Abstract
Introduction
The objective of the current study was to comprehensively assess the change of practice in hepatobiliary surgery by determining the rates and the trends of textbook outcomes (TO) among patients undergoing surgery for primary liver cancer over time.
Methods
Patients undergoing curative-intent resection for primary liver malignancies, including hepatocellular carcinoma (HCC) and intrahepatic cholangiocarcinoma (ICC) between 2005 and 2017 were analyzed using a large, international multi-institutional dataset. Rates of TO were assessed over time. Factors associated with achieving a TO and the impact of TO on long-term survival were examined.
Results
Among 1829 patients, 944 (51.6%) and 885 (48.4%) individuals underwent curative-intent resection for HCC and ICC, respectively. Over time, patients were older, more frequently had ASA class > 2, albumin-bilirubin grade 2/3, major vascular invasion and more frequently underwent major liver resection (all p < 0.05). Overall, a total of 1126 (62.0%) patients achieved a TO. No increasing trends in TO rates were noted over the years (ptrend = 0.90). In addition, there was no increasing trend in the TO rates among patients undergoing either major (ptrend = 0.39) or minor liver resection (ptrend = 0.63) over the study period. Achieving a TO was independently associated with 26% and 37% decreased hazards of death among ICC (HR 0.74, 95%CI 0.56–0.97) and HCC patients (HR 0.63, 95%CI 0.46–0.85), respectively.
Conclusion
Approximately 6 in 10 patients undergoing surgery for primary liver tumors achieved a TO. While TO rates did not increase over time, TO was associated with better long-term outcomes following liver resection for both HCC and ICC.



Similar content being viewed by others

References
Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
Liu Z, Jiang Y, Yuan H, et al. The trends in incidence of primary liver cancer caused by specific etiologies: results from the global burden of disease study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70(4):674–83.
Petrick JL, Kelly SP, Altekruse SF, McGlynn KA, Rosenberg PS. Future of hepatocellular carcinoma incidence in the united states forecast through 2030. J Clin Oncol. 2016;34(15):1787–94.
Tsilimigras DI, Bagante F, Sahara K, et al. Prognosis after resection of barcelona clinic liver cancer (BCLC) stage 0, A, and B hepatocellular carcinoma: a comprehensive assessment of the current BCLC classification. Ann Surg Oncol. 2019;26(11):3693–700.
Dimick JB, Staiger DO, Baser O, Birkmeyer JD. Composite measures for predicting surgical mortality in the hospital. Health Aff (Millwood). 2009;28(4):1189–98.
Dimick JB, Birkmeyer NJ, Finks JF, et al. Composite measures for profiling hospitals on bariatric surgery performance. JAMA Surg. 2014;149(1):10–6.
Dimick JB, Staiger DO, Osborne NH, Nicholas LH, Birkmeyer JD. Composite measures for rating hospital quality with major surgery. Health Serv Res. 2012;47(5):1861–79.
Staiger DO, Dimick JB, Baser O, Fan Z, Birkmeyer JD. Empirically derived composite measures of surgical performance. Med Care. 2009;47(2):226–33.
Merath K, Chen Q, Bagante F, et al. Textbook outcomes among medicare patients undergoing hepatopancreatic surgery. Ann Surg. 2018. https://doi.org/10.1097/SLA.0000000000003105.
Merath K, Chen Q, Bagante F, et al. A multi-institutional international analysis of textbook outcomes among patients undergoing curative-intent resection of intrahepatic cholangiocarcinoma. JAMA Surg. 2019;154:e190571.
van Roessel S, Mackay TM, van Dieren S, et al. Textbook outcome: nationwide analysis of a novel quality measure in pancreatic surgery. Ann Surg. 2019;271:155–62.
Wu L, Tsilimigras DI, Paredes AZ, et al. Trends in the incidence, treatment and outcomes of patients with intrahepatic cholangiocarcinoma in the USA: facility type is associated with margin status, use of lymphadenectomy and overall survival. World J Surg. 2019;43(7):1777–87.
Tsilimigras DI, Sahara K, Moris D, et al. Effect of surgical margin width on patterns of recurrence among patients undergoing R0 hepatectomy for T1 hepatocellular carcinoma: an international multi-institutional analysis. J Gastrointest Surg. 2019. https://doi.org/10.1007/s11605-019-04275-0.
Tsilimigras DI, Hyer JM, Moris D, et al. Prognostic utility of albumin-bilirubin grade for short- and long-term outcomes following hepatic resection for intrahepatic cholangiocarcinoma: a multi-institutional analysis of 706 patients. J Surg Oncol. 2019;120(2):206–13.
Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg. 2005;12(5):351–5.
