Abstract
Background
Surgical delays are associated with invasive cancer for patients with ductal carcinoma in situ (DCIS). During the Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) pandemic, neoadjuvant endocrine therapy (NET) was used as a bridge until postponed surgeries resumed. This study sought to determine the impact of NET on the rate of invasive cancer for patients with a diagnosis of DCIS who have a surgical delay compared with those not treated with NET.
Methods
Using the National Cancer Database, the study identified women with hormone receptor-positive (HR+) DCIS. The presence of invasion on final pathology was evaluated after stratifying by receipt of NET and by intervals based on time from diagnosis to surgery (≤30, 31–60, 61–90, 91–120, or 121–365 days).
Results
Of 109,990 women identified with HR+ DCIS, 276 (0.3%) underwent NET. The mean duration of NET was 74.4 days. The overall unadjusted rate of invasive cancer was similar between those who received NET ((15.6%) and those who did not (12.3%) (p = 0.10). In the multivariable analysis, neither the use nor the duration of NET were independently associated with invasion, but the trend across time-to-surgery categories demonstrated a higher rate of upgrade to invasive cancer in the no-NET group (p < 0.001), but not in the NET group (p = 0.97).
Conclusions
This analysis of a pre-COVID cohort showed evidence for a protective effect of NET in HR+ DCIS against the development of invasive cancer as the preoperative delay increased, although an appropriately powered prospective trial is needed for a definitive answer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The status of ductal carcinoma in situ (DCIS) of the breast as an obligate precursor of invasion has recently been in dispute. Although the natural history of DCIS is not definitively known, current data suggest that fewer than half of patients with DCIS eventually progress to the development of invasive ductal carcinoma (IDC), and that the molecular mechanisms behind progression are complex.1,2,3 Given both the risk of upgrade to IDC at the time of excision and the potential disease progression to IDC over time, the National Comprehensive Cancer Network guidelines currently recommend excision of DCIS to negative margins with either mastectomy or breast-conserving therapy.4
Currently, DCIS accounts for approximately 20% of breast cancer diagnoses, and its incidence has been increasing since the initiation of screening mammography.5, 6 Because no parallel decrease in the incidence of advanced cancers has occurred, many have questioned whether this surplus in DCIS cases represents a subset of patients who would not have progressed to IDC and are therefore being overtreated.7
Many controversies still exist around how to treat DCIS,8 and there is interest in identifying patients who may not benefit from surgical excision, as evidenced by ongoing trials evaluating active surveillance for patients with DCIS.9, 12
Several trials of active surveillance include the use of endocrine therapy, which is commonly used in the adjuvant setting given that approximately 75% of DCIS is hormone receptor-positive (HR+).13 However, non-operative management strategies for DCIS, which represent an “infinite delay” in surgical treatment, may be of concern because preoperative delays in DCIS are associated with an increased incidence of IDC at the time of ultimate excision.14
In early 2020, the Severe Acute Respiratory Syndrome-Coronavirus 2 (SARS-CoV-2) pandemic necessitated postponement of elective surgery throughout the United Sates, which included delay of surgery for breast cancer.15 The Society of Surgical Oncology and the COVID-19 Breast Cancer Consortium developed recommendations for the triage of patients during the pandemic.16,17 Specifically, the groups recommended neoadjuvant endocrine therapy (NET) for HR+ DCIS to bridge delays in upfront surgery based on clinical trials showing the efficacy of endocrine therapy against invasive breast cancer in the nonoperative setting and its recurrence benefits for DCIS. Data on outcomes for patients who experienced surgical delay during the pandemic are forthcoming. We designed this study to assess the impact of delay and the use of NET for patients with DCIS by testing the hypothesis that the use of NET decreases the rate of IDC at the time of excision regardless of the length of the preoperative delay.
