Abstract
Background
Most studies have failed to identify any prognostic value of the current T-stage protocol for pancreatic ductal adenocarcinoma (PDAC) by the American Joint Committee on Cancer and the Union for International Cancer Control unless some grouping was performed.
Methods
To document the parameters included in this T-stage protocol, 223 consecutive pancreatoduodenectomy specimens with PDAC were processed by a uniform grossing protocol.
Results
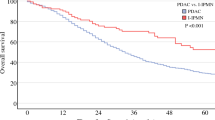
Peripancreatic soft tissue (PST) involvement, the main pT3 parameter, was found to be inapplicable and irreproducible due to lack of a true capsule in the pancreas and variability in the amount and distribution of adipose tissue. Furthermore, 91 % of the cases showed carcinoma in the adipose tissue, presumably representing the PST, and thus were classified as pT3. An additional 4.5 % were qualified as pT3 due to extension into adjacent sites. The T-stage defined as such was not found to have any correlation with survival (p = 0.4). A revised T-stage protocol was devised that defined pT1 as 2 cm or smaller, pT2 as >2–4 cm, and pT3 as larger than 4 cm. This revised protocol was tested in 757 consecutive PDACs. The median and 3-year survival rates of this size-based protocol were 26, 18, 13 months, and 40 %, 26 %, 20 %, respectively (p < 0.0001). The association between higher T-stage and shorter survival persisted in N0 cases and in multivariate modeling. Analysis of the Surveillance, Epidemiology, and End Results database also confirmed the survival differences (p < 0.0001).
Conclusions
This study showed that resected PDACs are already spread to various surfaces of the pancreas, leaving only about 4 % of PDACs to truly qualify as pT1/T2, and that the current T-stage protocol does not have any prognostic correlation. In contrast, as shown previously in many studies, size is an important prognosticator, and a size-based T-stage protocol is more applicable and has prognostic value in PDAC.


Similar content being viewed by others
References
Edge SB, Byrd DR, Compton CG, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual, 7th ed. New York: Springer, 2010.
Park H, An S, Eo SH, et al. Survival effect of tumor size and extrapancreatic extension in surgically resected pancreatic cancer: proposal for improved T classification. Hum Pathol. 2014;45:2341–6.
Brennan MF, Kattan MW, Klimstra D, Conlon K. Prognostic nomogram for patients undergoing resection for adenocarcinoma of the pancreas. Ann Surg. 2004;240:293–8.
Wagner M, Redaelli C, Lietz M, Seiler CA, Friess H, Buchler MW. Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br J Surg. 2004;91:586–94.
Lim JE, Chien MW, Earle CC. Prognostic factors following curative resection for pancreatic adenocarcinoma: a population-based, linked database analysis of 396 patients. Ann Surg. 2003;237:74–85.
Ferrone CR, Pieretti-Vanmarcke R, Bloom JP, et al. Pancreatic ductal adenocarcinoma: long-term survival does not equal cure. Surgery. 2012;152:S43–9.
Magistrelli P, Antinori A, Crucitti A, et al. Prognostic factors after surgical resection for pancreatic carcinoma. J Surg Oncol. 2000;74:36–40.
Kent TS, Sachs TE, Sanchez N, Vollmer CM Jr, Callery MP. Conditional survival in pancreatic cancer: better than expected. HPB Oxford. 2011;13:876–80.
Richter A, Niedergethmann M, Sturm JW, Lorenz D, Post S, Trede M. Long-term results of partial pancreaticoduodenectomy for ductal adenocarcinoma of the pancreatic head: 25-year experience. World J Surg. 2003;27:324–9.
de Jong MC, Li F, Cameron JL, et al. Reevaluating the impact of tumor size on survival following pancreaticoduodenectomy for pancreatic adenocarcinoma. J Surg Oncol. 2011;103:656–62.
Weber A, Kehl V, Mittermeyer T, et al. Prognostic factors for survival in patients with unresectable pancreatic cancer. Pancreas. 2010;39:1247–53.
Takai S, Satoi S, Toyokawa H, et al. Clinicopathologic evaluation after resection for ductal adenocarcinoma of the pancreas: a retrospective, single-institution experience. Pancreas. 2003;26:243–9.
Hartwig W, Hackert T, Hinz U, et al. Pancreatic cancer surgery in the new millennium: better prediction of outcome. Ann Surg. 2011;254:311–9.
Adsay NV, Basturk O, Altinel D, et al. The number of lymph nodes identified in a simple pancreatoduodenectomy specimen: comparison of conventional vs orange-peeling approach in pathologic assessment. Mod Pathol. 2009;22:107–12.
Adsay NV, Basturk O, Saka B, et al. Whipple made simple for surgical pathologists: orientation, dissection, and sampling of pancreaticoduodenectomy specimens for a more practical and accurate evaluation of pancreatic, distal common bile duct, and ampullary tumors. Am J Surg Pathol. 2014;38:480–93.