Amin MB, Greene FL, Edge SB, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67(2):93–9.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Luu C, Goldstein L, Goldner B, Schoellhammer HF, Chen SL. Trends in radiotherapy after breast-conserving surgery in elderly patients with early-stage breast cancer. Ann Surg Oncol. 2013;20(10):3266–73.
Virani S, Michaelson JS, Hutter MM, et al. Morbidity and mortality after liver resection: results of the patient safety in surgery study. J Am Coll Surg. 2007;204(6):1284–92.
Spolverato G, Yakoob MY, Kim Y, et al. Impact of complications on long-term survival after resection of intrahepatic cholangiocarcinoma. Cancer. 15 2015;121(16):2730–9.
Tsilimigras DI, Mehta R, Moris D, et al. Utilizing machine learning for pre- and postoperative assessment of patients undergoing resection for BCLC-0, A and B hepatocellular carcinoma: implications for resection beyond the BCLC guidelines. Ann Surg Oncol. 2019;27:866–74
Abulkhir A, Limongelli P, Healey AJ, et al. Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg. 2008;247(1):49–57.
Cloyd JM, Mizuno T, Kawaguchi Y, et al. Comprehensive complication index validates improved outcomes over time despite increased complexity in 3707 consecutive hepatectomies. Ann Surg. 2020;271(4):724-731.
Kokudo T, Hasegawa K, Matsuyama Y, et al. Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. J Hepatol. 2016;65(5):938–43.
Neuwirth MG, Bierema C, Sinnamon AJ, et al. Trends in major upper abdominal surgery for cancer in octogenarians: has there been a change in patient selection? Cancer. 2018;124(1):125–35.
Busweiler LA, Schouwenburg MG, van Berge Henegouwen MI, et al. Textbook outcome as a composite measure in oesophagogastric cancer surgery. Br J Surg. 2017;104(6):742–50.
Kolfschoten NE, Kievit J, Gooiker GA, et al. Focusing on desired outcomes of care after colon cancer resections; hospital variations in ‘textbook outcome’. Eur J Surg Oncol. 2013;39(2):156–63.
Karthaus EG, Lijftogt N, Busweiler LAD, et al. Textbook outcome: a composite measure for quality of elective aneurysm surgery. Ann Surg. 2017;266(5):898–904.
Liu J, Reid J, Leopardi L, Edwards S, Trochsler M, Maddern G. Progress towards near-zero 90-day mortality: 388 consecutive hepatectomies over a 16-year period. ANZ J Surg. 2019;89(9):1144–7.
Chan J, Bradshaw L, Houli N, et al. Outcomes of central hepatectomy versus extended hepatectomy. Hepatobiliary Pancreat Dis Int. 2019;18(3):249–54.
Beal EW, Tumin D, Kabir A, et al. Trends in the mortality of hepatocellular carcinoma in the United States. J Gastrointest Surg. 2017;21(12):2033–8.
Sasaki A, Aramaki M, Kawano K, et al. Intrahepatic peripheral cholangiocarcinoma: mode of spread and choice of surgical treatment. Br J Surg. 1998;85(9):1206–9.
Buettner S, van Vugt JL, JN IJ, Groot Koerkamp B. Intrahepatic cholangiocarcinoma: current perspectives. OncoTargets Ther. 2017;10:1131–42.
Chung YE, Kim MJ, Park YN, et al. Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics. 2009;29(3):683–700.
Idrees JJ, Merath K, Gani F, et al. Trends in centralization of surgical care and compliance with National Cancer Center Network guidelines for resected cholangiocarcinoma. HPB (Oxford). 2019;21(8):981–9.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
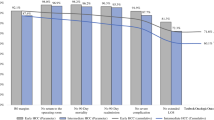
Supplemental Fig. 1
Textbook outcome rates stratified by procedure type (TIFF 85 kb)
Supplemental Fig. 2
Textbook outcome rates among patients treated at Eastern versus Western institutions (TIFF 189 kb)
Supplemental Fig. 3
Incidence of overall textbook outcome and individual TO components among patients treated in the early (2005–2008) versus late (2013–2017) study periods on PSM analysis (TIFF 482 kb)
Supplemental Fig. 4
Kaplan Meier curves demonstrating differences in overall survival among patients treated in the early (2005–2008) versus late (2013–2017) study periods on PSM analysis (TIFF 98 kb)
Rights and permissions
About this article
Cite this article
Tsilimigras, D.I., Sahara, K., Moris, D. et al. Assessing Textbook Outcomes Following Liver Surgery for Primary Liver Cancer Over a 12-Year Time Period at Major Hepatobiliary Centers. Ann Surg Oncol 27, 3318–3327 (2020). https://doi.org/10.1245/s10434-020-08548-w
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08548-w