Abstract
Introduction
Intrahepatic cholangiocarcinoma (ICC) remains an uncommon disease with a rising incidence worldwide. We sought to identify trends in therapeutic approaches and differences in patient outcomes based on facility types.
Methods
Between January 1, 2004, and December 31, 2015, a total of 27,120 patients with histologic diagnosis of ICC were identified in the National Cancer Database and were enrolled in this study.
Results
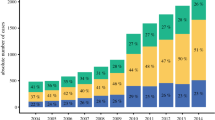
The incidence of ICC patients increased from 1194 in 2004 to 3821 in 2015 with an average annual increase of 4.16% (p < 0.001). Median survival of the cohort improved over the last 6 years of the study period (2004–2009: 8.05 months vs. 2010–2015: 9.49 months; p < 0.001). Among surgical patients (n = 5943, 21.9%), the incidence of R0 resection, lymphadenectomy and harvest of ≥6 lymph nodes increased over time (p < 0.001). Positive surgical margins (referent R0: R1, HR 1.49, 95% CI 1.24–1.79, p < 0.001) and treatment at community cancer centers (referent academic centers; HR 1.24, 95% CI 1.04–1.49, p = 0.023) were associated with a worse prognosis. Patients treated at academic centers had higher rates of R0 resection (72.4% vs. 67.7%; p = 0.006) and lymphadenectomy (55.6% vs. 49.5%, p = 0.009) versus community cancer centers. Overall survival was also better at academic versus community cancer programs (median OS: 11 months versus 6 months, respectively; p < 0.001).
Conclusions
The incidence of ICC has increased over the last 12 years in the USA with a moderate improvement in survival over time. Treatment at academic cancer centers was associated with higher R0 resection and lymphadenectomy rates, as well as improved OS for patients with ICC.




Similar content being viewed by others
References
Chang KY, Chang JY, Yen Y (2009) Increasing incidence of intrahepatic cholangiocarcinoma and its relationship to chronic viral hepatitis. J Natl Compr Canc Netw 7(4):423–427 (PubMed PMID: 19406042)
Amini N, Ejaz A, Spolverato G, Kim Y, Herman JM, Pawlik TM (2014) Temporal trends in liver-directed therapy of patients with intrahepatic cholangiocarcinoma in the United States: a population-based analysis. J Surg Oncol 110(2):163–170. https://doi.org/10.1002/jso.23605 (PubMed PMID: 24676600)
Saha SK, Zhu AX, Fuchs CS, Brooks GA (2016) Forty-year trends in cholangiocarcinoma incidence in the U.S.: intrahepatic disease on the rise. Oncologist 21(5):594–599. https://doi.org/10.1634/theoncologist.2015-0446 (PubMed PMID: 27000463; PubMed Central PMCID: PMCPMC4861366)
Dhanasekaran R, Hemming AW, Zendejas I, George T, Nelson DR, Soldevila-Pico C et al (2013) Treatment outcomes and prognostic factors of intrahepatic cholangiocarcinoma. Oncol Rep 29(4):1259–1267. https://doi.org/10.3892/or.2013.2290 (PubMed PMID: 23426976; PubMed Central PMCID: PMCPMC3621732)
Chapman BC, Paniccia A, Hosokawa PW, Henderson WG, Overbey DM, Messersmith W et al (2017) Impact of facility type and surgical volume on 10-year survival in patients undergoing hepatic resection for hepatocellular carcinoma. J Am Coll Surg 224(3):362–372. https://doi.org/10.1016/j.jamcollsurg.2016.11.011 (PubMed PMID: 27923615)
Kommalapati A, Tella SH, Goyal G, Borad M, Alberts SR, Roberts L et al (2018) Association between treatment facility volume, therapy types and overall survival in patients with intrahepatic cholangiocarcinoma. HPB. https://doi.org/10.1016/j.hpb.2018.08.004. (PubMed PMID: 30266490)
Chu QD, Zhou M, Peddi P, Medeiros KL, Zibari GB, Shokouh-Amiri H et al (2017) Influence of facility type on survival outcomes after pancreatectomy for pancreatic adenocarcinoma. HPB 19(12):1046–1057. https://doi.org/10.1016/j.hpb.2017.04.017 (PubMed PMID: 28967535)
Hyder O, Sachs T, Ejaz A, Spolverato G, Pawlik TM (2013) Impact of hospital teaching status on length of stay and mortality among patients undergoing complex hepatopancreaticobiliary surgery in the USA. J Gastrointest Surg 17(12):2114–2122. https://doi.org/10.1007/s11605-013-2349-4 (PubMed PMID: 24072683; PubMed Central PMCID: PMCPMC3980573)
Zhang XF, Chakedis J, Bagante F, Chen Q, Beal EW, Lv Y et al (2018) Trends in use of lymphadenectomy in surgery with curative intent for intrahepatic cholangiocarcinoma. Br J Surg 105(7):857–866. https://doi.org/10.1002/bjs.10827 (PubMed PMID: 29656380)
Zhang XF, Bagante F, Chen Q, Beal EW, Lv Y, Weiss M et al (2018) Perioperative and long-term outcome of intrahepatic cholangiocarcinoma involving the hepatic hilus after curative-intent resection: comparison with peripheral intrahepatic cholangiocarcinoma and hilar cholangiocarcinoma. Surgery 163(5):1114–1120. https://doi.org/10.1016/j.surg.2018.01.001 (PubMed PMID: 29398035)
