Abstract
Background
Surgical resection is associated with the best long-term results for intrahepatic cholangiocarcinoma (ICC); however, long-term outcomes are still poor.
Objective
The primary aim of this study was to validate the recently proposed MEGNA score and to identify additional prognostic factors influencing short- and long-term survival.
Patients and Methods
This was a retrospective analysis of a German multicenter cohort operated at 10 tertiary centers from 2004 to 2013. Patients were clustered using the MEGNA score and overall survival was analyzed. Cox regression analysis was used to identify prognostic factors for both overall and 90-day survival.
Results
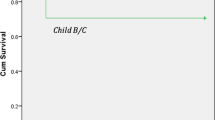
A total of 488 patients undergoing liver resection for ICC fulfilled the inclusion criteria and underwent analysis. Median age was 67 years, 72.5% of patients underwent major hepatic resection, and the lymphadenectomy rate was 86.9%. Median overall survival was 32.2 months. The MEGNA score significantly discriminated the long-term overall survival: 0 (68%), I (48%), II (32%), and III (19%) [p <0.001]. In addition, anemia was an independent prognostic factor for overall survival (hazard ratio 1.78, 95% confidence interval 1.29–2.45; p <0.01).
Conclusion
Hepatic resection provides the best long-term survival in all risk groups (19–65% overall survival). The MEGNA score is a good discriminator using histopathologic items and age for stratification. Correction of anemia should be attempted in every patient who responds to treatment. Perioperative liver failure remains a clinical challenge and contributes to a relevant number of perioperative deaths.


Similar content being viewed by others
References
Statistisches Bundesamt. Krankenhausstatistik-Diagnosedaten der Patienten und Patientinnen in Krankenhäusern, Statistisches Bundesamt.
Filmann N, Walter D, Schadde E, et al. Mortality after liver surgery in Germany. Br J Surg. 2019;106(11):1523–9.
Raoof M, Dumitra S, Ituarte PHG, et al. Development and validation of a prognostic score for intrahepatic cholangiocarcinoma. JAMA Surg. 2017;152:e170117.
Khan SA, Davidson BR, Goldin RD, et al. Guidelines for the diagnosis and treatment of cholangiocarcinoma: an update. Gut. 2012;61:1657–69.
Zhang X-F, Chakedis J, Bagante F, et al. Trends in use of lymphadenectomy in surgery with curative intent for intrahepatic cholangiocarcinoma. Br J Surg. 2018;105:857–66.
Bridgewater J, Galle PR, Khan SA, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60:1268–89.
Belgihiti J, Clavien PA, Gadzijev E, et al. The Brisbane 2000 terminology of liver anatomy and resections. HPB (Oxford). 2000;2:333–9.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149:713–24.
Koch M, Garden OJ, Padbury R, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680–8.
Rahbari NN, Garden OJ, Padbury R, et al. Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB (Oxford). 2011;13:528–35.
Chawla LS, Amdur RL, Amodeo S, et al. The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int. 2011;79:1361–9.
Keding V, Zacharowski K, Bechstein WO, et al. Patient Blood Management improves outcome in oncologic surgery. World J Surg Oncol. 2018;16:159.
Meybohm P, Fischer DP, Geisen C, et al. Safety and effectiveness of a Patient Blood Management (PBM) program in surgical patients: the study design for a multi-centre prospective epidemiologic non-inferiority trial. BMC Health Serv Res. 2014;14:576.
Meybohm P, Herrmann E, Steinbicker AU, et al. Patient blood management is associated with a substantial reduction of red blood cell utilization and safe for patient’s outcome: a prospective, Multicenter cohort study with a noninferiority design. Ann Surg. 2016;264:203–11.
Kim Y, Moris DP, Zhang X-F, et al. Evaluation of the 8th edition American Joint Commission on Cancer (AJCC) staging system for patients with intrahepatic cholangiocarcinoma: a Surveillance, Epidemiology, and End Results (SEER) analysis. J Surg Oncol. 2017;116:643–50.
Spolverato G, Kim Y, Alexandrescu S, et al. Is hepatic resection for large or multifocal intrahepatic cholangiocarcinoma justified? Results from a Multi-Institutional Collaboration. Ann Surg Oncol. 2015;22:2218–25.
Hyder O, Marques H, Pulitano C, et al. A nomogram to predict long-term survival after resection for intrahepatic cholangiocarcinoma: an Eastern and Western experience. JAMA Surg. 2014;149:432–8.
Ray S, Mehta NN, Golhar A, et al. Post hepatectomy liver failure—a comprehensive review of current concepts and controversies. Ann Med Surg. 2018;34:4–10.
Mueller MM, Van Remoortel H, Meybohm P, et al. Patient blood management: recommendations from the 2018 Frankfurt Consensus Conference. JAMA. 2019;321:983–97.
Hildebrand T, Pannicke N, Dechene A, et al. Biliary strictures and recurrence after liver transplantation for primary sclerosing cholangitis: a retrospective multicenter analysis. Liver Transplant. 2016;22:42–52.
Krawczyk M, Grąt M, Adam R, et al. Liver transplantation for hepatic trauma: a study from the European Liver Transplant Registry. Transplantation. 2016;100:2372–81.
Guise J-M, Savitz LA, Friedman CP. Mind the gap: putting evidence into practice in the era of learning health systems. J Gen Intern Med. 2018;33:2237–9.
Lamarca A, Ross P, Wasan HS, et al. Advanced intrahepatic cholangiocarcinoma: post hoc analysis of the ABC-01, -02 and -03 clinical trials. J Natl Cancer Inst. Epub 11 May 2019. https://doi.org/10.1093/jnci/djz071.
Funding
No funding was received for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Andreas A. Schnitzbauer, Johannes Eberhard, Fabian Bartsch, Stefan M. Brunner, Güralp O. Ceyhan, Dirk Walter, Helmut Fries, Sabine Hannes, Andreas Hecker, Jun Li, Karl Oldhafer, Nuh Rahbari, Falk Rauchfuss, Hans J. Schlitt, Utz Settmacher, Gregor Stavrou, Jürgen Weitz, Hauke Lang, Wolf O. Bechstein and Felix Rückert declare they have no conflict of interests.
Approval
The Institutional Review Board of the Medical Faculty Mannheim of the University of Heidelberg provided approval for this project in April 2016 (2016-816R-MA).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schnitzbauer, A.A., Eberhard, J., Bartsch, F. et al. The MEGNA Score and Preoperative Anemia are Major Prognostic Factors After Resection in the German Intrahepatic Cholangiocarcinoma Cohort. Ann Surg Oncol 27, 1147–1155 (2020). https://doi.org/10.1245/s10434-019-07968-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07968-7