Abstract
Background
The oncologic advantage of anatomic resection (AR) for primary hepatocellular carcinoma (HCC) remains controversial. This study aimed to evaluate the clinical advantages of AR for primary HCC by using propensity score-matching and by assessing treatment strategies for recurrence after surgery.
Methods
The study reviewed data of patients who underwent AR or non-anatomic resection (NAR) for solitary HCC (≤ 5 cm) in two institutions between 2004 and 2017. Surgical outcomes were compared between the two groups in a propensity score-adjusted cohort. The time-to-interventional failure (TIF), defined as the elapsed time from resection to unresectable/unablatable recurrence, also was evaluated.
Results
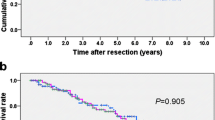
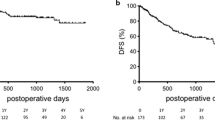
The inclusion criteria were met by 250 patients: 77 patients (31%) with AR and 173 patients (69%) with NAR. In the propensity score-matched populations (AR, 67; NAR, 67), the 5-year recurrence-free survival (RFS) for AR was better than for NAR (62% vs 35%; P = 0.005). No differences, however, were found in the 5-year overall survival between the two groups (72% vs 78%; P = 0.666). The 5-year TIF rates for the NAR group (60%) also were similar to those for the AR group (66%) (P = 0.413). In the cohort of 67 patients, curative repeat resection or ablation therapy was performed more frequently for the NAR patients (42%) than for the AR patients (10%) (P < 0.001).
Conclusion
For solitary HCC, AR decreases recurrence after the initial hepatectomy. However, aggressive curative-intent interventions for recurrence compensate for the impaired RFS, even for patients undergoing NAR.



Similar content being viewed by others
References
Fitzmaurice C, Allen C, Barber RM, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol. 2017;3:524–48.
Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatol Baltimore. 2011;53:1020–2.
Makuuchi M, Kokudo N, Arii S, et al. Development of evidence-based clinical guidelines for the diagnosis and treatment of hepatocellular carcinoma in Japan. Hepatol Res. 2008;38:37–51.
Fan ST, Lo CM, Liu CL, et al. Hepatectomy for hepatocellular carcinoma: toward zero hospital deaths. Ann Surg. 1999;229:322–30.
Nakashima T, Kojiro M. Pathologic characteristics of hepatocellular carcinoma. Semin Liver Dis. 1986;6:259–66.
Makuuchi M, Hasegawa H, Yamazaki S. Ultrasonically guided subsegmentectomy. Surg Gynecol Obstet. 1985;161:346–50.
Ishii M, Mizuguchi T, Kawamoto M, et al. Propensity score analysis demonstrated the prognostic advantage of anatomical liver resection in hepatocellular carcinoma. World J Gastroenterol. 2014;20:3335–42.
Cucchetti A, Qiao GL, Cescon M, et al. Anatomic versus nonanatomic resection in cirrhotic patients with early hepatocellular carcinoma. Surgery. 2014;155:512–21.
Kaibori M, Kon M, Kitawaki T, et al. Comparison of anatomic and non-anatomic hepatic resection for hepatocellular carcinoma. J Hepato-Biliary-Pancreatic Sci. 2017;24:616–26.
Shindoh J, Makuuchi M, Matsuyama Y, et al. Complete removal of the tumor-bearing portal territory decreases local tumor recurrence and improves disease-specific survival of patients with hepatocellular carcinoma. J Hepatol. 2016;64:594–600.
Kaibori M, Yoshii K, Hasegawa K, et al. Impact of systematic segmentectomy for small hepatocellular carcinoma. J Hepato-Biliary-Pancreatic Sci. 2020;27:331–41.
Okamura Y, Ito T, Sugiura T, Mori K, Uesaka K. Anatomic versus nonanatomic hepatectomy for a solitary hepatocellular carcinoma: a case-controlled study with propensity score matching. J Gastrointest Surg. 2014;18:1994–2002.
Marubashi S, Gotoh K, Akita H, et al. Anatomical versus non-anatomical resection for hepatocellular carcinoma. Br J Surg. 2015;102:776–84.
Shindoh J, Kawamura Y, Kobayashi Y, et al. Time-to-interventional failure as a new surrogate measure for survival outcomes after resection of hepatocellular carcinoma. J Gastrointest Surg. 2020;24(1):50–7.
Oguro S, Yoshimoto J, Imamura H, Ishizaki Y, Kawasaki S. Clinical significance of macroscopic no-margin hepatectomy for hepatocellular carcinoma. HPB. 2018;20:872–80.
Kishi Y, Saiura A, Yamamoto J, et al. Significance of anatomic resection for early and advanced hepatocellular carcinoma. Langenbeck’s Arch Surg. 2012;397:85–92.
