Abstract
Lung cancer is the leading cause of cancer-related deaths worldwide, resulting in the highest mortality rates among both men and women with respect to all other types of cancer. Difficulties in treating lung cancer arise from late-stage diagnoses and tumor heterogeneity and current treatment involves a combination of chemotherapeutics, surgery, and radiation. Chemotherapeutics administered systemically can lead to undesirable side effects and severe off-site toxicity. For example, chronic administration of the chemotherapeutic doxorubicin (DOX) leads to cardiotoxicity, thereby limiting its long-term use. Systemic administration of the highly lipophilic molecule paclitaxel (PTX) is hindered by its water solubility, necessitating the use of solubilizing agents, which can induce side effects. Thus, in this investigation, formulations consisting of spray-dried microparticles (MP) containing DOX and PTX were produced to be administered as dry powder aerosols directly to the lungs. Acetalated dextran (Ac-Dex) was used as the polymer in these formulations, as it is a biocompatible and biodegradable polymer that exhibits pH-responsive degradation. Solid-state characterization revealed that DOX and PTX remained in solubility favoring amorphous states in the MP formulations and that both drugs remained thermally stable throughout the spray drying process. In vitro release studies demonstrated the pH sensitivity of the formulations due to the use of Ac-Dex, as well as the release of both therapeutics over the course of at least 48 h. In vitro aerosol dispersion studies demonstrated that both formulations exhibited suitable aerosol dispersion properties for deep lung delivery.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the leading cause of cancer-related deaths worldwide, resulting in an estimated 1.8 million deaths in 2020 [1]. Patients diagnosed with lung cancer have a very bleak prognosis, with a 5-year survival of only 18.6% [2, 3]. A closer look at this prognosis reveals that early detection and the stage of disease progression can drastically influence clinical outcomes, as the 5-year survival of localized lung cancer not spread to other organs is closer to 56% [4]. As a result, the treatment regimen for lung cancer depends mainly on how far along the disease has progressed [5]. Typically, surgical resection is the first course of action, and if possible, is followed by chemotherapy and radiation treatments.
First-line chemotherapeutics used to treat lung cancer typically involve platinum-based compounds such as cisplatin and carboplatin [6]. However, previous studies have shown enhanced clinical benefits such as longer survival rate and slower disease progression in patients treated with a combinatorial chemotherapeutic regiment in which both a platinum-based chemotherapeutic and a non-platinum based chemotherapeutic such as doxorubicin (DOX) or paclitaxel (PTX) are administered together [7, 8]. DOX is an anthracycline that intercalates with DNA base pairs, leading to the inhibition of DNA and RNA synthesis, while also generating free radicals, which can lead to cell membrane, protein, and DNA damage [9]. DOX is commonly administered intravenously, which can lead to side effects including nausea, vomiting, and alopecia [10]. More serious side effects that limit the long term use of DOX include cardiotoxicity and tissue ulceration or necrosis [11].
PTX is a poorly water soluble chemotherapeutic that works by interfering with cancer cell division via microtubule stabilization [12]. Although effective in the treatment of a variety of cancers, PTX is typically administered intravenously and patients have reported side effects from PTX including fatigue, neuropathy, and hepatotoxicity [13]. The highly lipophilic nature of PTX, along with its lack of ionizable functional groups, has posed a major challenge in the development of PTX formulations [14]. Currently, polyoxyethylated castor oil (Cremophor EL) and ethanol are used as solubilizers in PTX for intravenous administration, but the risk of PTX precipitation and side effects attributed to these solubilizers can hinder the efficiency of PTX [15].
Acetalated dextran (Ac-Dex) is a biocompatible polymer that exhibits pH-mediated degradation, which can be beneficial in developing targeted particle-based formulations [16,17,18,19]. Ac-Dex degrades more quickly in acidic environments, which is suitable for targeting acidic tumor microenvironments [20], where drug-loaded particles can ferry chemotherapeutics with minimal release in pH-neutral tissue, subsequently releasing the drug payload when reaching the acidic tumor parenchyma. In addition, in the synthesis of Ac-Dex the reaction time modulates the cyclic-to-acyclic ratio acetal coverage on the polymer, which plays a key role in determining the degradation rate of the resulting polymer, where longer reaction time results in slower degrading Ac-Dex [21].
Chemotherapy-based formulations such as drug-loaded dry powder particles can be delivered via pulmonary administration, thereby offering many inherent advantages over systemically delivered oral or intravenous formulations [22]. Such advantages include improved drug stability, reduced systemic side effects, improved drug bioavailability, and the ability to circumvent physiological barriers such as the first pass metabolism [23]. Spray drying has been used to produce aerosolized dry powder microparticle formulations from a variety of solutions and suspensions [17, 24,25,26,27,28,29]. In particular, spray-dried microparticles can be produced that exhibit specific size and shape characteristics depending on spray drying parameters such as pump rate, aspiration rate, and temperature in addition to formulation parameters such as feed concentration or the type of solvent(s) used during microparticle production [30]. For effective pulmonary administration as dry powders, microparticles should exhibit a size between 0.5–5 µm diameter, as particles smaller than 0.5 µm are easily exhaled during normal breathing and particles larger than 5 µm will likely get trapped in the upper airways [31, 32].
In this investigation, two dry powder aerosol microparticle formulations consisting of a chemotherapeutic (DOX or PTX) and Ac-Dex were developed for the potential localized treatment of lung cancer. The resulting formulations were evaluated for their physicochemical, drug release, and aerosol dispersion properties with the goal of overcoming the limitations inherent to conventional lung cancer treatments. To our knowledge, this is the first time DOX and PTX have been formulated into spray-dried aerosol microparticle formulations.
Materials and Methods
Materials
Dextran from Leuconoctoc mesenteroides (9–11 kDa), phosphate buffered saline (PBS) powder, pyridinium p-toluenesulfonate (PPTS, 98%), D-mannitol (≥ 98%), 2-methoxypropene (2-MOP, 97%), triethylamine (TEA, ≥ 99%), anhydrous dimethyl sulfoxide (DMSO, ≥ 99.9%), ethanol (reagent grade, denatured), acetonitrile ( Omnisolv® ACN, LC–MS grade ≥ 99.9%), acetic acid (ReagentPlus®, ≥ 99.9%), anhydrous sodium acetate, and Tween80® were obtained from Sigma-Aldrich (St. Louis, MO). Doxorubicin hydrochloride salt (DOX, 579.98 Da) and paclitaxel (PTX, 853.91 Da) were purchased from LC Laboratories (Woburn, MA).
