Abstract
Background
The magnitude of the postoperative systemic inflammatory response (SIR), as evidenced by C-reactive protein (CRP), is associated with both short- and long-term outcomes following surgery for colorectal cancer. The present study examined the impact of preoperative dexamethasone on the postoperative SIR and complications following elective surgery for colorectal cancer.
Methods
Patients who underwent elective surgery, with curative intent, for colorectal cancer at a single center between 2008 and 2016 were included (n = 556) in this study. Data on the use of preoperative dexamethasone were obtained from anesthetic records, and its impact on CRP on postoperative days (PODs) 3 and 4, as well as postoperative complications, was assessed using propensity score matching (n = 276).
Results
In the propensity score-matched cohort, preoperative dexamethasone was associated with fewer patients exceeding the established CRP threshold of 150 mg/L on POD 3 (odds ratio [OR] 0.42, 95% confidence interval [CI] 0.26–0.70, p < 0.001) and fewer postoperative complications (OR 0.53, 95% CI 0.33–0.86, p = 0.009). Similar results for both POD 3 CRP and complications were observed when using propensity score-adjusted regression (OR 0.40, 95% CI 0.28–0.57 and OR 0.57, 95% CI 0.41–0.80, respectively) and propensity score stratification (OR 0.41, 95% CI 0.25–0.57 and OR 0.53, 95% CI 0.33–0.86, respectively).
Conclusions
Preoperative dexamethasone was associated with a lower postoperative SIR and fewer complications following elective surgery for colorectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Colorectal cancer is a leading cause of mortality in the developed world.1 Surgical resection continues to form the cornerstone of its management but is itself associated with significant morbidity and mortality.2 Long-term outcome is primarily related to disease stage at presentation, however it is increasingly understood that postoperative complications have a negative impact on oncologic outcome.3,4 In addition, postoperative complications are associated with a significant healthcare and societal cost.
Interleukin (IL)-6 and the more routinely available C-reactive protein (CRP), measured in the postoperative period, have been reported to be reliable markers of the magnitude of the surgical trauma.5 Furthermore, an association between the magnitude of this postoperative systemic inflammatory response (SIR) and the development of postoperative infective complications has been reported following surgery for colorectal cancer6–8 independent of presentation,9 and surgical approach.10 In addition, postoperative CRP and the threshold concentrations established to predict the development of infective complications have been reported to be associated with complication severity.11,12 More recently, a comprehensive systematic review suggested that CRP concentrations >150 mg/L on postoperative days (PODs) 3–5 should prompt investigation of potential postoperative complications such as anastomotic leak.13
There is good evidence that, compared with open surgery, laparoscopic surgery is associated with a reduction in the postoperative SIR.5 However, no definite causal relationship has yet been defined between attenuation of the postoperative SIR and postoperative complications. Furthermore, it remains to be seen whether strategies that attenuate the postoperative SIR may also reduce postoperative complication rates.
Corticosteroids, administered at the induction of anesthesia, are associated with the prevention of postoperative nausea and vomiting.14 Indeed, preoperative dexamethasone has now been integrated into many ‘enhanced recovery’ and ‘fast track’ perioperative care protocols, although the underlying mechanism remains unclear.15 Furthermore, there is evidence that preoperative administration of corticosteroids is associated with a reduction in the postoperative SIR following abdominal surgery.16,17
The aim of the present study was to examine the impact of preoperative dexamethasone on the magnitude of the postoperative SIR and complications following surgery for colorectal cancer. A propensity score analysis was performed due to significant imbalances in patient and operative variables potentially associated with both the postoperative SIR and complications.
Patients and Methods
Patients
This retrospective observational study of a prospectively collected database included patients who underwent resection with curative intent for histologically confirmed colorectal cancer in a single center between 2008 and 2016. Patients without available anesthetic records, receiving long-term corticosteroids, and who had existing inflammatory conditions, emergency surgery, or metastatic disease were not included in the analysis.
Clinical, radiological, and pathological data of all patients were reviewed by a specialist colorectal oncology multidisciplinary team before and after surgery. All patients received prophylactic antibiotics and venous thromboprophylaxis prior to the induction of anesthesia as per hospital policy. Furthermore, all patients were cared for in line with a unit standardized perioperative care policy that included early postoperative mobilization, early enteral nutrition, and the avoidance of routine nasogastric or peritoneal drainage. The use of epidural anesthesia was at the discretion of the anesthetic and surgical teams. Patients were administered dexamethasone intravenously prior to the induction of anesthesia, and at the discretion of the anesthetist, to reduce the likelihood of postoperative nausea and vomiting.
