Abstract
Background
Studies have shown intra-arterial therapies to be effective in controlling neuroendocrine liver metastases (NELMs), but the evidence supporting the selection of specific methods is limited. This meta-analysis is the first to compare survival outcomes between transarterial chemoembolization (TACE) and transarterial radioembolization (TARE) in the treatment of NELM.
Methods
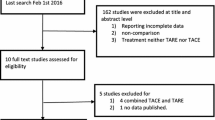
A systematic search according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines in PubMed and Embase databases was conducted in February 2020 for published studies comparing survival outcomes between TACE and TARE in the treatment of NELM.
Results
Six eligible cohort studies with a total of 643 patients were identified. The TACE and TARE groups were similar in terms of age, sex, hepatic tumor burden, tumor grade, and Eastern Cooperative Oncology Group (ECOG) score. The patients treated with TACE had significantly better overall survival (odds ratio [OR], 1.92; 95% confidence interval [CI] 1.14–3.22, p = 0.014) than those treated with TARE. Overall survival ranged from 16.8 to 81.9 months with TACE and from 14.5 to 66.8 months with TARE. No significant differences in hepatic progression-free survival (OR, 1.01; 95% CI 0.75–1.35; p = 0.96) or tumor response were observed within the first 3 months (OR, 2.87; 95% CI 0.81–10.21; p = 0.10) or thereafter (OR, 0.98; 95% CI 0.12–7.86; p = 0.99). The complication rates were similar between the two groups, with 6.9% of the TACE patients versus 8.5% of TARE patients reporting major complications (OR, 1.16; 95% CI 0.54–2.48; p = 0.71) and respectively 44.6% and 58.8% of the TACE and TARE patients reporting minor adverse events (OR, 1.08; 95% CI 0.39–2.99; p = 0.88).
Conclusions
Despite similar tumor responses, an overall survival benefit was associated with TACE treatment of NELM compared with TARE treatment. Randomized controlled trials are warranted to confirm this finding and clarify whether certain subpopulations benefit from different transarterial methods.





Similar content being viewed by others
References
Cives M, Strosberg JR. Gastroenteropancreatic neuroendocrine tumors. CA Cancer J Clin. 2018;68:471–87.
Dogeas E, Chong CCN, Weiss MJ, et al. Can echogenic appearance of neuroendocrine liver metastases on intraoperative ultrasonography predict tumor biology and prognosis? HPB Oxford. 2018;20:237–43.
Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26:3063–72.
Jia Z, Wang W. Yttrium-90 radioembolization for unresectable metastatic neuroendocrine liver tumor: a systematic review. Eur J Radiol. 2018;100:23–9.
Zeitels J, Naunheim K, Kaplan EL, Straus F. Carcinoid tumors: a 37-year experience. Arch Surg. 1982;117:732–7.
Bagante F, Spolverato G, Merath K, et al. Neuroendocrine liver metastasis: the chance to be cured after liver surgery. J Surg Oncol. 2017;115:687–95.https://doi.org/10.1002/jso.24563.
Bloomston M, Al-Saif O, Klemanski D, et al. Hepatic artery chemoembolization in 122 patients with metastatic carcinoid tumor: lessons learned. J Gastrointest Surg. 2007;11:264–71.
Dermine S, Palmieri L-J, Lavole J, et al. Nonpharmacological therapeutic options for liver metastases in advanced neuroendocrine tumors. J Clin Med. 2019;8:1907.
Pavel M, Costa F, Capdevila J, et al. ENETS consensus guidelines update for the management of distant metastatic disease of intestinal, pancreatic, bronchial neuroendocrine neoplasms (NEN) and NEN of unknown primary site. Neuroendocrinology. 2016;103:172–85.
Kulke MH, Anthony LB, Bushnell DL, et al. NANETS treatment guidelines: well-differentiated neuroendocrine tumors of the stomach and pancreas. Pancreas. 2010;39:735.
Boudreaux JP, Klimstra DS, Hassan MM, et al. The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: well-differentiated neuroendocrine tumors of the jejunum, ileum, appendix, and cecum. Pancreas. 2010;39:753–66.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: neuroendocrine and adrenal tumors. 2019.
Minh DD, Chapiro J, Gorodetski B, et al. Intra-arterial therapy of neuroendocrine tumour liver metastases: comparing conventional TACE, drug-eluting beads TACE and yttrium-90 radioembolisation as treatment options using a propensity score analysis model. Eur Radiol. 2017;27:4995–5005.