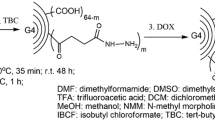
Synthesis of Acetalated Dextran
As seen in Figure A1, acetalated dextran (Ac-Dex) was synthesized according to a previously described method [33]. Briefly, dextran (1 g) and PPTS (25 g) were dissolved in DMSO (10 mL) under stirring. To initiate the reaction, 2-MOP (5 mL) was added to the solution. After 3 h, TEA was added to quench the reaction and the solution was transferred to a basic water solution (pH 9), which facilitated the precipitation of Ac-Dex. The precipitate was filtered and rinsed with basic water, frozen, and stored in a desiccator at –20°C until further use.
Preparation of Paclitaxel-loaded Microparticles via Spray Drying
Paclitaxel-loaded microparticles (PTX MP) were prepared by combining Ac-Dex and PTX ethanol (10% w/w PTX) to create a 1% w/v solution, as seen in Figure A2. The solution was fed into a Büchi B-290 spray dryer coupled with a B-295 inert loop (Büchi Labortechnik, AG, Switzerland) at the following conditions: inlet temperature of 100 ℃; pump rate of 1.5 mL/min; gas flow rate of 414 L/h; and aspiration rate of 35 m3/h. The dry particles were stored at − 20°C in a desiccator for further use.
Preparation of Doxorubicin-loaded Microparticles via Spray Drying
Doxorubicin-loaded microparticles (DOX MP) were prepared by spray drying an ethanol/water mixture that consisted of Ac-Dex in ethanol (10% w/v, 27 mL) and DOX in water (10% w/v, 30 mL). The ethanol and water solutions were combined, vortexed, and sonicated to ensure complete mixing, resulting in 10% w/w DOX and 1% w/v final solution for spray drying, as seen in Figure A2. DOX MP were obtained by spray drying the solution using the conditions described for PTX MP. The resulting yield of both formulations was calculated using the following equation:
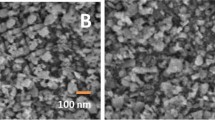
Scanning Electron Microscopy (SEM) and ImageJ Analysis
The size and morphology of the formulations were evaluated via scanning electron microscopy (SEM) using a Zeiss SIGMA VP Field Emission-SEM (Germany). The samples were sputter coated with a thin film of gold/palladium alloy (10 nm) in a BIO-RAD system at 20 µA for 10 s under argon gas. Images were captured at 3 kV. Particles in SEM micrographs were analyzed using ImageJ software (Systat, San Jose, CA, USA) using at least 100 MP to determine their geometric diameter (dg).
Physicochemical Characterization
Thermal transition events of the formulations and their raw components were determined via differential scanning calorimetry (DSC). Each sample was weighed into an aluminum pan (5–10 mg) and hermetically sealed. An empty pan of similar mass was used as reference. Reference and sample pans were heated from 0–180°C at a rate of 10°C/minute. The crystallinity of the formulations and their raw materials was evaluated using a Rigaku Multiflex X-ray diffractometer (The Midlands, TX) with a Cu Kα radiation source at 40 kV and 44 mA. Samples were deposited onto a 3 mm horizontal quartz glass holder for analysis and scans were performed from 5–60° (2θ) with a step width of 0.2° and a scan rate of 2°/min. Fourier transform infrared (FTIR) spectroscopy was used to investigate the infrared activity of the raw materials and formulations using a Shimadzu IRAffinity-1S spectrometer (Shimadzu, Japan). Each recorded spectrum is the average of 24 scans per sample using a wavenumber range from 4000 to 500 cm−1. Thermal gravimetric analysis (TGA) was used to evaluate the decomposition profiles of the raw materials and formulations using a TA Instruments TGA Q500 (New Castle, DE). Samples were heated from 0 to 500°C at a rate of 10°C/min.
Quantification of Drug Loading in Paclitaxel-Loaded Microparticles
The amount of PTX loaded into the PTX MP was evaluated via high-performance liquid chromatography (HPLC) using a Shimadzu Nexera I 2040c (Japan) equipped with a UV absorbance detector set at 227 nm. The mobile phase consisted of water and acetonitrile (45% v/v). Solute separation was achieved using an Ascentis C18 column (150 × 4.6 mm, 5 µm) with a flow rate of 1 mL/min and 10 μL sample injection volume. A PTX stock solution (1 mg/mL) was prepared in ethanol followed by the preparation of PTX standards via serial dilutions in the mobile phase. A standard curve was generated for PTX (see Figure A3). Prior to HPLC analysis, PTX MP were dissolved in the mobile phase at 1 mg/mL and PTX loading was determined using the following equation:
Quantification of Drug Loading in Doxorubicin-Loaded Microparticles
The amount of DOX loaded into DOX MP was evaluated via fluorescence spectroscopy using a Cytation 3 plate reader (BioTek Instruments Inc., Winooski, VT) at excitation and emission wavelengths of 460 nm and 595 nm, respectively. Stock DOX solutions (1 mg/mL) were prepared in water and standards were prepared via serial dilution from the stock solution. A standard curve was generated for (see Figure A3). Prior to analysis, DOX MP were dissolved in ethanol at 1 mg/mL. DOX loading was determined using the following equation:
The encapsulation efficiencies (EE) of the formulations were calculated using the following equation:
Analysis of In Vitro Drug Release from Spray-Dried Microparticles
Drug release from PTX MP and DOX MP was evaluated in acetate buffer (0.1 M, pH 5.0, 0.5% w/v Tween 80) designed to mimic tumor microenvironment [20] or PBS (pH 7.4, 0.5% w/v Tween 80) designed to mimic physiological pH. The MP formulations were dissolved in release medium at 1 mg/mL, vortexed, then placed in a sample shaker at 200 rpm and 37°C. Samples were covered with aluminum foil to protect against photodegradation. At designated time points, samples were centrifuged at 5534 × g at 4°C for 5 min and supernatant was withdrawn, placed in centrifuge tubes, and stored at –20°C until further analysis. An equal volume of fresh buffer was added to each sample and they were returned to the sample shaker until the next time point.