Washington K, Berlin J, Branton P, Burgart LJ. CAP cancer reporting protocols: protocol for the examination of specimens from patients with carcinoma of the exocrine pancreas, 2013. http://www.cap.org/ShowProperty?nodePath=/UCMCon/Contribution%20Folders/WebContent/pdf/pancreasexo-13protocol-3201.pdf. Accessed 25 Jan 2016.
Bosman FT, Carneiro F, H HR, Theise ND. WHO classification of tumors of digestive system. Lyon: WHO Press; 2010.
Hruban R, Pitman MB, Klimstra DS. Tumors of the Pancreas. Washington, DC: American Registry of Pathology; 2007.
Adsay V, Ohike N, Tajiri T, et al. Ampullary region carcinomas: definition and site-specific classification with delineation of four clinicopathologically and prognostically distinct subsets in an analysis of 249 cases. Am J Surg Pathol. 2012;36:1592–608.
Gonzalez RS, Bagci P, Kong SY, et al. Distal common bile duct adenocarcinoma: analysis of 47 cases and comparison with pancreatic and ampullary ductal carcinomas (abstract). Mod Pathol. 2014;25:109A.
Gönen M, Heller G. Concordance probability and discriminatory power in proportional hazards regression. Biometrika. 2005;92:965–70.
Oliva IV, Bandyopadhyay S, Coban I, et al. Incidence and significance of common bile duct involvement in resected pancreatic ductal adenocarcinomas: should it be represented in the TNM staging? (abstract). Mod Pathol. 2009;22:319A.
Verbeke CS. Resection margins and R1 rates in pancreatic cancer-are we there yet? Histopathology. 2008;52:787–96.
Esposito I, Kleeff J, Bergmann F, et al. Most pancreatic cancer resections are R1 resections. Ann Surg Oncol. 2008;15:1651–60.
Schlitter AM, Esposito I. Definition of microscopic tumor clearance (R0) in pancreatic cancer resections. Cancers Basel. 2010;2:2001–10.
Oettle H, Neuhaus P, Hochhaus A, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310:1473–81.
Oettle H, Post S, Neuhaus P, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007;297:267–77.
Neoptolemos JP, Dunn JA, Stocken DD, et al. Adjuvant chemoradiotherapy and chemotherapy in resectable pancreatic cancer: a randomised controlled trial. Lancet. 2001;358:1576–85.
Neoptolemos JP, Stocken DD, Friess H, et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med. 2004;350:1200–10.
Sinn M, Striefler JK, Sinn BV, et al. Does long-term survival in patients with pancreatic cancer really exist? Results from the CONKO-001 study. J Surg Oncol. 2013;108:398–402.
Hamidian Jahromi A, Zibari GB, Jafarimehr E, et al. Peripancreatic soft tissue involvement: independent outcome predictor in patients with resected pancreatic adenocarcinoma. Int Surg. 2014;99:62–70.
De La Cruz MS, Young AP, Ruffin MT. Diagnosis and management of pancreatic cancer. Am Fam Physician. 2014;89:626–32.
Yamada S, Fujii T, Sugimoto H, et al. Aggressive surgery for borderline resectable pancreatic cancer: evaluation of National Comprehensive Cancer Network guidelines. Pancreas. 2013;42:1004–10.
Evans DB, Farnell MB, Lillemoe KD, Vollmer C Jr, Strasberg SM, Schulick RD. Surgical treatment of resectable and borderline resectable pancreas cancer: expert consensus statement. Ann Surg Oncol. 2009;16:1736–44.
Katz MH, Crane CH, Varadhachary G. Management of borderline resectable pancreatic cancer. Semin Radiat Oncol. 2014;24:105–12.
Rohan VS, Hsu JT, Liu KH, et al. Long-term results and prognostic factors in resected pancreatic body and tail adenocarcinomas. J Gastrointest Cancer. 2013;44:89–93.
Ueda M, Endo I, Nakashima M, et al. Prognostic factors after resection of pancreatic cancer. World J Surg. 2009;33:104–10.
You DD, Lee HG, Heo JS, Choi SH, Choi DW. Prognostic factors and adjuvant chemoradiation therapy after pancreaticoduodenectomy for pancreatic adenocarcinoma. J Gastrointest Surg. 2009;13:1699–706.
Geer RJ, Brennan MF. Prognostic indicators for survival after resection of pancreatic adenocarcinoma. Am J Surg. 1993;165:68–72; discussion 72–63.
Sohn TA, Yeo CJ, Cameron JL, et al. Resected adenocarcinoma of the pancreas–616 patients: results, outcomes, and prognostic indicators. J Gastrointest Surg. 2000;4:567–79.
Moon HJ, An JY, Heo JS, Choi SH, Joh JW, Kim YI. Predicting survival after surgical resection for pancreatic ductal adenocarcinoma. Pancreas. 2006;32:37–43.
