Abstract
Background
Intraoperative hypovolemic phlebotomy (HP) has been suggested to reduce central venous pressure (CVP) before hepatectomy. This study aimed to analyze the impact of CVP drop after HP on intraoperative blood loss and postoperative renal function.
Methods
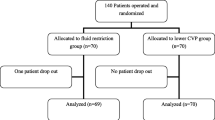
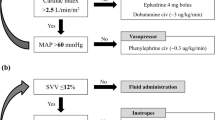
A retrospective review of a prospective database including 100 consecutive patients (43 males and 57 females; mean age, 65 years; range 23–89 years) undergoing liver resection with HP was performed. The primary outcome variable was estimated blood loss (EBL), and the secondary outcome was postoperative serum creatinin (Scr). A multivariate linear regression analysis was performed to identify predictors of intraoperative blood loss.
Results
The median CVP before blood salvage was 8 mmHg (range 4–30 mmHg). The median volume of hypovolemic phlebotomy was 400 ml (range 200–1000 ml). After HP, CVP decreased to a median of 3 mmHg (range –2 to 16 mmHg), resulting in a median CVP drop of 5.5 mmHg (range 2–14 mmHg). The median EBL during liver resection was 165 ml (range 0–800 ml). The median preoperative serum creatinin (Scr) was 0.82 g/dl (range 0.5–1.74 g/dl), and the postoperative Scr on day 1 was 0.74 g/dl (range 0.44–1.68 g/dl). The CVP drop was associated with EBL (P < 0.001). There was no significant impact of CVP drop on postoperative Scr.
Conclusion
A CVP drop after HP is a strong independent predictor of EBL during liver resection. The authors advocate the routine use of HP to reduce perioperative blood loss and transfusion rates in liver surgery. As a predictive tool, CVP drop might help surgeons decide whether a laparoscopic approach is safe.



Similar content being viewed by others
References
Alkozai EM, Lisman T, Porte RJ. Bleeding in liver surgery: prevention and treatment. Clin Liver Dis. 2009;13:145–54.
Schiergens TS, Rentsch M, Kasparek MS, Frenes K, Jauch K-W, Thasler WE. Impact of perioperative allogeneic red blood cell transfusion on recurrence and overall survival after resection of colorectal liver metastases. Dis Colon Rectum. 2015;58: 74–82.
Amato A, Pescatori M. Perioperative blood transfusions and recurrence of colorectal cancer. Cochrane Database Syst Rev. 2006. doi:10.1002/14651858.CD005033.pub2.
Kulaylat AN, Schubart JR, Stokes AL, Bhayani NH, Wong J, Kimchi ET, et al. Overall survival by pattern of recurrence following curative intent surgery for colorectal liver metastasis. J Surg Oncol. 2014;110:1011–5.
Kimura N, Toyoki Y, Ishido K, Kudo D, Yakoshi Y, Tsutsumi S, et al. Perioperative blood transfusion as a poor prognostic factor after aggressive surgical resection for hilar cholangiocarcinoma. J Gastrointest Surg. 2015;19: 866–79
Harada N, Shirabe K, Maeda T, Kayashima H, Ishida T, Maehara Y. Blood transfusion is associated with recurrence of hepatocellular carcinoma after hepatectomy in Child-Pugh class a patients. World J Surg. 2015;39:1044–51.
Kim JK, Kim HS, Park J, Jeong CW, Ku JH. Perioperative blood transfusion as a significant predictor of biochemical recurrence and survival after radical prostatectomy in patients with prostate cancer. PLoS ONE, 2016;11: 1–13
Acheson AG, Brookes MJ, Spahn DR. Effects of allogeneic red blood cell transfusions on clinical outcomes in patients undergoing colorectal cancer surgery: a systematic review and meta-analysis. Ann Surg. 2012;256:235–44.
Hallet J, Tsang M, Cheng ESW, Habashi R, Kulyk I, Hanna SS, et al. The impact of perioperative red blood cell transfusions on long-term outcomes after hepatectomy for colorectal liver metastases. Ann Surg Oncol. 2015;22: 4038–4045.
Liu L, Wang Z, Jiang S, Shao B, Liu J, Zhang S, et al. Perioperative allogenenic blood transfusion is associated with worse clinical outcomes for hepatocellular carcinoma: a meta-analysis. PLoS ONE. 2013;8: e64261
Matsumata T, Ikeda Y, Hayashi H, Kamakura T, Taketomi A, Sugimachi K. The association between transfusion and cancer-free survival after curative resection for hepatocellular carcinoma. Cancer. 1993;72:1866–71.
Lautt WW, Greenway CV. Hepatic venous compliance and role of liver as a blood reservoir. Am J Physiol. 1976;231:292–5.
Jones RM, Moulton CE, Hardy KJ. Central venous pressure and its effect on blood loss during liver resection. Br J Surg. 1998;85:1058–60.
Wang W-D, Liang L-J, Huang X-Q, Yin X-Y. Low central venous pressure reduces blood loss in hepatectomy. World J Gastroenterol. 2006;12:935–9.
