Abstract
Background
Surgical resection is the best treatment for colorectal liver metastases with good response to chemotherapy and in the absence of extrahepatic disease.1 With the amelioration of surgical technique, primary and recurrent colorectal liver metastases with venous invasion can be resected safely under short total vascular exclusion (TVE), and associated right thoracotomy can have a major benefit if resection at the hepato-caval junction is planned.2 The availability of the peritoneum as an autologous graft for venous reconstruction considerably facilitates the task of the surgeon.3 In this video, we present a patient who had staged double liver resection, double TVE, and double venous reconstruction by a peritoneal graft on the vena cava and the hepatic vein.
Methods
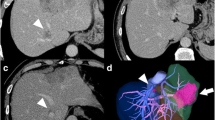
In March 2017, a 47-year-old female was diagnosed with rectal cancer and synchronous liver metastases, microsatellite stability, and Kras mutation. The patient received folinic acid, fluorouracil, and oxaliplatin (FOLFOX) chemotherapy, with good response and a decrease in tumor markers. After chemotherapy, a computed tomography (CT) scan showed one lesion located on the right liver with lateral invasion of the vena cava, and another lesion located in segment I. A liver-first strategy was decided and, in October 2017, the patient had a right hepatectomy extended to segment I and partially on the diaphragm, with lateral resection of the vena cava under isolated clampage of the vena cava and reconstruction with a peritoneal graft (60 mm). The patient received FOLFOX adjuvant chemotherapy for 3 months, and, while under radiotherapy for the rectal cancer, recurrence was diagnosed on the left liver lobe (two lesions), with lateral invasion of the left hepatic vein. Chemotherapy was shifted to folinic acid, fluorouracil, and irinotecan (FOLFIRI)–Avastin, with good response, allowing resection of the primary (T3N0M1), followed by adjuvant chemotherapy. In May 2019, the patient underwent two large resections on the left liver, including one under TVE, with opening of the diaphragm and intrathoracic control of the vena cava. The left hepatic vein was reconstructed laterally with a peritoneal graft (30 mm).
Results
Postoperative outcome was uneventful and the two hospital stays were 12 and 15 days, respectively. For the first hepatectomy, pathological examination showed two lesions (80 and 50 mm) with a residual tumor at 10% and R0 resection, and, for the second resection, pathological examination showed two lesions (18 and 20 mm) with residual tumor at 40–60% and R0 resection. In both cases, the tumor was in contact with the resected vein without wall infiltration. The reconstructed vena cava and hepatic vein were patent without stenosis. The patient is disease-free 3 years after the diagnosis.
Conclusion
Improvements in surgical technique combined with short TVE and associated thoracotomy allow some complicated liver resections to be performed safely. The use of the peritoneum for venous reconstruction is of great benefit in relation to safety and availability, especially in ‘redo’ liver surgery where intense adhesions can be encountered.
Similar content being viewed by others
References
Creasy JM, Sadot E, Koerkamp BG, Chou JF, Gonen M, Kemeny NE, et al. Actual 10-year survival after hepatic resection of colorectal liver metastases: what factors preclude cure? Surgery. 2018;163(6):1238–1244.
Dokmak S, Aussilhou B, Marchese T, Kardoun N, Cauchy F, Schneck AS, et al. Right trisectionectomy and caval reconstruction with peritoneal patch under short total vascular exclusion for hepatocellular carcinoma with tumoral thrombus in suprahepatic vena cava. Ann Surg Oncol. 2018;25(5):1152.
Dokmak S, Aussilhou B, Sauvanet A, Nagarajan G, Farges O, Belghiti J. Parietal peritoneum as an autologous substitute for venous reconstruction in hepatopancreatobiliary surgery. Ann Surg. 2015;262(2):366-71.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Safi Dokmak, Béatrice Aussilhou, Guillaume Levenson, Giovanni Guarneri, and Olivier Soubrane have no conflicts of interest in relation to this video.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
This video was presented at the 13th Congress of the European-African Hepato-Pancreato-Biliary Association, Amsterdam, The Netherlands, 2–5 June 2019, and the Americas Hepato-Pancreato-Biliary Association Annual Meeting, Miami, Florida, USA, 5–8 March 2020. (MP4 308688 kb)
Rights and permissions
About this article
Cite this article
Dokmak, S., Aussilhou, B., Levenson, G. et al. Staged Double Hepatectomy, Double Total Vascular Exclusion, and Double Venous Reconstruction by Peritoneal Patches in One Patient with Colorectal Liver Metastases. Ann Surg Oncol 28, 2028–2029 (2021). https://doi.org/10.1245/s10434-020-09155-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09155-5