The release data were fit to several commonly-used semi-empirical release kinetic models, including zero order [34,35,36], first order [36,37,38], Korsmeyer-Peppas [39, 40], Higuchi [41, 42], and Hixson-Crowell [43] models, as shown in Table I. Given the limitations in using the coefficient of determination (R2) to fit the data to the models, the adjusted coefficient of determination (\({R}_{adjusted}^{2}\)) was calculated to provide a more meaningful analysis of drug release kinetics [44], as seen below:
where n is the number of dissolution data points, p is the number of parameters in the model, and R2 is the original coefficient of determination determined by fitting the data to each semi-empirical model.
In Vitro Aerosol Dispersion Performance of Microparticle Formulations
The in vitro aerosol dispersion characteristics of the MP formulations were determined using a Next Generation Impactor (NGI, MSP Corporation, Shoreview, MN) equipped with a stainless-steel induction port (USP throat adaptor) attachment and stainless-steel gravimetric insert cups. The NGI was attached to a Copley HCPS vacuum pump and the airflow rate was set to 60 L/min to model the flow rate of a healthy adult lung [45]. Glass fiber filters (55 mm, Type A/E, Pall Life Sciences, PA) were placed in the gravimetric cups corresponding to stages 1 through 7 to minimize bounce or re-entrapment. The filter mass was recorded before and after each experiment. Each MP formulation (6–8 mg) was placed into a hydroxypropyl methylcellulose capsule (HPMC, size 3, Quali-V, Qualicaps Inc., Whitsett, NC) which was placed into a human dry powder inhaler device (HandiHaler, Boehringer Ingelhelm Pharmaceuticals, CT) attached to a custom rubber mouthpiece connected to the NGI. Three HPMC capsules were loaded and released for each measurement and all experiments were run in triplicate. The NGI was run with a delay time of 3 s and a running time of 10 s. For an airflow rate of 60 L/min, the effective cutoff diameter for each stage was as follows: stage 1 (8.06 μm), stage 2 (4.46 μm), stage 3 (2.82 μm), stage 4 (1.66 μm), stage 5 (0.94 μm), stage 6 (0.55 μm), and stage 7 (0.34 μm). The following equations were used to determine the fine particle dose (FPD), fine particle fraction (FPF), respirable dose (RD), and emitted dose (ED):
The experimental mass median aerodynamic diameter (MMADE) and geometric standard deviation (GSD) for the MP were determined using a Mathematica® program written by Dr. Warren Finlay [46, 47].
Tapped Density and Theoretical Aerodynamic Diameter Analysis
The tapped density (ρT) of the MP formulations was evaluated via tapped density measurements as previously described [48], where 20–25 mg of MP (m) was added to a thin glass tube and tapped 200 times on a hard surface to ensure efficient packing. The volume (V) occupied by the MP was measured using a digital caliper and ρT was calculated using the following equation:
The theoretical mass median aerodynamic diameter (MMADT) of the formulations was calculated using the following equation:
where dg is the geometric diameter of the particle determined via SEM and ρref is the reference density of solid polymer (1 g/cm3).
Statistical Analysis
All measurements were performed in at least triplicate (n ≥ 3). Statistical significance for all studies was determined using two-tailed students t-test in Microsoft Excel. A p-value < 0.05 was considered as statistically significant.
Results
Spray drying was used to produce dry powder paclitaxel-loaded microparticles (PTX MP) and doxorubicin-loaded microparticles (DOX MP) as seen in Figure A2. The resulting yield of the MP following spray drying was 32 and 46% for PTX MP and DOX MP, respectively. As shown in Fig. 1, PTX MP exhibited collapsed, corrugated morphology, whereas DOX MP were more spherical with a rough surface morphology. Both formulations were fairly heterogeneous in nature, as seen in the zoomed in images in Supplemental Information (Figure A4).
Neither raw PTX nor raw DOX exhibited thermal transition events in the temperature range tested (up to 180°C), whereas raw acetalated dextran (Ac-Dex) exhibited an endothermal transition at 168°C (see Fig. 2a). In comparison, DOX MP and PTX MP exhibited endothermic transitions at 150 and 145°C, respectively. In the x-ray diffractograms (Fig. 4b), raw PTX and DOX exhibited numerous sharp, distinct peaks, ranging from 5–30° and 13–30°, respectively, and these compounds exhibited ordered and well-defined microstructures, as seen in Figure A3. In comparison, raw Ac-Dex, PTX MP, and DOX MP exhibited broad diffraction patterns from 10–25°.
Solid-state characterization of spray-dried microparticles and their raw components, including: a differential scanning calorimetry, b x-ray diffraction, c Fourier-transform infrared spectroscopy, and d thermogravimetric analysis. Analyzed samples include paclitaxel-loaded microparticles (PTX MP), doxorubicin-loaded microparticles (DOX MP), raw PTX, raw DOX, and raw acetalated dextran (Ac-Dex)
As shown in Figs. 2C and A5, raw DOX exhibited the following absorbance peaks, which were determined via Fourier transform infrared (FTIR) spectroscopy: 3325 cm–1 from N–H stretching, 3531 cm–1 from O–H stretching, 2929 cm–1 and 2897 cm–1 from C-H stretching, 1730 cm–1 from C = O stretching, 1616 cm–1, 1581 cm–1, and 1414 cm–1 from C = C ring stretching, 1115 cm–1 and 1072 cm–1 from C–O–C stretching, 805 cm–1 from C = H bending, and 688 cm–1 from C = C ring bending. Raw PTX exhibited the following absorbance peaks: 3515 to 3300 cm−1, from N–H stretching, 1735 cm−1 from C = O stretching, 1645 cm−1 for an amide bond, and 1072 cm−1, 985 cm−1, and 704 cm−1 from aromatic bond vibrations. Raw DOX and raw PTX exhibited identifiable absorption peaks in the 1750 to 1480 cm−1 range that disappeared in the DOX MP and PTX MP spectra that are distinct peaks separate from those that occur in raw Ac-Dex. In addition, the Ac-Dex sample exhibited peaks in the 1450–750 cm−1 range, which correspond to acetal functional groups, likely attributed to hydroxyl conversion to acetal formation during the Ac-Dex synthesis process [49].