Methods
Study Design
A retrospective study analyzed women with DCIS using the National Cancer Database (NCDB) from 2006 to 2017. The NCDB is a joint collaboration between the American College of Surgeons and the American Cancer Society in which patient-level data are collected from all cancer patients seen in Commission on Cancer-accredited programs,18 representing approximately 70% of United States cancer cases.19 The NCDB studies were deemed by the Fox Chase Cancer Center IRB to be exempt at the time of submission.
We identified female patients with no previous malignancies, American Joint Committee on Cancer (AJCC) clinical stage 0 breast cancer, and DCIS or invasive ductal carcinoma on final pathology based on International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) Surveillance, Epidemiology, and End Results (SEER) histology codes (Fig. 1, Table S1). We then excluded patients based on multiple tumor and treatment factors, including those who did not undergo surgical resection; those with hormone (estrogen and progesterone) receptor-negative disease, missing stage, or pathologic stage discrepant with histology; and those who underwent neoadjuvant chemotherapy or radiation. The NCDB censors institution type for women younger than 40 years. Our analysis of institution type was therefore limited to women older than 40 years.
We then stratified the cohort based on whether they underwent NET, which we defined as initiation of endocrine therapy at any time before surgery. Patients whose endocrine therapy status was unknown were excluded. The patients were then categorized based on the time from diagnosis to initial surgery into the following groups: 30 days or less, 31–60 days, 61–90 days, 91–120 days, and 121–365 days. Patients whose time to surgery was 0 days or longer than 365 days were excluded from the analysis cohort.
Finally, the patients’ pathologic stage and ICD-O-3 SEER histology codes were used to identify those with invasive cancer at the time of resection. Tumor size reported in the NCDB is the extent of disease measured on final pathologic evaluation and does not permit a more granular quantitative analysis of the in situ or invasive component of disease.
Statistical Analysis
Patient, tumor, and treatment characteristics were compared both between and within NET and time-to-surgery groups using chi-square tests, Student’s t test, and analysis of variance (ANOVA). Binary logistic regression models were used to evaluate the impact of patient, tumor and treatment characteristics on the upgrade to invasive cancer on final pathology. Because the use and duration of NET are covariate, two multivariable models were constructed: a sensitivity model assessing the use of NET and a primary multivariable model assessing the duration of use, with the duration for those who had not received NET defined as 0 days. The rates of upgrade within each time-to-surgery group were compared using chi-square tests, whereas the trends of rate for invasion across time-to-surgery groups for each NET cohort were evaluated using the Cochran-Armitage trend test. The p values were two-sided, and p values lower than 0.05 were considered statistically significant. Analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA).
Results
Of the 109,990 patients included in the analysis, 276 (0.3%) underwent NET (Table 1). The use of NET increased over time, from 0.22% in 2006 to 0.34% in 2017 (p = 0.001), with lowest rate (0.15%) in 2011 and the highest rate (0.38%) in 2016. Compared with patients who did not receive NET, those who underwent NET were more likely to be older (p = 0.007) and white (p=0.048), to have larger (p = 0.001) well-differentiated (p = 0.001) tumors, and to have undergone mastectomy (p = 0.001).
Insurance status differed between the NET groups, with a larger proportion of patients who underwent NET having Medicare (37%) than those who did not undergo NET (29.2%), and with no uninsured patients in the NET group (p = 0.005). Community cancer centers had the lowest proportion of patients who underwent NET (0.13%), although the difference with other institution types was not significant (p = 0.13).
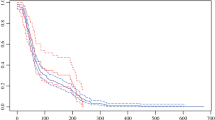
For those who received NET, the mean duration of preoperative therapy was 74.4 days. As expected, the median time to surgery was longer for the NET cohort than for the no-NET cohort (87.5 vs 35 days; p = 0.001). Correspondingly, nearly half (41.8%) of the patients in the no-NET group underwent surgery within 30 days of diagnosis, whereas 33% of the patients who received NET had surgery between 121 and 365 days after diagnosis (Fig. 2).
