Abstract
Objective
This study aimed to construct a nomogram to quantitatively predict pneumonectomy complication risks for non-small cell lung cancer (NSCLC) patients.
Methods
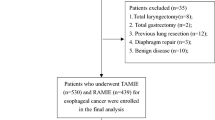
Data from 1052 NSCLC patients who underwent pneumonectomy were retrospectively retrieved from the databases of three thoracic centers. Multivariable logistic regression was used to investigate postoperative morbidity predictors. Clinical parameters and operative features were analyzed using univariable and multivariable logistic regression analyses, and a nomogram to predict the risk of postoperative complications was constructed using bootstrap resampling. A receiver operating characteristic (ROC) curve was used to estimate the discrimination power for the nomogram.
Results
A total of 212 patients (20.2%) had major complications. After regression analysis, forced expiratory volume in 1 s, Charlson Comorbidity Index score, male sex, and right-sided pneumonectomy were identified and entered into the nomogram. The nomogram showed a robust discrimination, with an area under the ROC curve of 0.753 (95% confidence interval 0.604–0.818). The calibration curves for the probability of postoperative complications showed optimal agreement between the nomogram and the actual probability.
Conclusions
Based on preoperative data, we developed a nomogram for predicting complication risks after pneumonectomy. This model may be helpful for thoracic surgeons in selecting appropriate patients for adopting prophylactic measures after surgery.





Similar content being viewed by others
REFERENCES
Pei G, Zhou S, Han Y, Liu Z, Xu S. Risk factors for postoperative complications after lung resection for non-small cell lung cancer in elderly patients at a single institution in China. J Thorac Dis. 2014;6(9):1230–8. https://doi.org/10.3978/j.issn.2072-1439.2014.07.23.
Handy JR Jr, Denniston K, Grunkemeier GL, Wu YX. What is the inpatient cost of hospital complications or death after lobectomy or pneumonectomy? Ann Thorac Surg. 2011;91(1):234–8. https://doi.org/10.1016/j.athoracsur.2010.08.043.
Wang G, Liu L, Zhang J, Li S. The analysis of prognosis factor in patients with non-small cell lung cancer receiving pneumonectomy. J Thorac Dis. 2020;12(4):1366–73. https://doi.org/10.21037/jtd.2020.02.33.
Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26(8):1364–70. https://doi.org/10.1200/JCO.2007.12.9791.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Jin C, Cao J, Cai Y, et al. A nomogram for predicting the risk of invasive pulmonary adenocarcinoma for patients with solitary peripheral subsolid nodules. J Thorac Cardiovasc Surg. 2017;153(2):462-469 e1. https://doi.org/10.1016/j.jtcvs.2016.10.019.
Wang S, Yang L, Ci B, et al. Development and validation of a nomogram prognostic model for SCLC patients. J Thorac Oncol. 2018;13(9):1338–48. https://doi.org/10.1016/j.jtho.2018.05.037.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
Birim O, Maat AP, Kappetein AP, van Meerbeeck JP, Damhuis RA, Bogers AJ. Validation of the Charlson comorbidity index in patients with operated primary non-small cell lung cancer. Eur J Cardiothorac Surg. 2003;23(1):30–4. https://doi.org/10.1016/s1010-7940(02)00721-2.
Thomas PA, Berbis J, Baste JM, et al. Pneumonectomy for lung cancer: contemporary national early morbidity and mortality outcomes. J Thorac Cardiovasc Surg. 2015;149(1):73–82. https://doi.org/10.1016/j.jtcvs.2014.09.063.
Pforr A, Pages PB, Baste JM, et al. A Predictive Score for Bronchopleural Fistula Established Using the French Database Epithor. Ann Thorac Surg. 2016;101(1):287–93. https://doi.org/10.1016/j.athoracsur.2015.06.026.
Dong J, Mao Y, Li J, He J. Stair-Climbing Test Predicts Postoperative Cardiopulmonary Complications and Hospital Stay in Patients with Non-Small Cell Lung Cancer. Med Sci Monit. 2017;23:1436–41. https://doi.org/10.12659/msm.900631.
Mazzella A, Pardolesi A, Maisonneuve P, et al. Bronchopleural fistula after pneumonectomy: risk factors and management, focusing on open-window Thoracostomy. Semin Thorac Cardiovasc Surg Spring. 2018;30(1):104–13. https://doi.org/10.1053/j.semtcvs.2017.10.003.