Thermalgravimetric analysis (TGA), as shown in Fig. 2d, showed that raw Ac-Dex, PTX MP, and DOX MP exhibited decomposition between 138 and 142°C, whereas raw DOX and raw PTX exhibited decomposition at 220 and 235°C, respectively.
High performance liquid chromatography (HPLC) and fluorescence spectroscopy were used to analyze the loading of PTX and DOX in the spray-dried MP, respectively, and to evaluate drug release. As seen in Figure A3, the resulting calibration curves demonstrated linearity between the measured absorbance and PTX concentrations and measured fluorescence and DOX concentrations. In particular, the PTX calibration curve exhibited linearity from 0.78 to 12.5 µg PTX/mL with a coefficient of determination (R2 value) of 0.997, and the DOX calibration curve demonstrated linearity from 0.19 to 6.25 µg DOX/mL with an R2 value of 0.999.
Both PTX and DOX MP formulations exhibited high drug loading and encapsulation efficiency (EE) values, as seen in Table I. As shown in Fig. 3, after one week, 21% of PTX was released from the PTX MP at pH 7.4, whereas 82% of PTX was released at pH 5.0 after 3 days. There was a noticeable increase in PTX release at pH 5.0 after 24 h, with the cumulative PTX release increasing from 8% at the 8-h mark to 56% at the 24-h mark. In comparison, DOX MP exhibited a burst release of DOX, with 54 and 55% of DOX being released after 30 min at pH 7.4 and pH 5.0, respectively. The release of DOX from DOX MP plateaued at 48 h, with 70% and 65% of DOX released at pH 5.0 and pH 7.4, respectively. There was no statistically significant difference between the DOX release values at any time point for the two different pH environments (Table II).
In vitro drug release profiles of (Left) paclitaxel-loaded microparticles (PTX MP) and (Right) doxorubicin-loaded microparticles (DOX MP) in modified phosphate buffer solution (0.1 M, pH 7.4) or sodium acetate buffer (0.1 M, pH 5.0) with 0.5% Tween 80 at 37°C. Data represent mean ± standard deviation (n = 3)
In this investigation, the drug release data from PTX MP and DOX MP were fitted to several semi-empirical kinetic release models, including the zero-order [34,35,36], first-order [36,37,38], Korsmeyer-Peppas [39, 40], Higuchi [41, 42], and Hixson-Crowell [43] models, the equations of which are shown in Table I. The resulting model parameters and corresponding adjusted coefficients of determination (R2) values were then calculated for each model and are summarized in Table III (select parameters with the best fit) and Table AI (all data). Based on the R2 values, the PTX release data fit the Higuchi model best at both pH release conditions, where the Higuchi release rate constant for PTX MP was fivefold higher at pH 5.0 versus pH 7.4 (p = 0.004). In comparison, the DOX release data fit the Korsmeyer-Peppas model best, but only fit well for pH 5.0 conditions, where the resulting release rate constants and exponents were similar at both pH conditions at approximately 55%/h1.74 and 1.74 au, respectively.
The aerosol dispersion and size characteristics of the spray-dried formulations can be seen in Fig. 4. Both DOX MP and PTX MP deposited on all stages of the Next Generation Impactor following aerosolization, with the majority of particles depositing on stages 2 through 5. The two formulations exhibited similar dispersion properties, with the fine particle fraction (FPF), respirable dose (RD), and emitted dose (ED) values ranging from 90–93, 70–97, and 70%, respectively. The corresponding fine particle dose and emitted dose values can be found in Table II. Both formulations exhibited geometric diameters close to 2 µm, whereas their theoretical mass median aerodynamic (ADT) and experimental mass median aerodynamic (ADE) values were approximately 1 and 3 µm, respectively. The geometric standard deviation (GSD) values for both formulations were slightly less than 2 µm and the tapped densities of the formulations were fairly low (e.g., ≤ 0.25 g/cm3), as seen in Table II.
In vitro aerosol dispersion performance of paclitaxel-loaded microparticles (PTX MP) and doxorubicin-loaded microparticles (DOX MP). a Percentage (%) of particles deposited on each stage of the Next Generation Impactor (NGI). b Fine particle fraction (FPF), respirable dose (RD), and emitted dose (ED) aerosol characteristics of the microparticle systems. c Size analysis of microparticles, including geometric diameter (dg), theoretical mass median aerodynamic diameter (ADT), experimental mass median aerodynamic diameter (ADE), and geometric standard deviation (GSD). Data represent mean ± standard deviation (n = 3)
Discussion
Spray-dried acetalated dextran (Ac-Dex)-based microparticles (MP) loaded with paclitaxel (PTX) or doxorubicin (DOX) were formulated as dry powder aerosol therapeutics for the potential treatment of lung cancer (see Figure A2) and the formulations were characterized for their physicochemical, drug release, and aerosol dispersion properties as an initial proof-of-concept study. In the case of spray drying, the resulting particle morphology is highly dependent on what occurs during droplet drying, which is governed by the spray drying conditions (e.g., pump rate, inlet temperature, etc.) used to produce the particles [16, 24, 25, 30, 50, 51].
In order to elucidate the impact of the type of drug and spray drying solvent on the formulations evaluated in this study, the other spray drying conditions were kept constant. Given this, the morphological differences in the particles can be attributed to the different solvent compositions of the feed solutions. The DOX MP feed solution involved a co-solvent containing both water and ethanol, whereas the PTX MP feed solution contained only ethanol. As ethanol has a lower boiling point than water, it will more readily evaporate under the same conditions. Thus, for the PTX MP prepared in ethanol, the higher evaporation rate led to the formation of collapsed structures, as the solutes did not have time to form a homogenous dispersion inside of the droplet during the drying process [52]. In comparison, for the DOX MP formulation containing water and ethanol, the evaporation rate of the co-solvent is slower due to the presence of water, allowing more time for the solutes to form a homogeneous dispersion inside of the droplet during the drying, leading to more spherical structures [53,54,55]. Furthermore, DOX MP exhibited a 1.5-times higher spray drying yield, which can likely be attributed to the moisture present due to water, causing the particles to stick to the collection vial more readily than the ‘dry’ PTX MP formulation.