Matsumoto G, Muta M, Tsuruta K, Horiguchi S, Karasawa K, Okamoto A. Tumor size significantly correlates with postoperative liver metastases and COX-2 expression in patients with resectable pancreatic cancer. Pancreatology. 2007;7:167–73.
Winter JM, Cameron JL, Campbell KA, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg. 2006;10:1199–210; discussion 1210–1191.
Kloppel G, Rindi G, Perren A, Komminoth P, Klimstra DS. The ENETS and AJCC/UICC TNM classifications of the neuroendocrine tumors of the gastrointestinal tract and the pancreas: a statement. Virchows Arch. 2010;456:595–7.
House MG, Gonen M, Jarnagin WR, et al. Prognostic significance of pathologic nodal status in patients with resected pancreatic cancer. J Gastrointest Surg. 2007;11:1549–55.
Pawlik TM, Gleisner AL, Cameron JL, et al. Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery. 2007;141:610–8.
Japan Pancreas Society. Classification of pancreatic carcinoma. 3rd English ed. Tokyo: Kanehara; 2011.
General rules for the study of pancreatic cancer. 6th ed. in Japanese, revised. Tokyo: Kanehara; 2013.
Staley CA, Cleary KR, Abbruzzese JL, et al. The need for standardized pathologic staging of pancreaticoduodenectomy specimens. Pancreas. 1996;12:373–80.
Luttges J, Zamboni G, Kloppel G. Recommendation for the examination of pancreaticoduodenectomy specimens removed from patients with carcinoma of the exocrine pancreas: a proposal for a standardized pathological staging of pancreaticoduodenectomy specimens including a checklist. Dig Surg. 1999;16:291–6.
Chatelain D, Flejou JF. Pancreatectomy for adenocarcinoma: prognostic factors, recommendations for pathological reports. Ann Pathol. 2002;22:422–31.
Verbeke CS, Gladhaug IP. Resection margin involvement and tumour origin in pancreatic head cancer. Br J Surg. 2012;99:1036–49.
Verbeke CS, Leitch D, Menon KV, McMahon MJ, Guillou PJ, Anthoney A. Redefining the R1 resection in pancreatic cancer. Br J Surg. 2006;93:1232–7.
Verbeke CS, Menon KV. Redefining resection margin status in pancreatic cancer. HPB Oxford. 2009;11:282–9.
The Royal College of Pathologists of United Kingdom Standards and Datasets for Reporting Cancers. Data set for the histopathological reporting of carcinomas of the pancreas, ampulla of vater, and common bile duct, 2013. http://www.rcpath.org/NR/rdonlyres/954273A2-3F01-4B97-B0F6-C136231DF65F/0/datasethistopathologicalreportingcarcinomasmay10.pdf. Accessed 24 Dec 2013.
Maksymov V, Hogan M, Khalifa MA. An anatomical-based mapping analysis of the pancreaticoduodenectomy retroperitoneal margin highlights the urgent need for standardized assessment. HPB Oxford. 2013;15:218–23.
Slidell MB, Chang DC, Cameron JL, et al. Impact of total lymph node count and lymph node ratio on staging and survival after pancreatectomy for pancreatic adenocarcinoma: a large, population-based analysis. Ann Surg Oncol. 2008;15:165–74.
Tomlinson JS, Jain S, Bentrem DJ, et al. Accuracy of staging node-negative pancreas cancer: a potential quality measure. Arch Surg. 2007;142:767–23; discussion 773–764.
Schwarz RE, Smith DD. Extent of lymph node retrieval and pancreatic cancer survival: information from a large US population database. Ann Surg Oncol. 2006;13:1189–200.
Basturk O, Saka B, Balci S, et al. Substaging of lymph node status in resected pancreatic ductal adenocarcinoma has strong prognostic correlations: proposal for a revised N classification for TNM staging. Ann Surg Oncol. 2015;22(Suppl 3)1187–95.
Disclosure
Volkan Adsay has a Grant from National Institutes of Health (#5P50 CA62924). Lauren M. Postlewait has received funding from the Katz Foundation. For the remaining authors none were declared. This study is also supported in parts by funds generously donated by Monastra Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Burcu Saka and Serdar Balci have contributed equally to the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Saka, B., Balci, S., Basturk, O. et al. Pancreatic Ductal Adenocarcinoma is Spread to the Peripancreatic Soft Tissue in the Majority of Resected Cases, Rendering the AJCC T-Stage Protocol (7th Edition) Inapplicable and Insignificant: A Size-Based Staging System (pT1: ≤2, pT2: >2–≤4, pT3: >4 cm) is More Valid and Clinically Relevant. Ann Surg Oncol 23, 2010–2018 (2016). https://doi.org/10.1245/s10434-016-5093-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5093-7