofluid in the early detection of breast cancer under the supervision of D. R. Leff and Z. Takats. The remaining authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiwa, N., Kumar, S., Gandhewar, R. et al. Diagnostic Accuracy of Nipple Discharge Fluid Cytology: A Meta-Analysis and Systematic Review of the Literature. Ann Surg Oncol 29, 1774–1786 (2022). https://doi.org/10.1245/s10434-021-11070-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-11070-2