Abstract
Background
Gastrointestinal cancer surgery patients often develop perioperative anemia commonly treated with red blood cell (RBC) transfusions. Given the potential associated risks, evidence published over the past 10 years supports restrictive transfusion practices and blood conservation programs. Whether transfusion practices have changed remains unclear. We describe temporal RBC transfusion trends in a large North American population who underwent gastrointestinal cancer surgery.
Methods
We conducted a population-based retrospective cohort study of patients who underwent gastrointestinal cancer resection between 2007 and 2018 using health administrative datasets. The outcome was RBC transfusion during hospitalization. Temporal transfusion trends were analyzed with Cochran-Armitage tests. Multivariable regression assessed the association between year of diagnosis and likelihood of RBC transfusion while controlling for confounding.
Results
Of 79,764 patients undergoing gastrointestinal cancer resection, the median age was 69 years old (interquartile range (IQR) 60–78 years) and 55.5% were male. The most frequent procedures were colectomy (52.8%) and proctectomy (23.0%). A total of 18,175 patients (23%) received RBC transfusion. The proportion of patients transfused decreased from 26.5% in 2007 to 18.9% in 2018 (p < 0.001). After adjusting for patient, procedure, and hospital factors, the most recent time period (2015–2018) was associated with a reduced likelihood of receiving RBC transfusion [relative risk 0.86 (95% confidence interval: 0.83–0.89)] relative to the intermediate time period (2011–2014).
Conclusion
Over 11 years, we observed decreased RBC transfusion use and reduced likelihood of transfusion in patients undergoing gastrointestinal cancer resection. This information provides a foundation to further examine transfusion appropriateness or explore if additional transfusion minimization in surgical patients can be achieved.



Similar content being viewed by others
References
Lucas DJ, Schexneider KI, Weiss M, et al. Trends and risk factors for transfusion in hepatopancreatobiliary surgery. J Gastrointest Surg. 2014;18:719–28.
Froman JP, Mathiason MA, Kallies KJ, Bottner WA, Shapiro SB. The impact of an integrated transfusion reduction initiative in patients undergoing resection for colorectal cancer. Am J Surg. 2012;204:944–50; discussion 50-1.
Elmi M, Mahar A, Kagedan D, et al. The impact of blood transfusion on perioperative outcomes following gastric cancer resection: an analysis of the American College of Surgeons National Surgical Quality Improvement Program database. Can J Surg. 2016;59:322–9.
Hallet J, Mahar AL, Tsang ME, et al. The impact of peri‐operative blood transfusions on post‐pancreatectomy short‐term outcomes: an analysis from the American College of Surgeons National Surgical Quality Improvement Program. HPB. 2015;17:975–82.
Weber RS, Jabbour N, Martin RC II. Anemia and transfusions in patients undergoing surgery for cancer. AnnSurgOncol. 2008;15:34–45.
Yohanathan L, Coburn NG, McLeod RS, et al. Understanding perioperative transfusion practices in gastrointestinal surgery—a practice survey of general surgeons. J Gastrointest Surg. 2016;20:1106–22.
Ejaz A, Spolverato G, Kim Y, Frank SM, Pawlik TM. Variation in triggers and use of perioperative blood transfusion in major gastrointestinal surgery. Br J Surg. 2014;101:1424–33.
Baron DM, Hochrieser H, Posch M, et al. Preoperative anaemia is associated with poor clinical outcome in non-cardiac surgery patients. Br J Anaesth. 2014;113:416–23.
Beattie WS, Karkouti K, Wijeysundera DN, Tait G. Risk associated with preoperative anemia in noncardiac surgery: a single-center cohort study. Anesthesiology. 2009;110:574–81.
Musallam KM, Tamim HM, Richards T, et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet. 2011;378:1396–407.
Carson JL, Duff A, Poses RM, et al. Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet. 1996;348:1055–60.
Hallet J, Mahar AL, Nathens AB, et al. The impact of perioperative blood transfusions on short-term outcomes following hepatectomy. Hepatobiliary SurgNutr. 2018;7:1-10.
Hill GE, Frawley WH, Griffith KE, Forestner JE, Minei JP. Allogeneic blood transfusion increases the risk of postoperative bacterial infection: a meta-analysis. J Trauma. 2003;54:908–14.