Makuuchi M, Kosuge T, Takayama T, et al. Surgery for small liver cancers. Semin Surg Oncol. 1993;9:298–304.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Mise Y, Vauthey JN, Zimmitti G, et al. Ninety-day postoperative mortality is a legitimate measure of hepatopancreatobiliary surgical quality. Ann Surg. 2015;262:1071–8.
Xing H, Sun LY, Yan WT, et al. Repeat hepatectomy for patients with early and late recurrence of hepatocellular carcinoma: a multicenter propensity score-matching analysis. Surgery. 2021;169(4):911–20.
Erridge S, Pucher PH, Markar SR, et al. Meta-analysis of determinants of survival following treatment of recurrent hepatocellular carcinoma. Br J Surg. 2017;104:1433–42.
Zhou Y, Sui C, Li B, et al. Repeat hepatectomy for recurrent hepatocellular carcinoma: a local experience and a systematic review. World J Surg Oncol. 2010;8:55.
Chan DL, Morris DL, Chua TC. Clinical efficacy and predictors of outcomes of repeat hepatectomy for recurrent hepatocellular carcinoma - a systematic review. Surg Oncol. 2013;22:e23-30.
Feng Y, Wu H, Huang DQ, et al. Radiofrequency ablation versus repeat resection for recurrent hepatocellular carcinoma (≤5 cm) after initial curative resection. Eur Radiol. 2020;30:6357–68.
Mise Y, Aloia TA, Brudvik KW, Schwarz L, Vauthey JN, Conrad C. Parenchymal-sparing hepatectomy in colorectal liver metastasis improves salvageability and survival. Ann Surg. 2016;263:146–52.
Mise Y, Hasegawa K, Shindoh J, et al. The feasibility of third or more repeat hepatectomy for recurrent hepatocellular carcinoma. Ann Surg. 2015;262:347–57.
Toro A, Pulvirenti E, Palermo F, Di Carlo I. Health-related quality of life in patients with hepatocellular carcinoma after hepatic resection, transcatheter arterial chemoembolization, radiofrequency ablation or no treatment. Surg Oncol. 2012;21:e23-30.
Huang G, Chen X, Lau WY, et al. Quality of life after surgical resection compared with radiofrequency ablation for small hepatocellular carcinomas. Br J Surg. 2014;101:1006–15.
Chie WC, Yu F, Li M, et al. Quality of life changes in patients undergoing treatment for hepatocellular carcinoma. Qual Life Res. 2015;24:2499–506.
Mise Y, Satou S, Ishizawa T, et al. Impact of surgery on quality of life in patients with hepatocellular carcinoma. World J Surg. 2014;38:958–67.
Yamashita Y, Hamatsu T, Rikimaru T, et al. Bile leakage after hepatic resection. Ann Surg. 2001;233:45–50.
Nagano Y, Togo S, Tanaka K, et al. Risk factors and management of bile leakage after hepatic resection. World J Surg. 2003;27:695–8.
Capussotti L, Ferrero A, Viganò L, Sgotto E, Muratore A, Polastri R (2006) Bile leakage and liver resection: where is the risk? Arch Surg. 141:690–4 (discussion 695).
Morimura R, Saiura A, Koga R, et al. Impact of previous hepatectomy on short-term outcomes of repeat hepatectomy for liver tumors with a special concern of operative time. Hepatogastroenterology. 2012;59:809–13.
Sadamori H, Yagi T, Matsuda H, Shinoura S, Umeda Y, Fujiwara T. Intractable bile leakage after hepatectomy for hepatocellular carcinoma in 359 recent cases. Dig Surg. 2012;29:149–56.
Sadamori H, Yagi T, Shinoura S, et al. Risk factors for major morbidity after liver resection for hepatocellular carcinoma. Br J Surg. 2013;100:122–9.
Livraghi T, Solbiati L, Meloni MF, Gazelle GS, Halpern EF, Goldberg SN. Treatment of focal liver tumors with percutaneous radiofrequency ablation: complications encountered in a multicenter study. Radiology. 2003;226:441–51.
Choi D, Lim HK, Rhim H, et al. Percutaneous radiofrequency ablation for recurrent hepatocellular carcinoma after hepatectomy: long-term results and prognostic factors. Ann Surg Oncol. 2007;14:2319–29.
Choi D, Lim HK, Kim MJ, et al. Liver abscess after percutaneous radiofrequency ablation for hepatocellular carcinomas: frequency and risk factors. AJR Am J Roentgenol. 2005;184:1860–7.
Imamura H, Matsuyama Y, Tanaka E, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003;38:200–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Minagawa, M., Mise, Y., Omichi, K. et al. Anatomic Resection for Hepatocellular Carcinoma: Prognostic Impact Assessed from Recurrence Treatment. Ann Surg Oncol 29, 913–921 (2022). https://doi.org/10.1245/s10434-021-10380-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10380-9