Abstract
Objective
We sought to examine the impact of primary tumor resection on survival in HER2+ stage IV breast cancer patients in the era of HER2 targeted therapy.
Methods
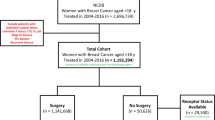
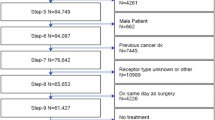
We conducted a retrospective cohort study of women with HER2+ stage IV breast cancer in the National Cancer Database from 2010 to 2012 comparing those who did and did not undergo definitive breast surgery.
Results
Of 3231 patients, treatment included primary site surgery in 35.0%; chemo/targeted therapy in 89.4%; endocrine therapy in 37.7%; and radiation in 31.8%. Surgery was associated with Medicare/other government (OR 1.36, 95% CI 1.03–1.81) or private insurance (OR 1.93, 95% CI 1.53–2.42) versus none/Medicaid, radiation (OR 2.10, 95% CI 1.76–2.51), chemo/targeted therapy (OR 1.99, 95% CI 1.47–2.70), and endocrine therapy (OR 1.73, 95% CI 1.40–2.14). Non-Hispanic Black versus White patients (OR 0.68, 95% CI 0.53–0.87) were less likely to have surgery. Overall mortality was associated with insurance (Medicare/other government versus none/Medicaid, HR 0.36, p < 0.0001), receipt of chemo/targeted therapy (HR 0.76, p = 0.008), endocrine therapy (HR 0.70, p = 0.0006), and radiation therapy (HR 1.33, p = 0.0009), NH Black versus White race/ethnicity (HR 1.39, p = 0.002), visceral versus bone-only metastases (HR 1.44, p = 0.0003), and lowest versus highest income quartile (HR 1.36, p = 0.01). Propensity score analysis showed surgery was associated with improved survival versus no surgery (HR 0.56, 95% CI 0.40–0.77).
Conclusions
Surgery of the primary site for metastatic HER2+ breast cancer is associated with improved overall survival in selected patients.


Similar content being viewed by others
References
Lu S, Wu J, Fang Y, et al. The impact of surgical excision of the primary tumor in stage IV breast cancer on survival: a meta-analysis. Oncotarget. 2018.
National Comprehensive Cancer Network. Breast Cancer (Version 1.2019). Accessed April 1, 2019.
Babiera GV, Rao R, Feng L, et al. Effect of primary tumor extirpation in breast cancer patients who present with stage IV disease and an intact primary tumor. Ann Surg Oncol. 2006;13(6):776–782.
Fields RC, Jeffe DB, Trinkaus K, et al. Surgical resection of the primary tumor is associated with increased long-term survival in patients with stage IV breast cancer after controlling for site of metastasis. Ann Surg Oncol. 2007;14(12):3345–3351.
Gnerlich J, Jeffe DB, Deshpande AD, Beers C, Zander C, Margenthaler JA. Surgical removal of the primary tumor increases overall survival in patients with metastatic breast cancer: analysis of the 1988–2003 SEER data. Ann Surg Oncol. 2007;14(8):2187–2194.
Khan SA, Stewart AK, Morrow M. Does aggressive local therapy improve survival in metastatic breast cancer? Surgery. 2002;132(4):620–627.
Rapiti E, Verkooijen HM, Vlastos G, et al. Complete excision of primary breast tumor improves survival of patients with metastatic breast cancer at diagnosis. J Clin Oncol. 2006;24(18):2743–2749.
Bafford AC, Burstein HJ, Barkley CR, et al. Breast surgery in stage IV breast cancer: impact of staging and patient selection on overall survival. Breast Cancer Res Treat. 2009;115(1):7–12.
Barbie TU, Golshan M. De novo stage 4 metastatic breast cancer: a surgical disease? Ann Surg Oncol. 2018;25(11):3109–3111.
Cady B, Nathan NR, Michaelson JS, Golshan M, Smith BL. Matched pair analyses of stage IV breast cancer with or without resection of primary breast site. Ann Surg Oncol. 2008;15(12):3384–3395.
Dominici L, Najita J, Hughes M, et al. Surgery of the primary tumor does not improve survival in stage IV breast cancer. Breast Cancer Res Treat. 2011;129(2):459–465.
Soran A, Ozmen V, Ozbas S, et al. Randomized trial comparing resection of primary tumor with no surgery in stage IV breast cancer at presentation: protocol MF07-01. Ann Surg Oncol. 2018;25(11):3141–3149.