Bernard AC, Davenport DL, Chang PK, Vaughan TB, Zwischenberger JB. Intraoperative transfusion of 1 U to 2 U packed red blood cells is associated with increased 30-day mortality, surgical-site infection, pneumonia, and sepsis in general surgery patients. J Am Coll Surg. 2009;208:931–7, 7.e1-2; discussion 8–9.
Ferraris VA, Davenport DL, Saha SP, Bernard A, Austin PC, Zwischenberger JB. Intraoperative transfusion of small amounts of blood heralds worse postoperative outcome in patients having noncardiac thoracic operations. Ann Thorac Surg. 2011;91:1674–80; discussion 80.
Bennett S, Baker LK, Martel G, et al. The impact of perioperative red blood cell transfusions in patients undergoing liver resection: a systematic review. HPB. 2017;19:321–30.
Amato A, Pescatori M. Perioperative blood transfusions for the recurrence of colorectal cancer. Cochrane Database Syst Rev. 2006:Cd005033.
Squires MH, 3rd, Kooby DA, Poultsides GA, et al. Effect of perioperative transfusion on recurrence and survival after gastric cancer resection: a 7-institution analysis of 765 patients from the US Gastric Cancer Collaborative. J Am Coll Surg. 2015;221:767–77.
Mavros MN, Xu L, Maqsood H, et al. Perioperative blood transfusion and the prognosis of pancreatic cancer surgery: systematic review and meta-analysis. Ann Surg Oncol. 2015;22:4382–91.
Hirai T, Yamashita Y, Mukaida H, Kuwahara M, Inoue H, Toge T. Poor prognosis in esophageal cancer patients with postoperative complications. Surg Today. 1998;28:576–9.
Branagan G, Finnis D, Wessex colorectal cancer audit working G. Prognosis after anastomotic leakage in colorectal surgery. Dis Colon Rectum. 2005;48:1021–6.
Kubota T, Hiki N, Sano T, et al. Prognostic significance of complications after curative surgery for gastric cancer. AnnSurg Oncol. 2014;21:891–8.
Hebert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion requirements in critical care investigators, Canadian critical care trials group. N Engl J Med. 1999;340:409–17.
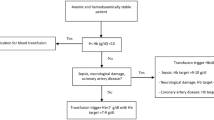
Carson JL, Stanworth SJ, Alexander JH, et al. Clinical trials evaluating red blood cell transfusion thresholds: an updated systematic review and with additional focus on patients with cardiovascular disease. Am Heart J. 2018;200:96–101.
Villanueva C, Colomo A, Bosch A, et al. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368:11–21.
Carson JL, Grossman BJ, Kleinman S, et al. Red blood cell transfusion: a clinical practice guideline from the AABB*. Ann Intern Med. 2012;157:49–58.
Carson JL, Guyatt G, Heddle NM, et al. Clinical practice guidelines from the AABB: red blood cell transfusion thresholds and storage. JAMA. 2016;316:2025–35.
Retter A, Wyncoll D, Pearse R, et al. Guidelines on the management of anaemia and red cell transfusion in adult critically ill patients. Br J Haematol. 2013;160:445–64.
Callum JL, Waters JH, Shaz BH, Sloan SR, Murphy MF. The AABB recommendations for the Choosing Wisely campaign of the American Board of Internal Medicine. Transfusion. 2014;54:2344–52.
Proceedings from the National Summit on Overuse. 2012. Accessed Feb 13, 2020. https://www.jointcommission.org/-/media/deprecated-unorganized/imported-assets/tjc/system-folders/assetmanager/national_summit_overusepdf.pdf?db=web&hash=7629FC4F71411700566C6593FA5A9197.
Kotze A, Harris A, Baker C, et al. British committee for standards in haematology guidelines on the identification and management of pre-operative anaemia. Br J Haematol. 2015;171:322–31.
Qaseem A, Humphrey LL, Fitterman N, Starkey M, Shekelle P. Treatment of anemia in patients with heart disease: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2013;159:770–9.
Spradbrow J, Cohen R, Lin Y, et al. Evaluating appropriate red blood cell transfusions: a quality audit at 10 Ontario hospitals to determine the optimal measure for assessing appropriateness. Transfusion. 2016;56:2466–76.
Hutton B, Fergusson D, Tinmouth A, McIntyre L, Kmetic A, Hébert PC. Transfusion rates vary significantly amongst Canadian medical centres. Can J Anaesth. 2005;52:581–90.
