Abstract
Background
Although the low central venous pressure (LCVP) technique is used to decrease blood loss during liver resection, its efficacy and safety during transplant procedures are still debatable. Our study aimed to assess the effects of this technique and its clinical safety for recipients undergoing liver transplantation.
Methods
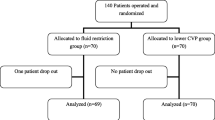
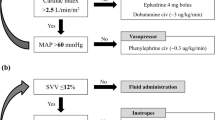
Eighty-six adult patients were randomly divided into a LCVP group and a control group. In the LCVP group, CVP was maintained below 5 mmHg or 40% lower than baseline during the preanhepatic phase by limiting infusion volume, manipulating the patient’s posture, and administration of somatostatin and nitroglycerine. Recipients in the control group received standard care. Hemodynamics, blood loss, liver function, and renal function of the two groups were compared perioperatively.
Results
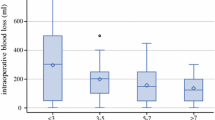
A lower CVP was maintained in the LCVP group during the preanhepatic phase, resulting in a significant decrease in blood loss (1922 ± 1429 vs. 3111 ± 1833 ml, P < 0.05) and transfusion volume (1200 ± 800 vs. 2400 ± 1200 ml, P < 0.05) intraoperatively. Compared with the control group, the LCVP group had a significantly lower mean arterial pressure at 2 h after the start of the operation (74 ± 11 vs. 84 ± 14 mmHg, P < 0.05), a lower lactate value at the end of the operation (5.9 ± 3.0 vs. 7.2 ± 3.0 mmol/l, P < 0.05), and a better preservation of liver function after the declamping of the portal vein. There were no significant differences in perioperative renal function and postoperative complications between the groups.
Conclusions
The LCVP technique during the preanhepatic phase reduced intraoperative blood loss, protected liver function, and had no detrimental effects on renal function in LT.



Similar content being viewed by others
Abbreviations
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate transaminase
- BUN:
-
Blood urea nitrogen
- CR:
-
Creatinine
- CVP:
-
Central venous pressure
- DO2I:
-
Oxygen delivery index
- FFP:
-
Fresh frozen plasma
- INR:
-
International normalized ratio
- LCVP:
-
Low central venous pressure
- LDLT:
-
Living donor liver transplantation
- LT:
-
Liver transplantation
- MAP:
-
Mean arterial pressure
- MELD:
-
Model for end-stage liver disease
- MODS:
-
Multiple-organ dysfunction syndromes
- PAWP:
-
Pulmonary arterial wedge pressure
- PT:
-
Prothrombin time
- PVP:
-
Portal vein pressure
- RBC:
-
Red blood cell
- TB:
-
Total bilirubin
- VO2I:
-
Oxygen consumption index
References
Lukanovic NP (2008) Topics in liver anaesthesia. Transplant Proc 40:1187–1189
Lopez-Plaza I (2007) Transfusion guidelines and liver transplantation: time for consensus. Liver Transpl 13:1630–1632
Yuasa T, Niwa N, Kimura S et al (2005) Intraoperative blood loss during living donor liver transplantation: an analysis of 635 recipients at a single center. Transfusion 45:879–884
Frasco PE, Poterack KA, Hentz JG et al (2005) A comparison of transfusion requirements between living donation and cadaveric donation liver transplantation: relationship to model of end-stage liver disease score and baseline coagulation status. Anesth Analg 101:30–37
Cacciarelli TV, Keeffe EB, Moore DH et al (1999) Effect of intraoperative blood transfusion on patient outcome in hepatic transplantation. Arch Surg 134:25–29
Massicotte L, Sassine MP, Lenis S et al (2005) Survival rate changes with transfusion of blood products during liver transplantation. Can J Anaesth 2:148–155
Ramos E, Dalmau A, Sabate A et al (2003) Intraoperative red blood cell transfusion in liver transplantation: influence on patient outcome, prediction of requirements, and measures to reduce them. Liver Transpl 9:1320–1327
Porte RJ, Molenaar IQ, Begliomini B et al (2000) Aprotinin and transfusion requirements in orthotropic liver transplantation: a multicentre randomised double-blind study. EMSALT Study Group. Lancet 355:1303–1309
Lentschener C, Roche K, Ozier Y (2005) A review of aprotinin in orthotropic liver transplantation: can its harmful effects offset its beneficial effects? Anesth Analg 100:1248–1255
Moreno-Gonzalez E, Meneu-Diaz JG, Fundora Y et al (2003) Advantages of the piggy back technique on intraoperative transfusion, fluid consumption, and vasoactive drug requirements in liver transplantation: a comparative study. Transplant Proc 35:1918–1919
Schroeder RA, Kuo PC (2008) Pro: low central venous pressure during liver transplantation—not too low. J Cardiothorac Vasc Anesth 22:311–314
Massicotte L, Lenis S, Thibeault L et al (2006) Effect of low central venous pressure and phlebotomy on blood product transfusion requirements during liver transplantations. Liver Transpl 12:117–123
Schroeder RA, Collins BH, Tuttle-Newhall E et al (2004) Intraoperative fluid management during orthotopic liver transplantation. J Cardiothorac Vasc Anesth 18:438–441
Mangus RS, Kinsella SB, Nobari MM et al (2007) Predictors of blood product use in orthotopic liver transplantation using the piggyback hepatectomy technique. Transplant Proc 39:3207–3213