Massicotte L, Sassine M-P, Lenis S, Roy A. Transfusion predictors in liver transplant. Anesth Analg. 2004;98:1245–51.
Li Z, Sun YM, Wu FX, Yang LQ, Lu ZJ, Yu WF. Controlled low central venous pressure reduces blood loss and transfusion requirements in hepatectomy. World J Gastroenterol. 2014;20:303–9.
Stéphan F, Rezaiguia-Delclaux S. Usefulness of a central venous catheter during hepatic surgery. Acta Anaesthesiol Scand. 2008;52:388–96.
Dunki-Jacobs EM, Philips P, Scoggins CR, McMasters KM, Martin RCG. Stroke volume variation in hepatic resection: a replacement for standard central venous pressure monitoring. Ann Surg Oncol. 2014;21:473–8.
Strasberg SM, Phillips C. Use and dissemination of the brisbane 2000 nomenclature of liver anatomy and resections. Ann Surg. 2013;257:377–82.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications. Ann Surg. 2004;240:205–13.
Valdivieso JR, Bes-Rastrollo M, Monedero P, De Irala J, Lavilla FJ. Evaluation of the prognostic value of the risk, injury, failure, loss and end-stage renal failure (RIFLE) criteria for acute kidney injury. Nephrology, 2008;13: 361–6
Herbert P, Wells G, Blajchman M, Marshall J, Martin C, Pagliarello G, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med, 1999;340:409–17.
Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1803 consecutive cases over the past decade. Ann Surg. 2002;236:397–407
Melendez JA, Arslan V, Fischer ME, Wuest D, Jarnagin WR, Fong Y, et al. Perioperative outcomes of major hepatic resections under low central venous pressure anesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg. 1998;187:620–5.
Kim YK, Chin JH, Kang SJ, Jun IG, Song JG, Jeong SM, et al. Association between central venous pressure and blood loss during hepatic resection in 984 living donors. Acta Anaesthesiol Scand. 2009;53:601–6.
Hashimoto T, Kokudo N, Orii R, Seyama Y, Sano K, Imamura H, et al. Intraoperative blood salvage during liver resection: a randomized controlled trial. Ann Surg. 2007;245:686–91.
Choi S-S, Cho S-S, Kim S-H, Jun I-G, Hwang G-S, Kim Y-K. Factors associated with blood transfusion in donor hepatectomy. Transpl J. 2013;96:1000–7.
Correa-Gallego C, Berman A, Denis SC, Langdon-Embry L, O’Connor D, Arslan-Carlon V, et al. Renal function after low central venous pressure-assisted liver resection: assessment of 2116 cases. HPB. 2015;17:258–64.
Mbah NA, Brown RE, Bower MR, Scoggins CR, McMasters KM, Martin RCG. Differences between bipolar compression and ultrasonic devices for parenchymal transection during laparoscopic liver resection. HPB. 2012;14:126–31.
Otsuka Y, Kaneko H, Cleary SP, Buell JF, Cai X, Wakabayashi G. What is the best technique in parenchymal transection in laparoscopic liver resection? Comprehensive review for the clinical question on the 2nd International Consensus Conference on Laparoscopic Liver Resection. J Hepatobiliary Pancreat Sci, 2015;22:363–70.
Giordano C, Deitte LA, Gravenstein N, Rice MJ. What is the preferred central venous pressure zero reference for hepatic resection? Anesth Analg. 2010;111:660–4.
Schroeder RA, Collins BH, Tuttle-Newhall E, Robertson K, Plotkin J, Johnson LB, et al. Intraoperative fluid management during orthotopic liver transplantation. J Cardiothorac Vasc Anesth. 2004;18:438–41.
Feng ZY, Xu X, Zhu SM, Bein B, Zheng S Sen. Effects of low central venous pressure during preanhepatic phase on blood loss and liver and renal function in liver transplantation. World J Surg. 2010;34:1864–73.
Kim WH, Park MH, Kim H-J, Lim H-Y, Shim HS, Sohn J-T, et al. Potentially modifiable risk factors for acute kidney injury after surgery on the thoracic aorta. Medicine Baltimore. 2015;94:e273–7.
Haase M, Bellomo R, Story D, Letis A, Klemz K, Matalanis G, et al. Effect of mean arterial pressure, haemoglobin, and blood transfusion during cardiopulmonary bypass on postoperative acute kidney injury. Nephrol Dial Transpl. 2012;27:153–60.
Wolters U, Wolf T, Stutzer H, Schroder T. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth. 1996;77:217–22.
DISCLOSURE
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ryckx, A., Christiaens, C., Clarysse, M. et al. Central Venous Pressure Drop After Hypovolemic Phlebotomy is a Strong Independent Predictor of Intraoperative Blood Loss During Liver Resection. Ann Surg Oncol 24, 1367–1375 (2017). https://doi.org/10.1245/s10434-016-5737-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5737-7