On each POD patients were clinically assessed and had blood samples, including serum CRP, obtained as standard until discharged. Further postoperative investigation and intervention was at the discretion of the patient’s surgical team who were not blind to serum CRP results.
Methods
Clinicopathological data were collected prospectively in a database, anonymized, and subsequently analyzed. Recorded information included patient demographics, tumor site, TNM stage (TNM, 5th edition, American Joint Committeee on Cancer), surgical approach, complications, and preoperative and postoperative serum CRP measurements.
Serum concentrations of CRP (mg/L) were measured using an autoanalyzer (Architect; Abbot Diagnostics, Maidenhead, UK) with a lower detectable limit of 0.2 mg/L, as was serum albumin (normal range 35–50 g/L). Exceeding the established CRP threshold of 150 mg/L on PODs 3 or 4 was recorded.13 The preoperative modified Glasgow Prognostic Score (mGPS) was calculated in patients for whom preoperative serum CRP and albumin were available.18
Data regarding the use of dexamethasone for the prevention of postoperative nausea and vomiting at the induction of anesthesia, the use of epidural anesthesia, and the need for intraoperative blood transfusion were collected by retrospective review of anesthetic notes.
Complications were recorded and categorized by severity using the Clavien–Dindo scale.19 Infective complications were categorized as described elsewhere and briefly summarized here.6 Wound (superficial surgical site) infection was defined as the presence of pus either spontaneously discharging from the wound or requiring drainage; deep surgical site infection was defined as surgical or image-guided drainage of intra-abdominal pus; anastomotic leak was defined as radiologically verified fistula to bowel anastomosis or diagnosed at laparotomy; pneumonia was defined by fever above 38.5 °C and consolidatory chest X-ray findings requiring antibiotic treatment; and septicemia was defined by the presence of sepsis combined with positive blood culture. Urinary tract infection was only included if complicated by septicemia and confirmed with positive urine culture.
This study was approved by the West of Scotland Research Ethics Committee, Glasgow, as part of a surgical audit.
Statistical Analysis
In the initial unmatched cohort, categorical data were compared using the χ 2 test. Data regarding postoperative CRP were non-normal and are presented as medians and ranges, and the medians of the two groups were compared using the Mann–Whitney U test. The treatment effect of preoperative dexamethasone in terms of exceeding the postoperative CRP threshold and complications was displayed as odds ratios (ORs) and 95% confidence intervals (CIs), while the magnitude of CRP by each POD was displayed graphically as 95% CIs of the median.
Multivariate logistic regression was used to generate a propensity score for each patient, predicting the probability of having received preoperative dexamethasone or not, based on the following variables thought to be associated with the postoperative SIR or complications: age, sex, body mass index (BMI), smoking status, American Society of Anesthesiologists (ASA) score, mGPS, tumor site, TNM stage, neoadjuvant chemoradiotherapy, surgical approach (open or laparoscopic), operation duration, blood transfusion, stoma formation, and the use of epidural anesthesia. Patients who received preoperative dexamethasone were then matched 1:1 with a patient who did not, using the closest propensity score on the logit scale (calliper < 0.05, order of match selection randomized, without replacement). Categorical data were compared using McNemar’s test, and continuous data were compared using the related samples Wilcoxon sign-rank test. The appropriateness of the propensity score matching was assessed visually by frequency of propensity scores in each group before and after matching. In addition, the propensity scores were included as a linear covariate alongside preoperative dexamethasone in multivariate binary logistic regression models for exceeding the POD 3 CRP threshold and postoperative complications. Finally, the propensity scores were used to stratify the patients by quintiles, from which an average treatment effect was calculated for both the POD 3 CRP threshold and postoperative complications as an OR and 95% CI.
In all tests, a two-sided p value <0.05 was considered statistically significant. Propensity scoring and matching, as well as all statistical analyses, were performed using IBM SPSS version 21 for Windows (IBM Corporation, Armonk, NY, USA).
Results
Patient Characteristics
Overall, 556 patients were included in the study (Table 1), of whom 310 were male (56%) and 360 (65%) were over 65 years of age. Most had colonic (355, 64%) and node-negative disease (375, 67%). Laparoscopic resection was performed in 212 patients (38%), with the remainder having open surgery. A postoperative complication occurred in 234 cases (42%), of which 151 (27%) were infective and 47 (8%) were classified as Clavien–Dindo grade 3–5 severity. Anastomotic leak occurred in 19 cases (3%), and there were 5 (1%) postoperative deaths.