Massicotte L, Beaulieu D, Thibeault L (2008) Con: low central venous pressure during liver transplantation. J Cardiothorac Vasc Anesth 22:315–317
Melendez JA, Arslan V, Fischer ME et al (1998) Perioperative outcomes of major hepatic resections under low central venous pressure anaesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg 187:620–625
Chen H, Merchant NB, Didolkar MS (2000) Hepatic resection using intermittent vascular inflow occlusion and low central venous pressure anaesthesia improves morbidity and mortality. J Gastrointest Surg 4:162–167
Chen CL, Chen YS, de Villa VH et al (2000) Minimal blood loss living donor hepatectomy. Transplantation 69:2580–2586
Smyrniotis V, Kostopanagiotou G, Theodoraki K et al (2004) The role of central venous pressure and type of vascular control in blood loss during major liver resections. Am J Surg 187:398–402
Wang WD, Liang LJ, Huang XQ et al (2006) Low central venous pressure reduces blood loss in hepatectomy. World J Gastroenterol 12:935–939
Ayanoglu HO, Ulukaya S, Yuzer Y et al (2003) Anesthetic management and complications in living donor hepatectomy. Transplant Proc 35:2970–2973
McCluskey SA, Karkouti K, Wijeysundera DN et al (2006) Derivation of a risk index for the prediction of massive blood transfusion in liver transplantation. Liver Transpl 12:1584–1593
Massicotte L, Sassine MP, Lenis S et al (2004) Transfusion predictors in liver transplant. Anesth Analg 98:1245–1251
Findlay JY, Rettke SR (2000) Poor prediction of blood transfusion requirements in adult liver transplantations from preoperative variables. J Clin Anesth 12:319–323
Steib A, Freys G, Lehmann C et al (2001) Intraoperative blood losses and transfusion requirements during adult liver transplantation remain difficult to predict. Can J Anaesth 48:1075–1079
Johnson M, Mannar R, Wu Av (1998) Correlation between blood loss and inferior vena caval pressure during liver resection. Br J Surg 85:188–190
Feng ZY, Jin XD, Chen YZ et al (2008) Predictors of massive blood transfusion in liver transplantation for patients with benign end-stage liver disease. Zhonghua Yi Xue Za Zhi 88:3040–3044
Jones RM, Moulton CE, Hardy KJ (1998) Central venous pressure and its effect on blood loss during liver resection. Br J Surg 85:1058–1060
Hashimoto T, Kokudo N, Orii R et al (2007) Intraoperative blood salvage during liver resection: a randomized controlled trial. Ann Surg 245:686–691
De Kock M, Laterre PF, Van Obbergh L et al (1998) The effects of intraoperative intravenous clonidine on fluid requirements, hemodynamic variables, and support during liver transplantation: a prospective, randomized study. Anesth Analg 86:468–476
Heise M, Settmacher U, Pfitzmann R et al (2003) A survival-based scoring system for initial graft functions following orthotopic liver transplantation. Transpl Int 16:794–800
Eisenbach C, Encke J, Merle U et al (2009) An early increase in gamma glutamyltranspeptidase and low aspartate aminotransferase peak values are associated with superior outcomes after orthotopic liver transplantation. Transplant Proc 41:1727–1730
Ito T, Kiuchi T, Yamamoto H et al (2003) Changes in portal venous pressure in the early phase after living donor liver transplantation: pathogenesis and clinical implications. Transplantation 75:1313–1317
Xu X, Man K, Zheng SS et al (2006) Attenuation of acute phase shear stress by somatostatin improves small-for-size liver graft survival. Liver Transpl 12:621–627
Landa I, Arias J, Gómez M et al (1992) Cytoprotective effect of somatostatin in a rat model of hepatic ischemic reperfusion. Hepatology 16:1474–1476
Nakata Y, Sato M, Watanabe Y et al (2000) Intraoperative fluid requirements during porcine liver transplantation. Transplant Proc 32:2338–2339
Lebrón Gallardo M, Herrera Gutierrez ME, Seller Pérez G et al (2004) Risk factors for renal dysfunction in the postoperative course of liver transplant. Liver Transpl 10:1379–1385
Soonawalla ZF, Stratopoulos C, Stoneham M et al (2008) Role of the reverse-Trendelenberg patient position in maintaining low-CVP anaesthesia during liver resections. Langenbecks Arch Surg 393:195–198
Hatano Y, Murakawa M, Segawa H et al (1990) Venous air embolism during hepatic resection. Anesthesiology 73:1282–1285
Cirera I, Feu F, Luca A et al (1995) Effects of bolus injections and continuous infusions of somatostatin and placebo in patients with cirrhosis: a double-blind hemodynamic investigation. Hepatology 22:106–111
Bosch J, Kravetz D, Rodes J (1981) Effects of somatostatin on hepatic and systemic hemodynamics in patients with cirrhosis of the liver: comparison with vasopressin. Gastroenterology 80:518–525
Acknowledgments
This study was supported by grants from the National Science and Technology (S & T) major project, China (2008ZX10002-026), and the Science and Technology Bureau of Zhejiang Province, China (2009C33091).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feng, ZY., Xu, X., Zhu, SM. et al. Effects of Low Central Venous Pressure During Preanhepatic Phase on Blood Loss and Liver and Renal Function in Liver Transplantation. World J Surg 34, 1864–1873 (2010). https://doi.org/10.1007/s00268-010-0544-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0544-y