Egger ME, Armstrong E, Martin II RCG, et al. Transarterial chemoembolization vs radioembolization for neuroendocrine liver metastases: a multi-institutional analysis. J Am Coll Surg. 2020;230:363–70. https://doi.org/10.1016/j.jamcollsurg.2019.12.026.
Ozkan F, Peynircioglu B, Cil BE, et al. Transarterial chemo and radioembolization (yttrium90) of hepatic metastasis of neuroendocrine tumors: single-center experience. UHOD Uluslararasi Hematoloji-Onkoloji Dergisi. 2013;23:20–7.
Engelman ES, Leon-Ferre R, Naraev BG, et al. Comparison of transarterial liver-directed therapies for low-grade metastatic neuroendocrine tumors in a single institution. Pancreas. 2014;43:219–25. https://doi.org/10.1097/mpa.0000000000000030.
Chen JX, Rose S, White SB, et al. Embolotherapy for neuroendocrine tumor liver metastases: prognostic factors for hepatic progression-free survival and overall survival. Cardiovasc Intervent Radiol. 2017;40:69–80.
Singla S, LeVea CM, Pokuri VK, et al. Ki67 score as a potential predictor in the selection of liver-directed therapies for metastatic neuroendocrine tumors: a single institutional experience. J Gastrointest Oncol. 2016;7:441–8.
Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3:1335–42.
Nazario J, Gupta S. Transarterial liver-directed therapies of neuroendocrine hepatic metastases. Semin Oncol. 2010;37:118–26.
Peynircioǧlu B, Çil B, Bozkurt F, et al. Radioembolization for the treatment of unresectable liver cancer: initial experience at a single center. Diagnostic Interv Radiol. 2010;16:70–8. https://doi.org/10.4261/1305-3825.DIR.2693-09.1
Strosberg JR, Cheema A, Kvols LK. A review of systemic and liver-directed therapies for metastatic neuroendocrine tumors of the gastroenteropancreatic tract. Cancer Control. 2011;18:127–37.
Gaur SK, Friese JL, Sadow CA, et al. Hepatic arterial chemoembolization using drug-eluting beads in gastrointestinal neuroendocrine tumor metastatic to the liver. Cardiovasc Intervent Radiol. 2011;34:566–72.
Riaz A, Kulik LM, Mulcahy MF, et al. Yttrium-90 radioembolization in the management of liver malignancies. Semin Oncol. 2010;37:94–101.
Dhir M, Shrestha R, Steel JL, et al. Initial treatment of unresectable neuroendocrine tumor liver metastases with transarterial chemoembolization using streptozotocin: a 20-year experience. Ann Surg Oncol. 2017;24:450–9.
Dong XD, Carr BI. Hepatic artery chemoembolization for the treatment of liver metastases from neuroendocrine tumors: a long-term follow-up in 123 patients. Med Oncol. 2011;28:S286–90.
Kennedy AS, Dezarn WA, McNeillie P, et al. Radioembolization for unresectable neuroendocrine hepatic metastases using resin 90Y-microspheres: early results in 148 patients. Am J Clin Oncol Cancer Clin Trials. 2008;31:271–9.
Memon K, Lewandowski RJ, Mulcahy MF, et al. Radioembolization for neuroendocrine liver metastases: safety, imaging, and long-term outcomes. Int J Radiat Oncol Biol Phys. 2012;83:887–94.
Rhee TK, Lewandowski RJ, Liu DM, et al. 90Y radioembolization for metastatic neuroendocrine liver tumors: preliminary results from a multi-institutional experience. Ann Surg. 2008;247:1029–35.
Varker KA, Martin EW, Klemanski D, et al. Repeat transarterial chemoembolization (TACE) for progressive hepatic carcinoid metastases provides results similar to first TACE. J Gastrointest Surg. 2007;11:1680–5.
Valkema R, Pauwels S, Kvols LK, et al. Survival and response after peptide receptor radionuclide therapy with [90Y-DOTA0, Tyr3]octreotide in patients with advanced gastroenteropancreatic neuroendocrine tumors. Semin Nucl Med. 2006;36:147–56.
Strosberg J, El-Haddad G, Wolin E, et al. Phase 3 trial of 177Lu-Dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376:125–35. https://doi.org/10.1056/NEJMoa1607427.
Disclosure
There are no conflicts of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ngo, L., Elnahla, A., Attia, A.S. et al. Chemoembolization Versus Radioembolization for Neuroendocrine Liver Metastases: A Meta-analysis Comparing Clinical Outcomes. Ann Surg Oncol 28, 1950–1958 (2021). https://doi.org/10.1245/s10434-020-09469-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09469-4