Differential scanning calorimetry (DSC) was performed to investigate the thermal transition events of the MP formulations and their raw compounds. Given that spray drying can impact the physicochemical traits of particle formulations [56, 57], DSC was performed up to 180°C, which was well above the temperature the spray drying conditions of this study (i.e., 100°C). The lack of transition peaks for raw PTX and DOX can be attributed to their melting temperatures being above 180°C at 222°C and 217°C, respectively, with no other transition events occurring below 200°C for these compounds [58, 59]. Overall, this analysis demonstrates that spray drying had no impact on thermal state of the particles at the given spray drying temperature.
The crystalline nature of the spray-dried MP and their raw components was investigated via x-ray diffraction (XRD), as crystallinity is a key characteristic of pharmaceutical formulations due to its impact on compound dissolution and drug bioavailability [60]. Pharmaceutical spray drying has been used to produce amorphous solid dispersions from poorly water-soluble crystalline compounds, typically resulting in formulations that exhibit enhanced solubility and bioavailability [51, 61, 62]. In this study, the sharp diffraction peaks seen for raw PTX and DOX indicate their crystalline behavior, which is in good agreement with previous reports confirming the crystallinity of raw PTX [63] and raw DOX [64]. In comparison, raw Ac-Dex and the spray-dried MP exhibited amorphous behavior, which is supported by the disappearance of the identifiable diffraction peaks inherent to the raw drugs and the presence of a broad diffraction patterns similar to raw Ac-Dex. The resulting amorphous nature of the spray-dried formulations has the potential to improve the solubility of the crystalline therapeutics.
Fourier transform infrared (FTIR) spectroscopy was performed to investigate the infrared activity of the MP and their raw materials. FTIR is useful in the detection of specific functional groups in a molecule in addition to ascertaining information regarding the crystallinity of a compound [65]. Overall, the spectra were in good agreement with previous studies [58, 66], which have reported that simplified spectra involving peak disappearance and peak attenuation (i.e., lower intensity signals) can indicate the disruption of crystalline domains in a compound [67]. Thus, the FTIR spectra supports the XRD and DSC data in that that DOX and PTX exhibit amorphous behavior when formulated into DOX MP and PTX MP.
TGA was performed to investigate the decomposition profiles of the MP formulations and raw compounds to ensure that the formulation components remained stable during the spray drying process. These resulting data indicated that the raw components and MP formulations exhibited decomposition temperatures well above the spray drying temperatures used in this investigation, thus demonstrating the thermal stability of the proposed formulations.
While aerosol microparticles offer the advantage of being delivered directly to the site of disease in the lungs, high drug loading is desirable in such formulations to help deliver therapeutically relevant concentrations to the lungs in an efficient manner, while minimizing the loss of potentially expensive therapeutics during the spray drying process [68]. In this study, PTX MP and DOX MP exhibited high drug loading and encapsulation efficiency (EE) values nearing and exceeding 100%, respectively. It has been shown that spray-dried microparticles can exhibited EE above 100% [28, 69], and this phenomena can likely be attributed to varying drug distribution in the particles based on size, where smaller particles with less drug are not captured during the spray drying process, thus skewing the drug loading data to be higher than the initial loading.
DOX MP and PTX MP were evaluated for their in vitro drug release characteristics in two physiologically relevant media, including acetate buffer (pH 5.0) to mimic the acidic environment inherent to tumor microenvironment and PBS (pH 7.4) to mimic healthy, disease-free tissue environments [20]. While the initial release data for the PTX MP were similar at the two pH conditions, this varied significantly after 8 h, which can be attributed to the acid-labile degradation of Ac-Dex, as seen in a previous studies [21, 70, 71]. In comparison, DOX MP exhibited similar drug release profiles in both pH conditions. A previous study showed that DOX is capable of forming dimers in the presence of buffers, leading to the precipitation of DOX [72], and that this precipitation is time-dependent and is accelerated at higher temperatures and in higher pH environments. Thus, this may help explain why in this investigation, 100% release of DOX from DOX MP was not achieved, as some of the DOX may have dimerized and precipitated out in the release samples. Furthermore, the burst release of DOX from the MP may be attributed to the partitioning of DOX in water and Ac-Dex in ethanol, leaving precipitated DOX on the outside of the formulation. Thus, the different release profiles of DOX and PTX from the same polymer system can likely be attributed to the fact that PTX is encapsulated in the microparticles during spray drying, whereas the DOX is more readily available on the surface of the particles.
Analysis of drug release kinetics via mathematical modelling can aid in formulation development and in the understanding of release behavior from complex pharmaceutical dosage forms [73]. In this study, PTX release data best fit the Higuchi release kinetics model, indicating that release from the PTX MP was governed by Fickian diffusion [74]. Furthermore, the significant difference in PTX release at low pH in comparison to neutral pH can be attributed to accelerated Ac-Dex degradation in acidic conditions [21].
In comparison, the release of DOX from DOX MP best followed the Korsmeyer-Peppas release model, which has been used to describe drug release from polymeric systems, where the Korsmeyer-Peppas release exponent (n) is used to describe the drug transport mechanism. For DOX release at both pH 7.4 and 5.0, n was 1.74, which describes the transport mechanisms as being Super Case II, where drug release is governed by matrix erosion for non-swellable systems [75]. Based on these data, DOX release from DOX MP is governed by multiple mechanisms, such as enhanced diffusion of water-soluble drug DOX in aqueous media in addition to polymer degradation, which may be more difficult to model accurately, which supports the low R2 values for the models utilized in this study [76].