Boffa DJ, Rosen JE, Mallin K, Loomis A, Gay G, Palis B et al (2017) Using the national cancer database for outcomes research: a review. JAMA Oncol. 3(12):1722–1728. https://doi.org/10.1001/jamaoncol.2016.6905 (PubMed PMID: 28241198)
Edge SB, Compton CC (2009) American joint committee on cancer: AJCC cancer staging manual, 7th edn. Springer, New York
Greene FL (2002) AJCC cancer staging manual, 6th edn. Springer, New York
American College of Surgeons, National Cancer Database: Patient User File Data Dictionary Items. http://ncdbpuf.facs.org/?q=node/259. Accessed 1 Dec 2016
Beal EW, Tumin D, Moris D, Zhang XF, Chakedis J, Dilhoff M et al (2018) Cohort contributions to trends in the incidence and mortality of intrahepatic cholangiocarcinoma. Hepatobiliary Surg Nutr 7(4):270–276. Epub 2018/09/18. https://doi.org/10.21037/hbsn.2018.03.16. (PubMed PMID: 30221154; PubMed Central PMCID: PMCPMC6131266)
Spolverato G, Vitale A, Cucchetti A, Popescu I, Marques HP, Aldrighetti L et al (2015) Can hepatic resection provide a long-term cure for patients with intrahepatic cholangiocarcinoma? Cancer 121(22):3998–4006. https://doi.org/10.1002/cncr.29619 (PubMed PMID: 26264223)
Asiyanbola B, Chang D, Gleisner AL, Nathan H, Choti MA, Schulick RD et al (2008) Operative mortality after hepatic resection: Are literature-based rates broadly applicable? J Gastrointest Surg 12(5):842–851. https://doi.org/10.1007/s11605-008-0494-y (PubMed PMID: 18266046)
Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A et al (2010) Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 362(14):1273–1281. Epub 2010/04/09. https://doi.org/10.1056/nejmoa0908721. (PubMed PMID: 20375404)
Bagante F, Spolverato G, Weiss M, Alexandrescu S, Marques HP, Aldrighetti L, et al. (2018) Assessment of the lymph node status in patients undergoing liver resection for intrahepatic cholangiocarcinoma: the new eighth edition AJCC staging system. J Gastrointest Surg 22(1):52–59. Epub 2017/04/21. https://doi.org/10.1007/s11605-017-3426-x. (PubMed PMID: 28424987)
Guglielmi A, Ruzzenente A, Campagnaro T, Valdegamberi A, Bagante F, Bertuzzo F et al (2013) Patterns and prognostic significance of lymph node dissection for surgical treatment of perihilar and intrahepatic cholangiocarcinoma. J Gastrointest Surg 17(11):1917–1928. https://doi.org/10.1007/s11605-013-2331-1 (PubMed PMID: 24048613)
Kim Y, Moris DP, Zhang XF, Bagante F, Spolverato G, Schmidt C et al (2017) Evaluation of the 8th edition American Joint Commission on Cancer (AJCC) staging system for patients with intrahepatic cholangiocarcinoma: a surveillance, epidemiology, and end results (SEER) analysis. J Surg Oncol 116(6):643–650. https://doi.org/10.1002/jso.24720 (PubMed PMID: 28608424)
Zhang XF, Chen Q, Kimbrough CW, Beal EW, Lv Y, Chakedis J et al (2018) Lymphadenectomy for intrahepatic cholangiocarcinoma: Has nodal evaluation been increasingly adopted by surgeons over time? A national database analysis. J Gastrointest Surg 22(4):668–675. https://doi.org/10.1007/s11605-017-3652-2 (PubMed PMID: 29264768)
Ratti F, Cipriani F, Ariotti R, Gagliano A, Paganelli M, Catena M et al (2016) Safety and feasibility of laparoscopic liver resection with associated lymphadenectomy for intrahepatic cholangiocarcinoma: a propensity score-based case-matched analysis from a single institution. Surg Endosc 30(5):1999–2010. https://doi.org/10.1007/s00464-015-4430-4 (PubMed PMID: 26194257)
Yoh T, Hatano E, Nishio T, Seo S, Taura K, Yasuchika K et al (2016) Significant improvement in outcomes of patients with intrahepatic cholangiocarcinoma after surgery. World J Surg 40(9):2229–2236. https://doi.org/10.1007/s00268-016-3583-1 (PubMed PMID: 27255940)
Ercolani G, Vetrone G, Grazi GL, Aramaki O, Cescon M, Ravaioli M et al (2010) Intrahepatic cholangiocarcinoma: primary liver resection and aggressive multimodal treatment of recurrence significantly prolong survival. Ann Surg 252(1):107–114. https://doi.org/10.1097/SLA.0b013e3181e462e6 (PubMed PMID: 20531002)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lu Wu and Diamantis I. Tsilimigras contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Figure 1
Trends in the use of chemotherapy and radiotherapy among patients with ICC who received non-surgical treatment (TIFF 77 kb)
Supplemental Figure 2
Trends in the use of chemotherapy (a) and radiotherapy (b) among non-surgical patients treated at different facility settings (TIFF 1075 kb)
Rights and permissions
About this article
Cite this article
Wu, L., Tsilimigras, D.I., Paredes, A.Z. et al. Trends in the Incidence, Treatment and Outcomes of Patients with Intrahepatic Cholangiocarcinoma in the USA: Facility Type is Associated with Margin Status, Use of Lymphadenectomy and Overall Survival. World J Surg 43, 1777–1787 (2019). https://doi.org/10.1007/s00268-019-04966-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-04966-4