Abstract
There has historically been a significant divide in the approach to the management of lateral pelvic lymph nodes in patients with rectal cancer. These differing paradigms have developed based upon competing priorities. In the West, the circumferential resection margin has been the main focus because it is a strong predictor of local recurrence, distal recurrence, and survival. This approach was supplemented by radiation and chemotherapy to treat the lateral pelvic lymph nodes and micrometastatic disease. In the East, lateral pelvic lymph nodes are considered to be locoregional; thus, surgical treatment has traditionally included routine dissection of this compartment for low rectal cancers without the use of neoadjuvant chemoradiotherapy. However, neither approach has adequately addressed the important issue of lateral compartment recurrence in patients with clinically evident lateral pelvic lymph node metastasis. The aims of the review were to present the recent key studies and evolution of lateral pelvic lymph node management in locally advanced rectal cancer and secondly to propose a management strategy for the lateral compartment based on the current evidence.

Reproduced with permission from Fujita et al.16

Reproduced with permission from Akiyoshi et al.22

Reprinted from Kanemitsu et al.23

Reprinted with permission from Ogura et al.11

Reprinted with permission from Ogura et al.11

Reproduced with permission from Malakorn et al.36
Similar content being viewed by others
References
Hashiguchi Y, Muro K, Saito Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020; 25:1–42.
Georgiou P, Tan E, Gouvas N, et al. Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol. 2009; 10:1053–62.
Kusters M, Beets GL, van de Velde CJ, et al. A comparison between the treatment of low rectal cancer in Japan and the Netherlands, focusing on the patterns of local recurrence. Ann Surg. 2009; 249:229–35.
Yano H, Moran BJ. The incidence of lateral pelvic side-wall nodal involvement in low rectal cancer may be similar in Japan and the West. Br J Surg. 2008; 95:33–49.
Quirke P, Durdey P, Dixon MF, Williams NS. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet. 1986; 2:996–9.
Quirke P, Steele R, Monson J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet. 2009; 373:821–8.
Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol. 2008; 26:303–12.
Sammour T, Chang GJ. Lateral pelvic lymph node dissection and radiation treatment for rectal cancer: mutually exclusive or mutually beneficial? Ann Gastroenterol Surg. 2018; 2:348–50.
Sammour T, Chang GJ. Lateral node dissection in low rectal cancer: time for a global approach? Ann Surg. 2017; 266:208–9.
Malakorn S, Chang GJ. Treatment of rectal cancer in the east and west: should it be different? Surgery. 2017; 162:315–6.
Ogura A, Konishi T, Cunningham C, et al. Neoadjuvant (chemo)radiotherapy with total mesorectal excision only is not sufficient to prevent lateral local recurrence in enlarged nodes: results of the multicenter lateral node study of patients with low cT3/4 rectal cancer. J Clin Oncol. 2019; 37:33–43.
Sugihara K, Kobayashi H, Kato T, et al. Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum. 2006; 49:1663–72.
Moriya Y, Sugihara K, Akasu T, Fujita S. Nerve-sparing surgery with lateral node dissection for advanced lower rectal cancer. Eur J Cancer. 1995; 31A:1229–32.
Sugihara K, Moriya Y, Akasu T, Fujita S. Pelvic autonomic nerve preservation for patients with rectal carcinoma. Oncologic and functional outcome. Cancer. 1996; 78:1871–80.
Moriya Y, Sugihara K, Akasu T, Fujita S. Importance of extended lymphadenectomy with lateral node dissection for advanced lower rectal cancer. World J Surg. 1997; 21:728–32.
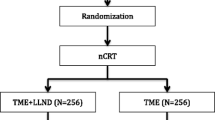
Fujita S, Mizusawa J, Kanemitsu Y, et al. Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212): a multicenter, randomized controlled, noninferiority trial. Ann Surg. 2017; 266:201–7.
Tsukamoto S, Fujita S, Ota M, et al. Long-term follow-up of the randomized trial of mesorectal excision with or without lateral lymph node dissection in rectal cancer (JCOG0212). Br J Surg. 2020; 107:586–94.
Peeters KC, Marijnen CA, Nagtegaal ID, et al. The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg. 2007; 246:693–701.
Fujita S, Akasu T, Mizusawa J, et al. Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol. 2012; 13:616–21.
Saito S, Fujita S, Mizusawa J, et al. Male sexual dysfunction after rectal cancer surgery: Results of a randomized trial comparing mesorectal excision with and without lateral lymph node dissection for patients with lower rectal cancer: Japan Clinical Oncology Group Study JCOG0212. Eur J Surg Oncol. 2016; 42:1851–8.
Weiser MR. AJCC 8th edition: colorectal cancer. Ann Surg Oncol. 2018; 25:1454–5.
Akiyoshi T, Watanabe T, Miyata S, et al. Results of a Japanese nationwide multi-institutional study on lateral pelvic lymph node metastasis in low rectal cancer: is it regional or distant disease? Ann Surg. 2012; 255:1129–34.