One of the most important characteristics of pulmonary formulations impacting their therapeutic efficacy is their aerosol dispersion properties [46]. Both spray-dried formulations deposited across all stages of the NGI, indicating their potential to deposit in both the upper and lower airways of the lungs [31, 77, 78]. The FPF, which describes the amount of aerosolized particulates that can pass through the larynx and ciliated airways into the lower airways, was high for both PTX MP and DOX MP, indicating that the majority of each can reach the lower airways of the lungs. It is worthy to mention that the RF for PTX MP was very high (close to 100%), whereas the respirable fraction for PTX MP was closer to 73%. This can be attributed to both a relatively low emitted dose, which can be attributed to leftover formulation remaining in the capsules after running the NGI, and a higher percentage of particles deposited on the initial NGI stage (which is not accounted for in any of the equations used in this investigation). More wrinkled and raisin-like particle morphology, as seen for PTX MP platforms, may lead to enhanced particle surface area, which may then lead to enhanced particle–particle interactions and further lead to particle agglomeration and increased particle size [79]. This may also support the notion of increased particle deposition in the initial NGI stage, leading to a lowered respirable fraction for PTX MP.
The spray-dried formulations exhibited aerodynamic and geometric diameters that indicate their potential for deep lung penetration [80]. Previous studies have demonstrated that alveolar macrophages in rat models show maximum particle uptake in the 2–3 µm range [81]. Since the particles in this investigation exhibited geometric diameters < 2 µm, they may be able to avoid or demonstrate minimal macrophage uptake. In addition, the resulting MMADEXP and GSD values were similar to previously reported studies using similar spray drying conditions [53]. Furthermore, the MMADEXP values were higher than the MMADTHEOR values due to increased particle interactions and agglomeration during the aerosolization process [53].
Tapped density studies are important as they can provide quantitative information regarding the flowability of dry powders. Particle platforms that exhibit higher tapped density values often can be more easily packed than particles with lower tapped density values, typically resulting in poor dry powder flowability [82]. Both PTX MP and DOX MP exhibited low tapped density values, resulting in theoretical MMAD values that are smaller than geometric diameter values, indicating that actual particle densities are higher than reported via tapped density analysis [53]. In addition, it has been shown that particles exhibiting tapped density values below 0.4 g/cm2 can more effectively deposit in deeper lung regions [83].
Overall, these data indicate the potential for PTX MP and DOX MP to be used as dry powder aerosol therapeutics in the treatment of lung cancer, especially given their drug loading, thermal stability, amorphous nature, and aerosol dispersion characteristics. A challenge in the formulation of particle formulations utilizing a poorly water soluble polymer such as Ac-Dex is in encapsulating water soluble drugs, which was seen for the DOX MP formulation. This study is the first step in formulating a new treatment option for a disease the currently has very poor outcomes for patients.
Conclusion
In this investigation, two aerosol dry powder formulations loaded with chemotherapeutics were produced for the potential treatment of lung cancer. The MP platforms exhibited diameters suitable for minimizing alveolar macrophage uptake and maximizing aerosol dispersion. Results from TGA indicated that the materials remained thermally stable during spray drying and FTIR spectroscopy, DSC, and XRD results support the notion that both PTX and DOX exhibited amorphous behavior in the final formulations, which can be advantageous for enhancing solubility and bioavailability. In vitro release studies demonstrated the pH-dependent, sustained release of PTX from the MP due to the use Ac-Dex, whereas the release of DOX was independent of the pH of the release medium. The aerosol dispersion studies indicated that the MP formulations exhibited appropriate aerosol dispersion properties, including high FPF, relatively high respirable fraction, and low tapped density values, which will result in a large amount of the formulation reaching the alveolar region of the lungs. Overall, the formulations developed in this investigation present an intriguing alternative to current lung cancer treatment options.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–49.
Hassan Lemjabbar-Alaouia OH, Yanga Y-W, Buchanana P. Lung cancer: biology and treatment options. Physiol Behav. 2017;176:139–48.
Schroedl C, Kalhan R. Incidence, treatment options, and outcomes of lung cancer in patients with chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2012;18:131–7.
World Health Organization. Lung Cancer Fact Sheet 2023. 26 June 2023. https://www.who.int/news-room/factsheets/detail/lung-cancer.
Alam A, Ansari MA, Badrealam KF, Pathak S. Molecular approaches to lung cancer prevention. Future Oncol. 2021;17:1793–810.
Wittgen BP, Kunst PW, van der Born K, van Wijk AW, Perkins W, Pilkiewicz FG, et al. Phase I study of aerosolized SLIT cisplatin in the treatment of patients with carcinoma of the lung. Clin Cancer Res. 2007;13:2414–21.
Grossi F, Gridelli C, Aita M, De Marinis F. Identifying an optimum treatment strategy for patients with advanced non-small cell lung cancer. Crit Rev Oncol Hematol. 2008;67:16–26.
Ramalingam S, Belani CP. Paclitaxel for non-small cell lung cancer. Expert Opin Pharmacother. 2004;5:1771–80.
Thorn CF, Oshiro C, Marsh S, Hernandez-Boussard T, McLeod H, Klein TE, et al. Doxorubicin pathways. Pharmacogenet Genomics. 2011;21:440–6.
Azarmi S, Tao X, Chen H, Wang Z, Finlay WH, Löbenberg R, et al. Formulation and cytotoxicity of doxorubicin nanoparticles carried by dry powder aerosol particles. Int J Pharm. 2006;319(1-2):155–61.
Johnson-Arbor K, Dubey R. Doxorubicin. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459232/.
Weaver BA. How Taxol/paclitaxel kills cancer cells. Mol Biol Cell. 2014;25(18):2677–81.
Von Eiff D, Bozorgmehr F, Chung I, Bernhardt D, Rieken S, Liersch S, et al. Paclitaxel for treatment of advanced small cell lung cancer (SCLC): A retrospective study of 185 patients. J Thorac Dis. 2020;12:782–93.
Marupudi NI, Han JE, Li KW, Renard VM, Tyler BM, Brem H. Paclitaxel: a review of adverse toxicities and novel delivery strategies. Expert Opin Drug Saf. 2007;6:609–21.