Impact of Dexamethasone on All Patients
In the unmatched cohort, exceeding the CRP threshold of 150 mg/L on POD 3 was significantly associated with higher rates of any complication (60 vs. 29%, OR 3.60, p < 0.001), infective complications (42 vs. 16%, OR 3.87, p < 0.001), anastomotic leak (6 vs. 1%, OR 4.16, p = 0.011), and Clavien–Dindo grade 3 or higher complications (13 vs. 5%, OR 3.10, p = 0.001). In the unmatched cohort (Table 1), 311 patients (56%) received dexamethasone at the induction of anesthesia, of whom 194 received 4 mg and 117 received 8 mg, while 245 (44%) did not. There were significant differences between those patients who received preoperative dexamethasone and those who did not, in ASA grade (p = 0.003), preoperative mGPS (p = 0.007), laparoscopic surgery (52 vs. 20%, p < 0.001), surgery lasting more than 4 h (41 vs. 23%, p < 0.001), blood transfusion (3 vs. 9%, p = 0.002), and epidural anesthesia (28 vs. 64%, p < 0.001). A significantly lower proportion of those who received preoperative dexamethasone exceeded the established CRP threshold of 150 mg/L on POD 3 (33 vs. 55%, p < 0.001), but not on day 4. Preoperative dexamethasone was significantly associated with fewer postoperative complications (36 vs. 50%, OR 0.40, p = 0.001) and infective complications (23 vs. 32%, OR 0.57, p = 0.021), but not anastomotic leak or complication severity.
Impact of Dexamethasone on the Propensity Score-Matched Cohort
Propensity scores could not be assigned to 156 patients due to missing covariate data, leaving 400 patients with propensity scores, of whom 262 had received dexamethasone at the induction of anesthesia and 138 had not (Fig. 1). Overall, 276 patients (138 from each group) were matched based on their propensity score, with a subsequent improvement in the balance of the distribution of propensity scores in each group (Fig. 2).
In the propensity score-matched cohort, exceeding the CRP threshold of 150 mg/L on POD 3 was significantly associated with higher rates of any complication (59 vs. 28%, OR 3.58, p < 0.001), infective complications (44 vs. 15%, OR 4.38, p < 0.001), and Clavien–Dindo grade 3 or higher complications (13 vs. 6%, OR 2.56, p = 0.032), but not anastomotic leak (7 vs. 2%, OR 3.29, p = 0.068). Following propensity score matching, the distribution of patient and operative variables was balanced between the two groups (Table 2). A significantly lower proportion of those who received preoperative dexamethasone exceeded the established CRP threshold of 150 mg/L on POD 3 (36 vs. 56%, OR 0.42, p = 0.001), but not on day 4. Preoperative dexamethasone was significantly associated with fewer postoperative complications (34 vs. 49%, OR 0.53, p = 0.001).
Other Propensity Score Analyses
Analysis of the impact of preoperative dexamethasone on exceeding the POD 3 CRP threshold (Table 3) found a similarly statistically significant probability reduction using regression adjustment (OR 0.53, 95% CI 0.34–0.83), propensity score stratification (OR 0.41, 95% 0.25–0.57), and propensity score matching (0.42, 95% CI 0.26–0.70). The same analysis of the impact of preoperative dexamethasone on postoperative complications (Table 3) found a similarly statistically significant probability reduction using regression adjustment (OR 0.62, 95% CI 0.40–0.96), propensity score stratification (OR 0.62, 95% 0.29–0.95), and propensity score matching (0.53, 95% CI 0.33–0.86).
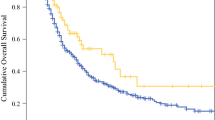
Time-Dependent Effect of Preoperative Dexamethasone
Dexamethasone at the induction of anesthesia had a similar time-dependent effect on postoperative CRP in both the unmatched and matched cohorts. There was a significant reduction in CRP on PODs 1–3, with similar concentrations from POD 4 onward.
Discussion
The present study reports that dexamethasone, administered at the induction of anesthesia, prior to surgery for colorectal cancer was associated with a reduction in the magnitude of the postoperative SIR and fewer postoperative complications.