Kanemitsu Y, Komori K, Shida D, et al. Potential impact of lateral lymph node dissection (LLND) for low rectal cancer on prognoses and local control: a comparison of 2 high-volume centers in Japan that employ different policies concerning LLND. Surgery. 2017; 162:303–14.
Ogura A, Konishi T, Beets GL, et al. Lateral nodal features on restaging magnetic resonance imaging associated with lateral local recurrence in low rectal cancer after neoadjuvant chemoradiotherapy or radiotherapy. JAMA Surg. 2019. https://doi.org/10.1001/jamasurg.2019.2172.
Nagasaki T, Akiyoshi T, Fujimoto Y, et al. Preoperative chemoradiotherapy might improve the prognosis of patients with locally advanced low rectal cancer and lateral pelvic lymph node metastases. World J Surg. 2017; 41:876–83.
Taylor FG, Quirke P, Heald RJ, et al. Preoperative magnetic resonance imaging assessment of circumferential resection margin predicts disease-free survival and local recurrence: 5-year follow-up results of the MERCURY study. J Clin Oncol. 2014; 32:34–43.
Kim TH, Jeong SY, Choi DH, et al. Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol. 2008; 15:729–37.
Kim MJ, Kim TH, Kim DY, et al. Can chemoradiation allow for omission of lateral pelvic node dissection for locally advanced rectal cancer? J Surg Oncol. 2015; 111:459–64.
Kim TG, Park W, Choi DH, et al. Factors associated with lateral pelvic recurrence after curative resection following neoadjuvant chemoradiotherapy in rectal cancer patients. Int J Colorectal Dis. 2014; 29:193–200.
Kusters M, Slater A, Muirhead R, et al. What to do with lateral nodal disease in low locally advanced rectal cancer? A call for further reflection and research. Dis Colon Rectum. 2017; 60:577–85.
Atef Y, Koedam TW, van Oostendorp SE, Bonjer HJ, Wijsmuller AR, Tuynman JB. Lateral pelvic lymph node metastases in rectal cancer: a systematic review. World J Surg. 2019; 43:3198–206.
Kusters M, van de Velde CJ, Beets-Tan RG, et al. Patterns of local recurrence in rectal cancer: a single-center experience. Ann Surg Oncol. 2009; 16:289–96.
Beppu N, Kimura F, Aihara T, et al. Patterns of local recurrence and oncologic outcomes in T3 low rectal cancer (≤ 5 cm from the anal verge) treated with short-course radiotherapy with delayed surgery: outcomes in T3 low rectal cancer treated with short-course radiotherapy with delayed surgery. Ann Surg Oncol. 2017; 24:219–26.
Akiyoshi T, Ueno M, Matsueda K, et al. Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol. 2014; 21:189–96.
Ishihara S, Kawai K, Tanaka T, et al. Oncological outcomes of lateral pelvic lymph node metastasis in rectal cancer treated with preoperative chemoradiotherapy. Dis Colon Rectum. 2017; 60:469–76.
Malakorn S, Yang Y, Bednarski BK, et al. Who should get lateral pelvic lymph node dissection after neoadjuvant chemoradiation? Dis Colon Rectum. 2019; 62:1158–66.
Akiyoshi T, Matsueda K, Hiratsuka M, et al. Indications for lateral pelvic lymph node dissection based on magnetic resonance imaging before and after preoperative chemoradiotherapy in patients with advanced low-rectal cancer. Ann Surg Oncol. 2015; 22 Suppl 3:S614–20.
Ishihara S, Kanemitsu Y, Murono K, et al. Oncological benefit of lateral pelvic lymph node dissection for rectal cancer treated without preoperative chemoradiotherapy: a multicenter retrospective study using propensity score analysis. Int J Colorectal Dis. 2016; 31:1315–21.
Ogura A, Akiyoshi T, Nagasaki T, et al. Feasibility of laparoscopic total mesorectal excision with extended lateral pelvic lymph node dissection for advanced lower rectal cancer after preoperative chemoradiotherapy. World J Surg. 2017; 41:868–75.
Kim MJ, Hur BY, Lee ES, et al. Prediction of lateral pelvic lymph node metastasis in patients with locally advanced rectal cancer with preoperative chemoradiotherapy: focus on MR imaging findings. PLoS One. 2018; 13:e0195815.
Zhang X, Wei M, Deng X, Wang Z, He D. Is lateral lymph node dissection necessary for node size < 5 mm after neoadjuvant chemoradiation? Dis Colon Rectum. 2020; 63:e41–2.
Chang GJ, Holliday EB, Malakorn S. The authors reply. Dis Colon Rectum. 2020; 63:e43.
Acknowledgment
None.
Funding
Sources of support: This study was supported in part by the Aman Trust (GJC), the Andrews Family Fund (GJC), and National Institutes of Health/National Cancer Institute Grant CA016672 (The University of Texas MD Anderson Cancer Center Support Grant). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of data; preparation, review, or approval of the manuscript; and decision to submit for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr GJ Chang is a consultant for Medicaroid.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peacock, O., Chang, G.J. The Landmark Series: Management of Lateral Lymph Nodes in Locally Advanced Rectal Cancer. Ann Surg Oncol 27, 2723–2731 (2020). https://doi.org/10.1245/s10434-020-08639-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08639-8