Surapaneni MS, Das SK, Das NG. Designing paclitaxel drug delivery systems aimed at improved patient outcomes: current status and challenges. ISRN Pharmacol. 2012;2012:1–15.
Wang Z, Meenach SA. Optimization of acetalated dextran-based nanocomposite microparticles for deep lung delivery of therapeutics via spray-drying. J Pharm Sci. 2017;106:3539–47.
Wang Z, Meenach SA. Synthesis and characterization of nanocomposite microparticles (nCmP) for the treatment of cystic fibrosis-related infections. Pharm Res. 2016;33:1862–72.
Meenach SA, Kim YJ, Kauffman KJ, Kanthamneni N, Bachelder EM, Ainslie KM. Synthesis, optimization, and characterization of camptothecin-loaded acetalated dextran porous microparticles for pulmonary delivery. Mol Pharm. 2012;9:290–8.
Bachelder EM, Beaudette TT, Broaders KE, Dashe J, Fréchet JMJ. Acetal-Derivatized Dextran: An Acid-Responsive Biodegradable Material for Therapeutic Applications. J Am Chem Soc. 2008;130(32):10494–5.
Kato Y, Ozawa S, Miyamoto C, Maehata Y, Suzuki A, Maeda T, et al. Acidic extracellular microenvironment and cancer. Cancer Cell Int. 2013;13.
Bachelder EM, Beaudette TT, Broaders KE, Dashe J, Fréchet JMJ. Acetal-derivatized dextran: An acid-responsive biodegradable material for therapeutic applications. J Am Chem Soc. 2008;130:10494–5.
Abdelaziz HM, Gaber M, Abd-Elwakil MM, Mabrouk MT, Elgohary MM, Kamel NM, et al. Inhalable particulate drug delivery systems for lung cancer therapy: Nanoparticles, microparticles, nanocomposites and nanoaggregates. J Control Release. 2018;269:374–92.
Berkenfeld K, Lamprecht A, McConville JT. Devices for dry powder drug delivery to the lung. AAPS PharmSciTech. 2015;16:479–90.
Vehring R. Pharmaceutical particle engineering via spray drying. Pharm Res. 2008;25:999–1022.
Vehring R, Foss WR, Lechuga-Ballesteros D. Particle formation in spray drying. J Aerosol Sci. 2007;38:728–46.
Torrico Guzmán EA, Sun Q, Meenach SA. Development and evaluation of paclitaxel-loaded aerosol nanocomposite microparticles and their efficacy against air-grown lung cancer tumor spheroids. ACS Biomater Sci Eng. 2019;5:6570–80.
Shah NK, Gupta SK, Wang Z, Meenach SA. Enhancement of macrophage uptake via phosphatidylserine-coated acetalated dextran nanoparticles. J Drug Deliv Sci Technol. 2019;50:57–65.
Meenach SA, Anderson KW, Hilt JZ, McGarry RC, Mansour HM. High-performing dry powder inhalers of paclitaxel DPPC/DPPG lung surfactant-mimic multifunctional particles in lung cancer: physicochemical characterization, in vitro aerosol dispersion, and cellular studies. Ageing Int. 2014;15:1574–87.
Stocke NA, Meenach SA, Arnold SM, Mansour HM, Hilt JZ. Formulation and characterization of inhalable magnetic nanocomposite microparticles (MnMs) for targeted pulmonary delivery via spray drying. Int J Pharm. 2015;479:320–8.
Shepard KB, Adam MS, Morgen MM, Mudie DM, Regan DT, Baumann JM, et al. Impact of process parameters on particle morphology and filament formation in spray dried Eudragit L100 polymer. Powder Technol. 2020;362:221–30.
Darquenne C. Aerosol deposition in health and disease. J Aerosol Med Pulm Drug Deliv. 2012;25:140–7.
Darquenne C, Prisk GK. Aerosol deposition in the human respiratory tract breathing air and 80: 20 heliox. J Aerosol Med-Depos Clearance Eff Lung. 2004;17:278–85.
Jakaria MG, Sorkhdini P, Yang D, Zhou Y, Meenach SA. Lung Cell Membrane-Coated Nanoparticles Capable of Enhanced Internalization and Translocation in Pulmonary Epithelial Cells. Int J Pharm. 2021;613:121418.
Ramteke KH. Mathematical Models of Drug Dissolution: A Review. Acad J Pharm. 2014;3:388–96.
Freitas MN, Marchetti JM. Nimesulide PLA microspheres as a potential sustained release system for the treatment of inflammatory diseases. Int J Pharm. 2005;295:201–11.
Dash S, Murthy PN, Nath L, Chowdhury P. Kinetic modeling on drug release from controlled drug delivery systems. Acta Poloniae Pharmaceutica - Drug Res. 2010;67:217–23.
Suriyaprakash TNK, Prabu SL, Satyam T. In-vitro studies of diclofenac sodium controlled-release dosage from biopolymeric hydrophilic matrices. Ars Pharmaceutica. 2011;52:20–4.
Okunlola A, Adewusi SA. Development of theophylline microbeads using pregelatinized breadfruit starch (artocarpus altilis) as a novel co-polymer for controlled release. Adv Pharm Bull. 2019;9:93–101.
Ritger PL, Peppas NA. A simple equation for description of solute release II. Fickian and anomalous release from swellable devices. J Control Release. 1987;5:37–42.
Korsmeyer RW, Gurny R, Doelker E, Buri P, Peppas NA. Mechanisms of solute release from porous hydrophilic polymers. Int J Pharm. 1983;15:25–35.
Higuchi T. Mechanism of sustained action medication theoretical analysis of rate of release of solids matrics. J Pharm Sci. 1963;52:1145–9.
Koizumi T, Ueda M, Kakemi M, Kameda H. Rate of release of medicaments from ointment bases containing drugs in suspension. Chem Pharm Bull (Tokyo). 1975;23:3288–92.
Hixson AW, Crowell JH. Modeling and comparison of dissolution profiles. Ind Eng Chem. 1931;23:923–31.
Costa P. Modeling and comparison of dissolution profiles Paulo. Eur J Pharm Sci. 2001;13:123–33.