Qiang JK, Thompson T, Callum J, Pinkerton P, Lin Y. Variations in RBC and frozen plasma utilization rates across 62 Ontario community hospitals. Transfusion. 2019;59:545–54.
Ejaz A, Spolverato G, Kim Y, Frank SM, Pawlik TM. Identifying variations in blood use based on hemoglobin transfusion trigger and target among hepatopancreaticobiliary surgeons. J Am Coll of Surg. 2014;219:217–28.
Hallet J, Pronina I, Hanif I, et al. Appropriateness of transfusions for colorectal surgery (ATRACS): a multi-institutional assessment of current red blood cell transfusion practices. Can J Surg. 2014;57:S86–S139.
Ross A, Mohammed S, Vanburen G, et al. An assessment of the necessity of transfusion during pancreatoduodenectomy. Surg. 2013;154:504–11.
Norgaard A, De Lichtenberg TH, Nielsen J, Johansson PI. Monitoring compliance with transfusion guidelines in hospital departments by electronic data capture. Blood Transfus. 2014;12:509–19.
Mueller MM, Van Remoortel H, Meybohm P, et al. Patient blood management: recommendations from the 2018 Frankfurt Consensus Conference. JAMA. 2019;321:983–97.
Lomas J, Anderson GM, Domnick-Pierre K, Vayda E, Enkin MW, Hannah WJ. Do practice guidelines guide practice? The effect of a consensus statement on the practice of physicians. N Engl J Med. 1989;321:1306–11.
Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–65.
LaPar DJ, Crosby IK, Ailawadi G, et al. Blood product conservation is associated with improved outcomes and reduced costs after cardiac surgery. J Thorac Cardiovasc Surg. 2013;145:796–803; discussion-4.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296.
Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12:e1001885.
Government of Canada. Canada Health Act. Government of Canada. Accessed Mar 26, 2020. https://www.canada.ca/en/health-canada/services/health-care-system/canada-health-care-system-medicare/canada-health-act.html.
Robles SC, Marrett LD, Aileen Clarke E, Risch HA. An application of capture-recapture methods to the estimation of completeness of cancer registration. J Clin Epidemiol. 1988;41:495–501.
McLaughlin JR, Kreiger N, Marrett LD, Holowaty EJ. Cancer incidence registration and trends in Ontario. Eur J Cancer Clin Oncol. 1991;27:1520–4.
Juurlink D, Preyra C, Croxford R, et al. Canadian institute for health information discharge abstract database: a validation study. Institute for Clinical Evaluative Sciences, Toronto, Ontario, 2006.
Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T. Identifying individuals with physcian diagnosed COPD in health administrative databases. COPD. 2009;6:388–94.
Austin PC, Daly PA, Tu JV. A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. Am Heart J. 2002;144:290–6.
Hux JE, Ivis F, Flintoft V, Bica A. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care. 2002;25:512–6.
Altoijry A, Al-Omran M, Lindsay TF, Johnston KW, Melo M, Mamdani M. Validity of vascular trauma codes at major trauma centres. Can J Surg. 2013;56:405–8.
DAD Data Elements 2018–2019. Accessed Feb 15, 2020. https://www.cihi.ca/sites/default/files/document/dad-data-elements-2018-en-web.pdf.
Murji A, Lam M, Allen B, et al. Risks of pre-operative anemia in women undergoing elective hysterectomy and myomectomy. Am J Obstet Gynecol. 2019.
Kralj B. Measuring “rurality” for purposes of health-care planning: an empirical measure for Ontario. Ontario Med Rev. 2000;67:33–52.
Matheson FI, Dunn JR, Smith KL, Moineddin R, Glazier RH. Development of the Canadian Marginalization Index: a new tool for the study of inequality. Can J Public Health. 2012;103:S12–6.
Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82:703–10.
The Johns Hopkins ACG® System. The Johns Hopkins University. Accessed January 22, 2020. https://www.hopkinsacg.org.
Reid RJ, MacWilliam L, Verhulst L, Roos N, Atkinson M. Performance of the ACG case-mix system in two Canadian provinces. Med Care. 2001;39:86–99.
Reid RJ, Roos NP, MacWilliam L, Frohlich N, Black C. Assessing population health care need using a claims-based ACG morbidity measure: a validation analysis in the Province of Manitoba. Health Serv Res. 2002;37:1345–64.