The duration of NET was directly proportional to the time to surgery. The patients who had surgery within 30 days after diagnosis received NET for a mean of 13 days, whereas the patients who had surgery 121 to 365 days after diagnosis received NET for a mean of 143 days (p < 0.001; Table S2).
Stratification by time-to-surgery group showed differences among patient, tumor, and treatment factors in both the NET and no-NET groups. Interestingly, black patients were more likely to undergo surgery between 121 and 365 days than any racial group in both the NET (51.5%; p = 0.04) and no-NET (4.0%; p < 0.001) groups. Community cancer centers had the highest proportion of patients who underwent surgery within 30 days after diagnosis than any other institution type in both the NET and no-NET groups (both p < 0.001). Similarly, in both the NET and no-NET groups, a higher proportion of patients undergoing lumpectomy had surgery within 30 days, but the difference among the time-to-surgery groups was significant only for the no-NET group (p = 0.09 and 0.001, respectively).
The overall unadjusted rate for invasive cancer was similar between those who did and those who did not receive NET (15.6 vs 12.3%; respectively; p = 0.10; Table 1). Table 2 outlines the results from the uni- and multivariable analyses assessing the patient, tumor, and treatment characteristics associated with finding invasive cancer at the time of excision. The factors associated with invasion in the multivariable analysis were higher income quartile, Medicaid insurance, treatment received at an institution other than a community cancer center, well-differentiated tumors, and treatment with mastectomy rather than lumpectomy.
In the univariate analysis, neither the use of NET nor the duration of NET had a significant association with invasion in the univariate analysis. The use of NET was not significantly associated with invasion in the sensitivity analysis, nor was the duration of NET use associated with invasion in the multivariable model. No significant differences in the cohort of patients experiencing upgrade were observed when the NET and no-NET groups were compared except for a higher proportion of patients with low-grade tumors in the NET group (Table S3).
The unadjusted rate of invasion did not differ between the NET and no-NET cohorts within each time-to-surgery group (Fig. 3). However, the trend in invasion differed significantly between the NET and no-NET cohorts across the time-to-surgery groups, with an increase in the rate of invasion as time to surgery increased for the no-NET group (p < 0.001). The NET group showed no significant trend (p = 0.97). The rate of IDC did increase from the less-than-30-day group (12.9%) through the 61-to-90-day group (21.1%) which was followed by a drop in the 91-to-120-day group (11.9%). The patients in the 91-to-120-day group had a mean NET duration of 57.1 days.
Discussion
This study describes important findings related to the impact of both preoperative delay and NET on the incidence of IDC among patients with HR+ DCIS. We hypothesized that the use of NET would decrease the rate of IDC at the time of excision regardless of preoperative delay, and our analyses demonstrated a difference in the trend for invasion, which suggests a potential protective effect of NET.
The results of this study confirm those of our previous findings in which preoperative delay was associated with an increase in the incidence of IDC among all patients with DCIS.14 In this analysis, we focused on an HR+ subtype of DCIS, and noted that the majority of patients who did not receive NET (>80%) had excision within 60 days after diagnosis. Again, the rate of IDC at excision was positively associated with time to surgery. As expected, the time to surgery was longer for the NET cohort.
The concept that NET may have a protective effect on the development of invasion or progression of invasive tumor growth is founded in several studies evaluating the effects of endocrine therapy on both DCIS and invasive disease. For example, after a median follow-up period of 14.5 years, National Surgical Adjuvant Breast and Bowel Project (NSABP) Trial B-24 established that both tamoxifen and age were among the factors most significant in reducing in-breast tumor recurrence for patients with DCIS who previously underwent breast conservation and radiotherapy.20
Meanwhile, for invasive disease, two nearly identical prospective trials demonstrated that endocrine therapy alone affords benefits similar to those for older women undergoing both surgery and endocrine therapy. Although local events in the nonoperative arm were higher, after a median of 96 months of follow-up evaluation, the Italian GRETA trial found no difference between these approaches in the rates of overall survival from breast cancer.21
A British trial with a similar comparison found no difference in disease-free or overall survival in the first 3 years of trial analysis.22 These data and others provide evidence for the concept that endocrine therapy not only can suppress tumor growth, but also may treat even gross disease in women whose tumors are sensitive to hormonal blockade, and thus should be effective for short-term treatment when excision is not feasible.