Currently, corticosteroids are administered in the perioperative period to reduce postoperative nausea and vomiting.14,15 However, when taken together with existing evidence,16,17,20 the results of the present study also suggest an important role for reducing the complication rate following surgery for colorectal cancer by attenuating the postoperative stress response. Indeed, the use of preoperative corticosteroids represents a potentially simple and cost-effective method of improving surgical outcomes for a large surgical population. It was of interest that postoperative CRP retained its association with postoperative complications in those patients who had received preoperative dexamethasone. In particular, the CRP threshold of 150 mg/L on POD 3 remained significantly associated with all and infective complications in this group of patients in whom the magnitude of the postoperative SIR was lower as a whole.21 Indeed, the results of the present study suggest that the measurement of postoperative CRP in this subgroup remains useful in the clinical setting. For these reasons, the present study in colorectal cancer is timely.
There remain long-standing concerns that corticosteroids may inhibit collagen formation, and therefore wound healing, in the postoperative period. However, neither the present study nor previous meta-analyses have identified a significant negative association with either wound complications or anastomotic leak14,15 Furthermore, there have been some concerns that preoperative corticosteroids may have a negative impact on oncologic outcome following surgery for colorectal cancer; however, the evidence for this is limited in both numbers and length of follow-up.22
The mechanisms by which corticosteroids exert their anti-inflammatory action remain poorly understood. Inhibition of nuclear factor κB (NF-κB) leads to a downregulatory effect on lymphoid tissue and thus adaptive immune responses.23 In addition, attenuation of the innate immune response and myeloid tissues occurs as a consequence of reduction of the transcription of proinflammatory cytokines such as IL-6, alongside the inhibition of cyclooxygenase-dependent pathways by increasing the transcription of lipocortins.15,24,25
An important implication of the present and previous results is that postoperative complications are themselves recognized to have a negative impact on oncologic outcomes.26 Indeed, the generation of a prometastatic environment through systemic inflammation, as part of the surgical injury and the severity of postoperative complications, has been proposed to promote metastatic disease progression.27 Furthermore, it has been proposed that this host response to both the tumor and surgery should become a target for intervention.28 Indeed, it may be hypothesized that a reduction in the magnitude of the postoperative SIR, with a consequent reduction in postoperative complication rates, may improve long-term outcomes following surgery for colorectal cancer. Strategies such as the prospective evaluation of perioperative corticosteroids represent a logical starting point.
The main limitation of the present study was its retrospective nature. Significant imbalance between the two groups meant that propensity score matching was used to obtain balanced groups for determination of the treatment effect; however, this resulted in the exclusion of a significant proportion of patients, and does not necessarily help those confounders that are either unmeasured or unknown.29 Nonetheless, it was reassuring that the overall treatment effect and its magnitude were similar among the unmatched cohort, the matched cohort, and when propensity regression was applied.30 In addition, the nature of the analysis prevented the assessment of any dose–response relationship.
Conclusions
The results of the present study suggest that the use of preoperative corticosteroids is associated with both attenuation of the magnitude of the SIR and fewer complications following surgery for colorectal cancer. This would suggest that the magnitude of the postoperative SIR and postoperative complications are causally related. Optimal doses and treatment regimens are yet to be determined. Indeed, further prospective randomized trials are necessary before recommendations regarding the use of preoperative dexamethasone in the context of the postoperative SIR can be made.
References
Cancer Research UK. Cancer statistics. http://www.cancerresearchuk.org/cancer-info/cancerstats/incidence/commoncancers/(2004)
Ghaferi LG, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49:1076–81
Mirnezami A, Mirneznami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg. 2011;253(5):890–99
Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, Berger DH. Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer. Ann Surg. 2015;261(3):497–05
Watt DG, Horgan PG, McMillan DC. Routine clinical markers of the magnitude of the systemic inflammatory response after elective operation: a systematic review. Surgery. 2015;157(2):362–80
Platt JJ, Ramanathan ML, Crosbie RA, Anderson JH, McKee RF, Horgan PG, et al. C-reactive protein as a predictor of postoperative infective complications after curative resection in patients with colorectal cancer. Ann Surg Oncol. 2012;19:4168–77
Singh PP, Zeng ISL, Srinivasa S, Lemanu DP, Connolly AB, Hill AG. Systematic review and meta-analysis of use of serum C-reactive protein levels to predict anastomotic leak after colorectal surgery. Br J Surg. 2014;101:339–46
Adamina M, Steffen T, Tarantino I, Beutner U, Schmied BM, Warschkow R. Meta-analysis of the predictive value of C-reactive protein for infectious complications in abdominal surgery. Br J Surg. 2015;102:590–98
Straatman J, de Weerdesteijn EW, Tuynman JB, Cuesta MA, van der Peet DL. C-reactive protein as a marker for postoperative complications. Are there differences in emergency and elective colorectal surgery? Dis Colon Rectum. 2016;59(1):35–41
Ramanathan ML, MacKay G, Platt J, Horgan PG, McMillan DC. The impact of open versus laparoscopic resection for colon cancer on c-reactive protein concentrations as a predictor of postoperative infective complications. Ann Surg Oncol. 2015;22(3):938–43
Selby J, Prabhudesai A. Can C-reactive protein predict the severity of a post-operative complication after elective resection of colorectal cancer. Int J Colorectal Dis. 2014;29(10):1211–15.