Weiner JP, Starfield BH, Steinwachs DM, Mumford LM. Development and application of a population-oriented measure of ambulatory care case-mix. Med Care. 1991;29:452–72.
Starfield B, Weiner J, Mumford L, Steinwachs D. Ambulatory care groups: a categorization of diagnoses for research and management. Health Serv Res. 1991;26:53–74.
Government of Ontario. Public Hospitals Act Regulation 964—Classification of Hospitals. Ministry of Health and Long-Term Care, 2009. Accessed March 26, 2020. http://www.health.gov.on.ca/en/common/system/services/hosp/hospcode.aspx.
Ontario Network of Transfusion Coordinators. Accessed Feb 13, 2020. https://www.ontracprogram.com/.
Ontario Regional Blood Coordinating Network. Accessed January 28, 2020. https://transfusionontario.org/en/.
Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38:1228–34.
Mamdani M, Sykora K, Li P, et al. Reader’s guide to critical appraisal of cohort studies: 2. Assessing potential for confounding. BMJ. 2005;330:960–2.
Cochran WG. Some methods for strengthening the common χ2 tests. Biometrics 1954;10.
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6.
McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–3.
Freedman J. The ONTraC Ontario program in blood conservation. Transfus Apher Sci. 2014;50:32–6.
Ecker BL, Simmons KD, Zaheer S, et al. Blood transfusion in major abdominal surgery for malignant tumors: a trend analysis using the National Surgical Quality Improvement Program. JAMA Surg. 2016;151:518-25.
Odell DD, Bilimoria KY. Evaluating appropriate blood transfusion in cancer surgery. JAMA Surg. 2016;151:525–6.
Leijssen LGJ, Dinaux AM, Kunitake H, Bordeianou LG, Berger DL. Is there a drawback of converting a laparoscopic colectomy in colon cancer? JSurgRes. 2018;232:595–604.
Schwenk W, Haase O, Neudecker J, Muller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005:CD003145.
McNally SJ, Revie EJ, Massie LJ, et al. Factors in perioperative care that determine blood loss in liver surgery. HPB. 2012;14:236–41.
Osorio J, Jericó C, Miranda C, et al. Perioperative transfusion management in gastric cancer surgery: analysis of the Spanish subset of the EURECCA Oesophago-Gastric Cancer Registry. Cirugía Española (English Edition). 2018;96:546–54.
American Society of Anesthesiologists Task Force on Perioperative Blood M. Practice guidelines for perioperative blood management: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management*. Anesthesiology. 2015;122:241–75.
Acknowledgments
We thank the Ontario Regional Blood Coordinating Network (ORBCoN) and the Ontario Transfusion Coordinators (ONTraC) program for their support. This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). Parts of this material are based on data and/or information compiled and provided by CIHI. However, the analyses, conclusions, opinions, and statements expressed in the material are those of the author(s), and not necessarily those of CIHI. Parts of this material are based on data and information provided by Cancer Care Ontario (CCO). The opinions, results, view, and conclusions reported in this paper are those of the authors and do not necessarily reflect those of CCO. No endorsement by CCO is intended or should be inferred. Parts of this work were presented at American Society of Clinical Oncology Gastrointestinal Cancer Symposium, San Francisco, CA, January 23, 2020; University of Toronto Department of Surgery Gallie Day, Toronto, Canada, May 8, 2020; University of Toronto Division of General Surgery Annual Assembly, Toronto, Canada, May 14, 2020.
Funding
This study received funding from the following: Ministry of Health and Long-Term Care Clinician Investigator Program, Sunnybrook Alternative Funding Plan Innovation Grant, and Canadian Institute of Health Research New Investigator Award. The funding sources had no role in the design and conduct of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no relevant conflicts of interest. J.C. has received research support from Canadian Blood Services and Octapharma. Y.L. has received research support from Novartis and Octapharma, and has consulted for Amgen and Pfizer. J.H. has received speaking honoraria from Ipsen Biopharmaceuticals Canada and Advanced Accelerator Applications.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zuckerman, J., Coburn, N., Callum, J. et al. Declining Use of Red Blood Cell Transfusions for Gastrointestinal Cancer Surgery: A Population-Based Analysis. Ann Surg Oncol 28, 29–38 (2021). https://doi.org/10.1245/s10434-020-09291-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09291-y