Soran A. The role of loco-regional treatment in long-term quality of life in de novo stage IV breast cancer patient: protocol MF07-01Q. Paper presented at: Plenary presentation at the 20th annual meeting of the American Society of Breast Surgeons; May 4, 2019, 2019; Dallas, Texas.
Badwe R, Hawaldar R, Nair N, et al. Locoregional treatment versus no treatment of the primary tumour in metastatic breast cancer: an open-label randomised controlled trial. Lancet Oncol. 2015;16(13):1380–1388.
Hudis CA. Trastuzumab — mechanism of action and use in clinical practice. N Engl J Med. 2007;357(1):39–51.
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235(4785):177.
Slamon DJ, Godolphin W, Jones LA, et al. Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science. 1989;244(4905):707.
Dawood S, Broglio K, Buzdar AU, Hortobagyi GN, Giordano SH. Prognosis of women with metastatic breast cancer by HER2 status and trastuzumab treatment: an institutional-based review. J Clin Oncol. 2010;28(1):92–98.
Slamon DJ, Leyland-Jones B, Shak S, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–792.
Swain SM, Miles D, Kim S-B, et al. End-of-study analysis from the phase III, randomized, double-blind, placebo (Pla)-controlled CLEOPATRA study of first-line (1L) pertuzumab (P), trastuzumab (H), and docetaxel (D) in patients (pts) with HER2-positive metastatic breast cancer (MBC). J Clin Oncol. 2019;37(15_suppl):1020–1020.
Baselga J, Cortés J, Kim S-B, et al. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012;366(2):109–119.
Geyer CE, Forster J, Lindquist D, et al. Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med. 2006;355(26):2733–2743.
Jackisch C, Stroyakovskiy D, Pivot X, et al. Subcutaneous vs intravenous trastuzumab for patients with ERBB2-positive early breast cancer. JAMA Oncol. 2019;5(5):e190339.
Verma S, Miles D, Gianni L, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367(19):1783–1791.
Giuliano AE, Connolly JL, Edge SB, et al. Breast cancer—major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(4):290–303.
American College of Surgeons. CS site-specific factor 15, HER2: summary result of testing. http://web2.facs.org/cstage0205/breast/Breast_sbg.html. Accessed 1 Nov 2018.
American College of Surgeons. NCDB Analytic Stage Group. http://ncdbpuf.facs.org/content/analytic-stage-group-ajcc-alphanumeric. Accessed 1 Nov 2018.
American College of Surgeons. Charlson/Deyo score. http://ncdbpuf.facs.org/content/charlsondeyo-comorbidity-index. Accessed 1 Nov 2018.
American College of Surgeons. Surgery of the primary site: BREAST. http://ncdbpuf.facs.org/content/breast. Accessed 1 Nov 2018.
American College of Surgeons. Spanish origin. http://ncdbpuf.facs.org/content/spanish-origin. Accessed 1 Nov 2018.
American College of Surgeons. Immunotherapy. http://ncdbpuf.facs.org/content/immunotherapy. Accessed 1 Nov 2018.
Fisher B, Gunduz N, Coyle J, Rudock C, Saffer E. Presence of a growth-stimulating factor in serum following primary tumor removal in mice. Cancer Res. 1989;49(8):1996.
Ten Kate M, Hofland LJ, Van Grevenstein WMU, Van Koetsveld PV, Jeekel J, Van Eijck CHJ. Influence of proinflammatory cytokines on the adhesion of human colon carcinoma cells to lung microvascular endothelium. Int J Cancer. 2004;112(6):943–950.
Benish M, Bartal I, Goldfarb Y, et al. Perioperative use of β-blockers and COX-2 inhibitors may improve immune competence and reduce the risk of tumor metastasis. Ann Surg Oncol. 2008;15(7):2042–2052.
Shien T, Iwata H. Significance of primary lesion resection in stage IV breast cancer. Jpn J Clin Oncol. 2017;47(5):381–384.
Kakarala M, Wicha MS. Implications of the cancer stem-cell hypothesis for breast cancer prevention and therapy. J Clin Oncol. 2008;26(17):2813–2820.
Danna EA, Sinha P, Gilbert M, Clements VK, Pulaski BA, Ostrand-Rosenberg S. Surgical removal of primary tumor reverses tumor-induced immunosuppression despite the presence of metastatic disease. Cancer Res. 2004;64(6):2205–2211.
Kim M-Y, Oskarsson T, Acharyya S, et al. Tumor self-seeding by circulating cancer cells. Cell. 2009;139(7):1315–1326.
Norton L, Massagué J. Is cancer a disease of self-seeding? Nat Med. 2006;12(8):875–878.