The mean duration of NET in this study was 74.4 days, and the duration of NET increased across time-to-surgery groups as expected. Currently no consensus exists on the ideal duration of NET for either DCIS or IDC. One study evaluating the impacts of NET on the rate of invasion and outcomes for patients with DCIS used a standard duration of 3 months,23 and multiple studies have examined the use of NET in IDC, demonstrating a pathologic response with NET duration as short as 8 weeks and response leveling at 12 months.24,25,26
For the NET cohort in this study, the rates of invasion decreased among the patients who had surgery more than 90 days after diagnosis compared with those who had surgery sooner. This may support a 3-month duration of endocrine therapy in the neoadjuvant setting because this observation may reflect a time-to-effect phenomenon in which the protective effect of NET is not realized until after a threshold of exposure is met.
As elective surgeries resumed after the first wave of the SARS-CoV2 pandemic, consortium recommendations permitted those receiving bridging NET to proceed with excision as soon as they were able to be scheduled for surgery regardless of NET duration.27 Therefore, we included all patients who underwent NET up to a preoperative delay of 365 days in the study to reflect the variation among treatment durations during the pandemic. The rate of IDC across time-to-surgery groups showed no linear trend in the NET cohort, likely reflecting confounders that we still cannot identify to inform us which DCIS lesions are likely to develop an invasive component and which will remain in situ. However, there may be a NET treatment effect
When assessing whether the use of NET has an impact on the rate of IDC, our analysis had seemingly conflicting results. First, the trend across time-to-surgery groups demonstrated an increased rate of upgrade to invasive cancer in the no-NET group, but not in the NET group, supporting the concept that NET is protective. In contrast, neither the uni- nor multivariable analysis was able to demonstrate a significant association between the probability of invasion and either the use or duration of NET, and the unadjusted rate of invasion did not differ between the NET cohorts for any of the time-to-surgery groups.
The difference in these analyses may have stemmed from the relatively small number of patients undergoing NET, variability in the amounts of time NET was received, variations in compliance with NET, time to the initiation of NET, or other confounders. However, taken together, the confounders exhibit some evidence to support a protective effect of NET on invasion as preoperative delay increased that is consistent with the level 1 data on endocrine therapy in the adjuvant setting. During the post-pandemic era, in which neoadjuvant endocrine therapy has become more frequent, these findings should be confirmed.
The analysis and conclusions of this study are supported by strengths inherent to using a large national database, but may have been influenced by its limitations. The NCDB is sufficiently large that we could compile an analysis cohort for NET in DCIS, which is a treatment method that until the SARS-CoV2 pandemic had not seen widespread use outside clinical trials. Our NET cohort was small relative to the non-NET group given its rare use over the time of investigation, and this may have limited the power of our study to detect a difference between the groups in our analyses. Given that NET is not a standard treatment regimen for DCIS, our analysis also may have been influenced by selection bias because in this pre-pandemic cohort, non-random factors may have led patients and physicians to choose NET, leading to potential confounding variables that could have masked differences between the groups. Additional analyses of larger datasets that further stratify patients into groups based on low-risk features, including those under active surveillance for DCIS, may reveal additional insights into the impact of NET on invasion. Ultimately, however, to avoid confounding, a prospective trial would likely be required to achieve the power and long-term follow-up evaluation needed for a definitive proof of a protective effect by NET when preoperative delays are unavoidable. Whether such a trial can be performed also may be influenced by results from three ongoing nonoperative DCIS trials9,28,29 evaluating whether nonoperative DCIS management provides outcomes similar to those of strategies that use excision.
