Abstract
Background
Preoperative weight loss in esophageal cancer is reported to be associated with a poor prognosis. However, the impact of postoperative weight loss on the prognosis of patients with esophageal cancer remains unclear.
Methods
This study included 186 patients with esophageal squamous cell carcinoma who underwent surgery between January 2012 and January 2015. The relationship between weight loss 6 months after esophagectomy as well as the clinical factors and prognosis of patients was investigated.
Results
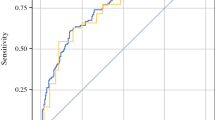
The mean weight loss rate for all the patients was 9.3% at 3 months, 10.8% at 6 months, 11.1% at 12 months, and 11.4% at 24 months after surgery. The patients with severe weight loss 6 months after surgery (≥ 12%) exhibited lower serum albumin levels and a lower prognostic nutrition index 6 months after esophagectomy than the patients with moderate weight loss (< 12%; p = 0.011 and 0.009, respectively). Although overall survival did not differ significantly between the two groups, for all the patients, severe weight loss was significantly associated with shortened overall survival for the cStages 3 and 4 patients (3-year overall survival rate, 76.6% in the moderate group vs 54.5% in the severe group; p = 0.042). The multivariate analyses identified only severe weight loss as an independent factor associated with worse overall survival for the cStages 3 and 4 patients (p = 0.034).
Conclusion
This study showed that postoperative weight loss negatively affected the prognosis for patients with advanced esophageal cancer, indicating the necessity of administering nutritional interventions to these patients to prevent postoperative weight loss.

Similar content being viewed by others
References
Bollschweiler E, Plum P, Monig SP, Holscher AH. Current and future treatment options for esophageal cancer in the elderly. Expert Opin Pharmacother. 2017;18:1001–10.
Gockel I, Niebisch S, Ahlbrand C, et al. Risk and complication management in esophageal cancer surgery: a review of the literature. Thorac Cardiovasc Surg. 2016;64:596–605.
Martin L, Lagergren J, Lindblad M, Rouvelas I, Lagergren P. Malnutrition after oesophageal cancer surgery in Sweden. Br J Surg. 2007;94:1496–500.
Lagergren J, Lagergren P, Recent developments in esophageal adenocarcinoma. CA Cancer J Clin. 2013;63:232–8.
Riccardi D, Allen K, Nutritional management of patients with esophageal and esophagogastric junction cancer. Cancer Control. 1999;6:64–72.
Anandavadivelan P, Wikman A, Johar A, Lagergren P. Impact of weight loss and eating difficulties on health-related quality of life up to 10 years after oesophagectomy for cancer. Br J Surg. 2018;105:410–8.
Elliott JA, Docherty NG, Eckhardt HG, et al. Weight loss, satiety, and the postprandial gut hormone response after esophagectomy: a prospective study. Ann Surg. 2017;266:82–90.
Baker M, Halliday V, Williams RN, Bowrey DJ. A systematic review of the nutritional consequences of esophagectomy. Clin Nutr. 2016;35:987–94.
Ludwig DJ, Thirlby RC, Low DE. A prospective evaluation of dietary status and symptoms after near-total esophagectomy without gastric emptying procedure. Am J Surg. 2001;181:454–8.
Haverkort EB, Binnekade JM, Busch OR, et al. Presence and persistence of nutrition-related symptoms during the first year following esophagectomy with gastric tube reconstruction in clinically disease-free patients. World J Surg. 2010;34:2844–52.
D’Journo XB, Ouattara M, Loundou A, et al.. Prognostic impact of weight loss in 1-year survivors after transthoracic esophagectomy for cancer. Dis Esophagus. 2012;25:527–34.
Martin L, Lagergren P. Risk factors for weight loss among patients surviving 5 years after esophageal cancer surgery. Ann Surg Oncol. 2015;22:610–6.