Zambetti M, Montemurro F, Morandi P, et al. Safety profile of subcutaneous trastuzumab for the treatment of patients with HER2-positive early or locally advanced breast cancer: primary analysis of the SCHEARLY study. Eur J Cancer. 2018;105:61–70.
Thomas A, Khan SA, Chrischilles EA, Schroeder MC. Initial surgery and survival in stage IV breast cancer in the United States, 1988–2011. JAMA Surg. 2015.
Lane WO, Thomas SM, Blitzblau RC, et al. Surgical resection of the primary tumor in women with de novo stage IV breast cancer: contemporary practice patterns and survival analysis. Ann Surg. 2019;269(3):537–544.
King TA, Lyman J, Gonen M, et al. A prospective analysis of surgery and survival in stage IV breast cancer (TBCRC 013). J Clin Oncol. 2016;34(15_suppl):1006–1006.
National Institutes of Health Clinical Trials. A randomized phase III trial of the value of early local therapy for the intact primary tumor in patients with metastatic breast cancer. https://clinicaltrials.gov/ct2/show/NCT01242800?term=NCT01242800&rank=1. Accessed 1 Apr 2019.
UMIN Clinical Trials Registry. A randomized controlled trial comparing primary tumor resection plus systemic therapy with systemic therapy alone in metastatic breast cancer (JCOG1017, PRIM-BC). https://upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000006333. Accessed 1 Apr 2019.
Neuman HB, Morrogh M, Gonen M, Van Zee KJ, Morrow M, King TA. Stage IV breast cancer in the era of targeted therapy. Cancer. 2010;116(5):1226–1233.
Pons-Tostivint E, Kirova Y, Lusque A, et al. Survival impact of locoregional treatment of the primary tumor in de novo metastatic breast cancers in a large multicentric cohort study: a propensity score-matched analysis. Ann Surg Oncol. 2019;26(2):356–365.
Harano K, Lei X, Gonzalez-Angulo AM, et al. Clinicopathological and surgical factors associated with long-term survival in patients with HER2-positive metastatic breast cancer. Breast Cancer Res Treat. 2016;159(2):367–374.
Imkampe A, Bendall S, Bates T. The significance of the site of recurrence to subsequent breast cancer survival. Eur J Surg Oncol (EJSO). 2007;33(4):420–423.
American College of Surgeons. Radiation therapy. http://ncdbpuf.facs.org/content/radiation-therapy. Accessed 1 Nov 2018.
Sogaard M, W. Thomsen R, Bossen, Henrik Toft Sørensen H, Nørgaard M. The impact of comorbidity on cancer survival: a review. Clin Epidemiol. 2013:3.
Rugo HS, Brufsky AM, Yood MU, et al. Racial disparities in treatment patterns and clinical outcomes in patients with HER2-positive metastatic breast cancer. Breast Cancer Res Treat. 2013;141(3):461–470.
Newman LA. Breast cancer in African-American women. Oncol. 2005;10(1):1–14.
Ren J-X, Gong Y, Ling H, Hu X, Shao Z-M. Racial/ethnic differences in the outcomes of patients with metastatic breast cancer: contributions of demographic, socioeconomic, tumor and metastatic characteristics. Breast Cancer Res Treat. 2019;173(1):225–237.
Vaz-Luis I, Lin NU, Keating NL, et al. Racial differences in outcomes for patients with metastatic breast cancer by disease subtype. Breast Cancer Res Treat. 2015;151(3):697–707.
Cardoso F, Harbeck N, Fallowfield L, Kyriakides S, Senkus E. Locally recurrent or metastatic breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(suppl 7):vii11-vii19.
National Comprehensive Cancer Network. Breast cancer (Version 2010). Accessed 1 Apr 2019.
Howie LJ, Scher NS, Amiri-Kordestani L, et al. FDA approval summary: pertuzumab for adjuvant treatment of HER2-positive early breast cancer. Clin Cancer Res. 2019;25(10):2949–2955.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The NCDB is a joint project of the Commission on Cancer of the American College of Surgeons and the American Cancer Society and the data used in the study are derived from a de-identified NCDB file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed, or the conclusions drawn from these data.
Disclosures
The authors have no disclosures. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mudgway, R., Chavez de Paz Villanueva, C., Lin, A.C. et al. The Impact of Primary Tumor Surgery on Survival in HER2 Positive Stage IV Breast Cancer Patients in the Current Era of Targeted Therapy. Ann Surg Oncol 27, 2711–2720 (2020). https://doi.org/10.1245/s10434-020-08310-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08310-2