Conclusions
In summary, for women with HR+ DCIS, NET may have a protective effect of NET against the development of invasive cancer as preoperative delay increases. As outcomes data from greater numbers of patients treated with NET during the SARS-CoV2 pandemic and the trials of active surveillance in DCIS become available, the impact and optimal duration of NET may become clearer.
References
Collins LC, Tamimi RM, Baer HJ, Connolly JL, Colditz GA, Schnitt SJ. Outcome of patients with ductal carcinoma in situ untreated after diagnostic biopsy. Cancer. 2005;103:1778–84. https://doi.org/10.1002/cncr.20979.
Erbas B, Provenzano E, Armes J, Gertig D. The natural history of ductal carcinoma in situ of the breast: a review. Breast Cancer Res Treat. 2006;97:135–44. https://doi.org/10.1007/s10549-005-9101-z.
Cowell CF, Weigelt B, Sakr RA, et al. Progression from ductal carcinoma in situ to invasive breast cancer: revisited. Mol Oncol. 2013;7:859–69. https://doi.org/10.1016/j.molonc.2013.07.005.
Abraham J, Aft R, Agnese D, et al. NCCN Guidelines Version 3.2021 Breast Cancer. 2021. https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 8 Oct 2021.
Gorringe KL, Fox SB. Ductal carcinoma in situ biology, biomarkers, and diagnosis. Front Oncol. 2017;7:248. https://doi.org/10.3389/fonc.2017.00248.
Kerlikowske K. Epidemiology of ductal carcinoma in situ. J Natl Cancer Inst Monogr. 2010;2010:139–41. https://doi.org/10.1093/jncimonographs/lgq027.
Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367:1998–2005. https://doi.org/10.1056/NEJMoa1206809.
Barrio AV, Van Zee KJ. Controversies in the treatment of ductal carcinoma in situ. Annu Rev Med. 2017;68:197–211. https://doi.org/10.1146/annurev-med-050715-104920.
LORIS–University of Birmingham. Retrieved 17 April 2021 at https://www.birmingham.ac.uk/research/crctu/trials/loris/index.aspx.
Management of Low-risk (Grade I and II) DCIS - Full Text View - ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02492607. Accessed April 17, 2021.
Comparing an Operation to Monitoring, With or Without Endocrine Therapy (COMET) Trial for Low-Risk DCIS: Full Text View–ClinicalTrials.gov. Retrieved 17 April 2021 at https://clinicaltrials.gov/ct2/show/NCT02926911.
Kanbayashi C, Thompson AM, Hwang E-SS, et al. The international collaboration of active surveillance trials for low-risk DCIS LORIS, LORD, COMET, LORETTA. J Clin Oncol. 2019;37(15 suppl):TPS603–4. https://doi.org/10.1200/jco.2019.37.15_suppl.tps603.
Lari SA, Kuerer HM. Biological markers in DCIS and risk of breast recurrence: a systematic review. J Cancer. 2011;2:232–61. https://doi.org/10.7150/jca.2.232.
Ward WH, DeMora L, Handorf E, et al. Preoperative delays in the treatment of DCIS and the associated incidence of invasive breast cancer. Ann Surg Oncol. 2020;27:386–96. https://doi.org/10.1245/s10434-019-07844-4.
CMS Releases Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures During COVID-19 Response/CMS. Retrieved 17 April 2021 at https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental.
Bartlett DL, Howe JR, Chang G, et al. Management of cancer surgery cases during the COVID-19 pandemic: considerations. Ann Surg Oncol. 2020;27:1717–20. https://doi.org/10.1245/s10434-020-08461-2.
Dietz JR, Moran MS, Isakoff SJ, et al. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic the COVID-19 pandemic breast cancer consortium. Breast Cancer Res Treat. 2020;181:487–97. https://doi.org/10.1007/s10549-020-05644-z.