Blanc K, Dechartres A, Zaimi R, et al. Patients experiencing early acute respiratory failure have high postoperative mortality after pneumonectomy. J Thorac Cardiovasc Surg. Dec 2018;156(6):2368–76. https://doi.org/10.1016/j.jtcvs.2018.08.113.
Soll C, Hahnloser D, Frauenfelder T, Russi EW, Weder W, Kestenholz PB. The postpneumonectomy syndrome: clinical presentation and treatment. Eur J Cardiothorac Surg. 2009;35(2):319–24. https://doi.org/10.1016/j.ejcts.2008.07.070.
da Silva PS, de Oliveira R, Tamura N, Neto HM. Right pneumonectomy syndrome: a late life-threatening complication of pneumonectomy. Pediatr Emerg Care. 2010;26(7):499–502. https://doi.org/10.1097/PEC.0b013e3181e5bfb3.
Daffre E, Prieto M, Huang H, et al. Normalized pulmonary artery diameter predicts occurrence of postpneumonectomy respiratory failure, ARDS, and mortality. Cancers (Basel). 2020;12(6):1515. https://doi.org/10.3390/cancers12061515.
Birim O, Kappetein AP, Bogers AJ. Charlson comorbidity index as a predictor of long-term outcome after surgery for nonsmall cell lung cancer. Eur J Cardiothorac Surg. 2005;28(5):759–62. https://doi.org/10.1016/j.ejcts.2005.06.046.
Otake S, Ohtsuka T, Asakura K, Kamiyama I, Kohno M. Impact of comorbidity index on morbidity and survival in non-small cell lung cancer. Asian Cardiovasc Thorac Ann. 2016;24(1):30–3. https://doi.org/10.1177/0218492315617834.
Yang CC, Fong Y, Lin LC, et al. The age-adjusted Charlson comorbidity index is a better predictor of survival in operated lung cancer patients than the Charlson and Elixhauser comorbidity indices. Eur J Cardiothorac Surg. 2018;53(1):235–40. https://doi.org/10.1093/ejcts/ezx215.
Mitsudomi T, Mizoue T, Yoshimatsu T, et al. Postoperative complications after pneumonectomy for treatment of lung cancer: multivariate analysis. J Surg Oncol. 1996;61(3):218–22. https://doi.org/10.1002/(SICI)1096-9098(199603)61:3%3c218::AID-JSO11%3e3.0.CO;2-3.
Rodriguez M, Gomez Hernandez MT, Novoa NM, Aranda JL, Jimenez MF, Varela G. Morbidity and mortality in octogenarians with lung cancer undergoing pneumonectomy. Arch Bronconeumol. 2015;51(5):219–22. https://doi.org/10.1016/j.arbres.2014.07.008.
Leo F, Scanagatta P, Baglio P, et al. The risk of pneumonectomy over the age of 70 A case-control study. Eur J Cardiothorac Surg. 2007;31(5):780–2. https://doi.org/10.1016/j.ejcts.2007.01.036.
Parquin F, Marchal M, Mehiri S, Herve P, Lescot B. Post-pneumonectomy pulmonary edema: analysis and risk factors. Eur J Cardiothorac Surg. 1996;10(11):929–32. https://doi.org/10.1016/s1010-7940(96)80392-7 (discussion 933).
Cao C, Louie BE, Melfi F, et al. Outcomes of major complications after robotic anatomic pulmonary resection. J Thorac Cardiovasc Surg. 2020;159(2):681–6. https://doi.org/10.1016/j.jtcvs.2019.08.057.
Acknowledgments
This study was supported by the Beijing Municipal Administration of Hospitals Incubating Program (Code: PX2021060) and the National Nature Science Foundation of China (No. 81670089). The authors thank LetPub (www.letpub.com) for their linguistic assistance during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure
Wang Chong, Wang Shaodong, He Wenxin, and Li Zhixin declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1
Rights and permissions
About this article
Cite this article
Wang, C., Wang, S., Li, Z. et al. A Multiple-Center Nomogram to Predict Pneumonectomy Complication Risk for Non-Small Cell Lung Cancer Patients. Ann Surg Oncol 29, 561–569 (2022). https://doi.org/10.1245/s10434-021-10504-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10504-1