Liu J, Xie X, Zhou C, et al. Which factors are associated with actual 5-year survival of oesophageal squamous cell carcinoma? Eur J Cardiothorac Surg. 2012;41:e7–11.
Brierley JD, Gospodarowicz MK, Wittekind C. TNM Classification of Malignant Tumours. 8th ed. Wiley, New York, 2017.
Sugimura K, Miyata, H, Shinno N, et al. Prognostic factors for esophageal squamous cell carcinoma treated with neoadjuvant docetaxel/cisplatin/5-fluorouracil followed by surgery. Oncology. 2019;97:1–8.
Kubo Y, Miyata H, Sugimura K, et al. Prophylactic effect of premedication with intravenous magnesium on renal dysfunction in preoperative cisplatin-based chemotherapy for esophageal cancer. Oncology. 2019;97:319–26.
Miyata H, Sugimura K, Yamasaki M, et al. Clinical impact of the location of lymph node metastases after neoadjuvant chemotherapy for middle and lower thoracic esophageal cancer. Ann Surg Oncol. 2019;26:200–8.
Miyata H, Sugimura K, Yamasaki M, et al. Clinical implications of conversion surgery after induction therapy for T4b thoracic esophageal squamous cell carcinoma. Ann Surg Oncol. 2019;26:4737–43.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 1984;85:1001–5.
Kudou K, Saeki H, Nakashima Y, et al. C-reactive protein/albumin ratio is a poor prognostic factor of esophagogastric junction and upper gastric cancer. J Gastroenterol Hepatol. 2019;34:355–63.
Lagarde SM, de Boer JD, ten Kate FJ, et al. Postoperative complications after esophagectomy for adenocarcinoma of the esophagus are related to timing of death due to recurrence. Ann Surg. 2008;247:71–6.
Takahashi K, Watanabe M, Kozuki R, et al. Prognostic significance of skeletal muscle loss during early postoperative period in elderly patients with esophageal cancer. Ann Surg Oncol. 2019;26:3727–35.
Okada G, Momoki C, Habu D, et al. Effect of postoperative oral intake on prognosis for esophageal cancer. Nutrients. 2019;11:E1338.
Glickman JN, Torres C, Wang HH, et al. The prognostic significance of lymph node micrometastasis in patients with esophageal carcinoma. Cancer. 1999;85:769–78.
Sato F, Shimada Y, Li Z, et al. Lymph node micrometastasis and prognosis in patients with oesophageal squamous cell carcinoma. Br J Surg. 2001;88:426–32.
Marti A, Marcos A, Martinez JA. Obesity and immune function relationships. Obes Rev. 2001;2:131–40.
Ouattara M, D’Journo XB, Loundou A, et al. Body mass index kinetics and risk factors of malnutrition one year after radical oesophagectomy for cancer. Eur J Cardiothorac Surg. 2012;41:1088–93.
Kitagawa H, Namikawa T, Munekage M, et al. Analysis of factors associated with weight loss after esophagectomy for esophageal cancer. Anticancer Res. 2016;36:5409–12.
Schandl A, Kauppila JH, Anandavadivelan P, Johar A, Lagergren P. Predicting the risk of weight loss after esophageal cancer surgery. Ann Surg Oncol. 2019;26:2385–91.
Sugiyama K, Narita Y, Mitani S, et al. Baseline sarcopenia and skeletal muscle loss during chemotherapy affect survival outcomes in metastatic gastric cancer. Anticancer Res. 2018;38:5859–66.
Nagata M, Ito H, Yoshida T, et al. Risk factors for progressive sarcopenia 6 months after complete resection of lung cancer: what can thoracic surgeons do against sarcopenia? J Thorac Dis. 2020;12:307–318.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kubo, Y., Miyata, H., Sugimura, K. et al. Prognostic Implication of Postoperative Weight Loss After Esophagectomy for Esophageal Squamous Cell Cancer. Ann Surg Oncol 28, 184–193 (2021). https://doi.org/10.1245/s10434-020-08762-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08762-6