Boffa DJ, Rosen JE, Mallin K, et al. Using the National Cancer Database for outcomes research: a review. JAMA Oncol. 2017;3:1722–8. https://doi.org/10.1001/jamaoncol.2016.6905.
Mallin K, Browner A, Palis B, et al. Incident cases captured in the National Cancer Database compared with those in US population-based central cancer registries in 2012–2014. Ann Surg Oncol. 2019;26:1604–12. https://doi.org/10.1245/s10434-019-07213-1.
Allred DC, Anderson SJ, Paik S, et al. Adjuvant tamoxifen reduces subsequent breast cancer in women with estrogen receptor-positive ductal carcinoma in situ: a study based on NSABP protocol B-24. J Clin Oncol. 2012;30:1268–73. https://doi.org/10.1200/JCO.2010.34.0141.
Mustacchi G, Scanni A, Capasso I, Farris A, Pluchinotta A, Isola G. Update of the phase III trial “GRETA” of surgery and tamoxifen versus tamoxifen alone for early breast cancer in elderly women. Future Oncol. 2015;11:933–41. https://doi.org/10.2217/fon.14.266.
Fennessy M, Bates T, MacRae K, Riley D, Houghton J, Baum M. Late follow-up of a randomized trial of surgery plus tamoxifen versus tamoxifen alone in women aged over 70 years with operable breast cancer. Br J Surg. 2004;91:699–704. https://doi.org/10.1002/bjs.4603.
Chen YY, DeVries S, Anderson J, et al. Pathologic and biologic response to preoperative endocrine therapy in patients with ER-positive ductal carcinoma in situ. BMC Cancer. 2009;9:285. https://doi.org/10.1186/1471-2407-9-285.
Allevi G, Strina C, Andreis D, et al. Increased pathological complete response rate after a long-term neoadjuvant letrozole treatment in postmenopausal oestrogen and/or progesterone receptor-positive breast cancer. Br J Cancer. 2013;108:1587–92. https://doi.org/10.1038/bjc.2013.151.
Carpenter R, Doughty JC, Cordiner C, et al. Optimum duration of neoadjuvant letrozole to permit breast-conserving surgery. Breast Cancer Res Treat. 2014;144:569–76. https://doi.org/10.1007/s10549-014-2835-8.
Spring LM, Gupta A, Reynolds KL, et al. Neoadjuvant endocrine therapy for estrogen receptor-positive breast cancer: a systematic review and meta-analysis. JAMA Oncol. 2016;2:1477–86. https://doi.org/10.1001/jamaoncol.2016.1897.
COVID-19 Pandemic Breast Cancer Consortium Develops Considerations for Re-entry. Retrieved 17 April 2021 at https://www.facs.org/quality-programs/cancer/news/considerations-for-reentry-051520.
Hwang ES, Hyslop T, Lynch T, et al. The COMET (Comparison of Operative versus Monitoring and Endocrine Therapy) trial: a phase III randomised controlled clinical trial for low-risk ductal carcinoma in situ (DCIS). BMJ Open. 2019;9:e026797. https://doi.org/10.1136/bmjopen-2018-026797.
Elshof LE, Tryfonidis K, Slaets L, et al. Feasibility of a prospective, randomised, open-label, international multicentre, phase III, non-inferiority trial to assess the safety of active surveillance for low-risk ductal carcinoma in situ: the LORD study. Eur J Cancer. 2015;51:1497–510. https://doi.org/10.1016/j.ejca.2015.05.008.
Acknowledgment
This study was supported by United States Public Health Services Grant P30CA006927 and by private funding from the Marlyn Fein chapter of the Fox Chase Cancer Center Board of Associates for statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Williams, A.D., Chang, C., Sigurdson, E.R. et al. Neoadjuvant Endocrine Therapy and Delays in Surgery for Ductal Carcinoma in Situ: Implications for the Coronavirus Pandemic. Ann Surg Oncol 29, 1683–1691 (2022). https://doi.org/10.1245/s10434-021-10883-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10883-5