McSorley ST, Ramanathan ML, Horgan PG, McMillan DC. Postoperative C-reactive protein measurement predicts the severity of complications following surgery for colorectal cancer. Int J Colorectal Dis. 2015;30(7):913–17
McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal cancer. Br J Surg. 2015;102:462–79
Karanicolas PJ, Smith SE, Kanbur B, Davies E, Guyatt GH. The impact of prophylactic dexamethasone on nausea and vomiting after laparoscopic cholecystectomy: a systematic review and meta-analysis. Ann Surg. 2008;248(5):751–62
Watt DG, McSorley ST, Horgan PG, McMillan DC. Enhanced recovery after surgery: which components, if any, impact on the systemic inflammatory response following surgery for colorectal surgery? A systematic review. Medicine. 2015;94(36):e1286
Srinivasa S, Kahoker AA, Yu TC, Hill AG. Preoperative glucocorticoid use in major abdominal surgery: systematic review and meta-analysis of randomized trials. Ann Surg. 2011;254(2):183–91
McSorley ST, Horgan PG, McMillan DC. The impact of preoperative corticosteroids on the systemic inflammatory response and postoperative complications following surgery for gastrointestinal cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2016;101:139–50
McMillan DC. The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev. 2012;36(5):534–40
Dindo D, Demartines N, Clavien P. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13
Laaninen M, Sand J, Nordback I, Vasama K, Laukkarinen J. Perioperative hydrocortisone reduces major complications after pancreaticoduodenectomy: a randomized controlled trial. Ann Surg. 2016;264(5):696–02
McSorley ST, Watt DG, Horgan PG, McMillan DC. Postoperative systemic inflammatory response, complication severity, and survival following surgery for colorectal cancer. Ann Surg Oncol. 2016;23(9):2832–40
Singh PP, Lemanu DP, Taylor MH, Hill AG. Association between pre-operative glucocorticoids and long-term survival and cancer recurrence after colectomy: follow-up analysis of a previously randomized trial. Br J Anaesth. 2014;113(S1):i68–i73
Chu CC, Hsing CH, Shieh JP, Chien CC, Ho CM, Wang JJ. The cellular mechanisms of the antiemetic action of dexamethasone and related glucocorticoids against vomiting. Eur J Pharmacol. 2014;722:48–54
Rhen T, Cidlowski JA. Anti-inflammatory action of glucocorticoids: new mechanisms for old drugs. N Engl J Med. 2005;353:1711–23
Leung DYM, Bloom JW. Update on glucocorticoid action and resistance. J Allergy Clin Immunol. 2003;111(1):3–22
McSorley ST, Horgan PG, McMillan DC. The impact of the type and severity of postoperative complications on long-term outcomes following surgery for colorectal cancer: a systematic review and meta-analysis. Crit Rev Oncol Haematol. 2016;97:168–77
McAllister SS, Weinberg RA. The tumour induced systemic environment as a critical regulator of cancer progression and metastasis. Nat Cell Biol. 2014;16(8):717–27
Roxburgh CS, Horgan PG, McMillan DC. The perioperative immune/inflammatory insult in cancer surgery: time for intervention? Oncoimmunology. 2013;2:e27324
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–24
Shida D, Hamaguchi T, Ochiai H, Tsukamoto S, Takashima A, Boku N, et al. Prognostic impact of palliative primary tumor resection for unresectable stage 4 colorectal cancer: using a propensity score analysis. Ann Surg Oncol. 2016;23(11):3602–08
Acknowledgement
The authors acknowledge the support of the consultant surgeons of the colorectal unit of the Glasgow Royal Infirmary.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
McSorley, S.T., Roxburgh, C.S.D., Horgan, P.G. et al. The Impact of Preoperative Dexamethasone on the Magnitude of the Postoperative Systemic Inflammatory Response and Complications Following Surgery for Colorectal Cancer. Ann Surg Oncol 24, 2104–2112 (2017). https://doi.org/10.1245/s10434-017-5817-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5817-3