Abstract
Background
The pathological tumor classification of distal cholangiocarcinoma in the American Joint Committee on Cancer (AJCC) Cancer Staging Manual 8th edition is based on invasive depth, whereas that of perihilar cholangiocarcinoma (PHCC) continues to be layer-based. We aimed to clarify whether invasive depth measurement based on invasive tumor thickness (ITT) could help determine postoperative prognosis in patients with PHCC.
Methods
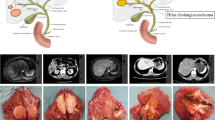
We enrolled 184 patients with PHCC who underwent hepatectomy plus extrahepatic bile duct resection or hepatopancreatoduodenectomy with curative intent. ITT was measured using simple definitions according to the sectioning direction or gross tumor pattern.
Results
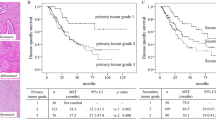
The median ITT was 5.8 mm (range 0.7–15.5). Using the recursive partitioning technique, ITT was classified into grades A (ITT < 2 mm, n = 9), B (2 mm ≤ ITT < 5 mm, n = 68), C (5 mm ≤ ITT < 11 mm, n = 81), and D (11 mm < ITT, n = 26). The median survival times (MSTs) in patients with grade B, C, or D were 90.8, 44.6, and 21.1 months, respectively (patients with grade A did not reach the MST). There were significant differences in postoperative prognosis between ITT grades (A vs. B, p = 0.027; B vs. C, p < 0.001; C vs. D, p = 0.004). Through multivariate analysis, regional node metastasis, invasive carcinoma at the resected margin, and ITT grade were determined as independent prognostic factors.
Conclusion
ITT could be measured using simple methods and may be used to stratify postoperative prognosis in patients with PHCC.




Similar content being viewed by others
References
Amin MB, Edge S, Greene F, et al. AJCC Cancer Staging Manual. 8th ed. New York: Springer; 2016.
Greene FL, Page DL, FIeming ID, Fritz A, Balch CM, Haller DG. American Joint Committee on Cancer (AJCC) Cancer Staging Manual. 6th ed. New York: Springer; 2002.
Edge S, Byrd DR, Compton CC, Fritz AG, Greene F, Trotti A. AJCC Cancer Staging Manual. 7th ed. New York: Springer; 2010.
Moon A, Choi DW, Choi SH, Heo JS, Jang KT. Validation of T stage according to depth of invasion and N stage subclassification based on number of metastatic lymph nodes for distal extrahepatic bile duct (EBD) carcinoma. Medicine (Baltimore). 2015;94(50):e2064.
Postlewait LM, Ethun CG, Le N, et al. Proposal for a new T-stage classification system for distal cholangiocarcinoma: a 10-institution study from the U.S. Extrahepatic Biliary Malignancy Consortium. HPB (Oxford). 2016;18(10):793–799.
Aoyama H, Ebata T, Hattori M, et al. Reappraisal of classification of distal cholangiocarcinoma based on tumour depth. Br J Surg. 2018;105(7):867–75.
Ruzzenente A, Bagante F, Ardito F, et al. Comparison of the 7th and 8th editions of the American Joint Committee on Cancer Staging Systems for perihilar cholangiocarcinoma. Surgery. 2018;164(2):244–50.
Shinohara K, Ebata T, Shimoyama Y, et al. Proposal for a new classification for perihilar cholangiocarcinoma based on tumour depth. Br J Surg. 2019;106(4):427–35.
Hong SM, Pawlik TM, Cho H, et al. Depth of tumor invasion better predicts prognosis than the current American Joint Committee on Cancer T classification for distal bile duct carcinoma. Surgery. 2009;146(2):250–7.
Zhao Y, Nakanishi Y, Ogino M, et al. Validation study of tumor invasive thickness for postoperative prognosis in 110 patients who underwent pancreatoduodenectomy for distal cholangiocarcinoma at a single institution. Am J Surg Pathol. 2019;43(5):717–23.
de Jong MC, Hong SM, Augustine MM, et al. Hilar cholangiocarcinoma: tumor depth as a predictor of outcome. Arch Surg. 2011;146(6):697–703.
Kondo S, Hirano S, Ambo Y, et al. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg. 2004;240(1):95–101.
Hirano S, Kondo S, Tanaka E, et al. Outcome of surgical treatment of hilar cholangiocarcinoma: a special reference to postoperative morbidity and mortality. J Hepatobiliary Pancreat Sci. 2010;17(4):455–62.
Lee JW, Um SH, Lee JB, Mun J, Cho H. Scoring and staging systems using cox linear regression modeling and recursive partitioning. Methods Inf Med. 2006;45(1):37–43.
Hong SM, Cho H, Moskaluk CA, Yu E. Measurement of the invasion depth of extrahepatic bile duct carcinoma: an alternative method overcoming the current T classification problems of the AJCC staging system. Am J Surg Pathol. 2007;31(2):199–206.
Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15(4):361–87.
Schroder MS, Culhane AC, Quackenbush J, Haibe-Kains B. survcomp: an R/Bioconductor package for performance assessment and comparison of survival models. Bioinformatics. 2011;27(22):3206–8.
Acknowledgment
The authors are grateful to Dr. Tomoko Mitsuhashi from the Department of Surgical Pathology, Hokkaido University Hospital, and Dr. Soichi Murakami, Dr. Yuma Ebihara, Dr. Yo Kurashima, Dr. Aya Matsui, Dr. Hajime Narasaki, Dr. Yusuke Watanabe, Dr. Mariko Ogino, Yusuke Yoshida, and Hiroyuki Yamamoto from the Department of Gastroenterological Surgery II, Hokkaido University Faculty of Medicine, for scientific advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mitsunobu Oba, Yoshitsugu Nakanishi, Toraji Amano, Keisuke Okamura, Takahiro Tsuchikawa, Toru Nakamura, Takehiro Noji, Toshimichi Asano, Kimitaka Tanaka, and Satoshi Hirano have no conflicts of interest or funding sources to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10434_2020_9135_MOESM1_ESM.tif
Bland–Altman plot for measurement of interobserver difference in measuring invasive tumor thickness. Differences were plotted against the means of each two measurements. The mean difference in ITT measurement between observers was 0.015 mm (solid line) with a standard deviation of 1.22. The 95% limits of agreement between observers was calculated as the mean difference ± 1.96 standard deviation of the difference (dotted lines). ITT invasive tumor thickness (TIFF 201 kb)
10434_2020_9135_MOESM2_ESM.tif
Log-rank statistic for cut-off points for invasive tumor thickness. Log-rank statistics for all possible cut-off points at 1-mm intervals for ITT were calculated. After the ITT value having the largest log-rank statistic was set up as the first cut-off point, patients were divided into two groups with higher and lower ITT values than the first cut-off point. Significant cut-off points were then further sought in each group. This procedure continued until there were no more significant cut-off points (when p > 0.05). The first cut-off point of ITT was determined as 5 mm. Subsequently, patients were classified into high (ITT ≥ 5 mm) and low (ITT < 5 mm) subgroups. Finally, the second cut-off points were found at 2 mm in the low subgroup and 11 mm in the high subgroup. ITT invasive tumor thickness (TIFF 201 kb)
Rights and permissions
About this article
Cite this article
Oba, M., Nakanishi, Y., Amano, T. et al. Stratification of Postoperative Prognosis by Invasive Tumor Thickness in Perihilar Cholangiocarcinoma. Ann Surg Oncol 28, 2001–2009 (2021). https://doi.org/10.1245/s10434-020-09135-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09135-9