Haidl P, Heindl S, Siemon K, Bernacka M, Cloes RM. Inhalation device requirements for patients’ inhalation maneuvers. Respir Med. 2016;118:65–75.
Meenach SA, et al. Characterization and aerosol dispersion performance of advanced spray-dried chemotherapeutic PEGylated phospholipid particles for dry powder inhalation delivery in lung cancer. Eur J Pharm Sci. 2013;4:699–711.
Finlay W. The ARLA Respiratory Deposition Calculator. 2008. Available from: http://www.mece.ualberta.ca/arla/impactor_mmad_calculator.html.
Liu P. How to Perform a Standardized Tapped Density Test for Pharmaceutical How to Perform a Standardized Tapped Density Test for Pharmaceutical Powders ?. Bettersize Instruments Ltd. Pamphlet. 2021.
Da Silva ARP, Macedo TL, Coletta DJ, Feldman S, de Pereira MM. Synthesis, characterization and cytotoxicity of Chitosan/Polyvinyl alcohol/bioactive glass hybrid scaffolds obtained by Lyophilization. Revista Materia. 2016;21:964–73.
Islam MIU, Langrish TAG. The effect of different atomizing gases and drying media on the crystallization behavior of spray-dried powders. Drying Technol. 2010;28:1035–43.
Paudel A, Worku ZA, Guns JMS, Guns S, Van den Mooter G. Manufacturing of solid dispersions of poorly water soluble drugs by spray drying: Formulation and process considerations. Int J Pharm. 2013;453:253–84.
Raula J, Eerikäinen H, Kauppinen EI. Influence of the solvent composition on the aerosol synthesis of pharmaceutical polymer nanoparticles. Int J Pharm. 2004;284:13–21.
Shah NK, Wang Z, Gupta SK, Le Campion A, Meenach SA. Sustained release of a model water-soluble compound via dry powder aerosolizable acetalated dextran microparticles. Pharm Dev Technol. 2019;24:1133–43.
Littringer EM, Mescher A, Eckhard S, Schröttner H, Langes C, Fries M, et al. Spray drying of mannitol as a drug carrier—The impact of process parameters on product properties. Dry Technol. 2011;30:114–24. https://doi.org/10.1080/07373937.2011.620726.
Malamatari M, Charisi A, Malamataris S, Kachrimanis K, Nikolakakis I. Spray drying for the preparation of nanoparticle-based drug formulations as dry powders for inhalation. Processes. 2020;8(7):788.
Maas SG, Schaldach G, Littringer EM, Mescher A, Griesser UJ, Braun DE, et al. The impact of spray drying outlet temperature on the particle morphology of mannitol. Powder Technol. 2011;213:27–35.
Islam MIU, Langrish TAG. An investigation into lactose crystallization under high temperature conditions during spray drying. Food Res Int. 2010;43:46–56.
Martins KF, Messias AD, Leite FL, Duek EAR. Preparation and characterization of paclitaxel-loaded PLDLA microspheres. Mater Res. 2014;17:650–6.
Zhao X, Chen Q, Liu W, Li Y, Tang H, Liu X, et al. Codelivery of doxorubicin and curcumin with lipid nanoparticles results in improved efficacy of chemotherapy in liver cancer. Int J Nanomedicine. 2014;10:257–70.
Sun Y, Zhu L, Wu T, Cai T, Gunn EM, Yu L. Stability of amorphous pharmaceutical solids: Crystal growth mechanisms and effect of polymer additives. AAPS Journal. 2012;14:380–8.
Pandi P, Bulusu R, Kommineni N, Khan W, Singh M. Amorphous solid dispersions: An update for preparation, characterization, mechanism on bioavailability, stability, regulatory considerations and marketed products. Int J Pharm. 2020;586:1–28.
Fong SYK, Ibisogly A, Bauer-Brandl A. Solubility enhancement of BCS Class II drug by solid phospholipid dispersions: Spray drying versus freeze-drying. Int J Pharm. 2015;496(2):382–91
Pyo SH, Cho JS, Choi HJ, Han BH. Preparation and dissolution profiles of the amorphous, dihydrated crystalline, and anhydrous crystalline forms of paclitaxel. Dry Technol. 2007;25:1759–67.
Sreeharsha N, Hiremath JG, Al-Dhubiab BE, Meravanige G, Karnati RK, Attimarad M, et al. Fabrication of poly (Sebacic acid-co-ricinoleic-ester anhydride) with β-cyclodextrin-loaded doxorubicin implants and in vitro characterization. Indian J Pharm Educ Res. 2020;54:826–34.
Vasanthan N. Crystallinity determination of nylon 66 by density measurement and fourier transform infrared (FTIR) spectroscopy. J Chem Educ. 2012;89:387–90.
Bansal R, Singh R, Kaur K. Quantitative analysis of doxorubicin hydrochloride and arterolane maleate by mid IR spectroscopy using transmission and reflectance modes. BMC Chem. 2021;15(27):1.
Ciolacu D, Ciolacu F, Popa VI. Amorphous cellulose - Structure and characterization. Cellul Chem Technol. 2011;45:13–21.
Heidari M, Golenser J, Greiner A. Meeting the needs of a potent carrier for malaria treatment: Encapsulation of artemisone in poly(lactide-co-glycolide) micro- and nanoparticles. Part Part Syst Charact. 2022;39(2100152):1.
Shah NK, Gupta SK, Wang Z, Meenach SA. Enhancement of macrophage uptake via phosphatidylserine-coated acetalated dextran nanoparticles. J Drug Deliv Sci Technol. 2019;50:57–65.
Wang Z, Gupta SK, Meenach SA. Development and physicochemical characterization of acetalated dextran aerosol particle systems for deep lung delivery. Int J Pharm. 2017;525:264–74.
Shah NK, Wang Z, Gupta SK, Le Campion A, Meenach SA. Sustained release of a model water-soluble compound via dry powder aerosolizable acetalated dextran microparticles. Pharm Dev Technol. 2019;24(9):1133–1143.
Yamada Y. Dimerization of doxorubicin causes its precipitation. ACS Omega. 2020;5:33235–41.
Paarakh MP, Jose PANI, Setty CM, Peter GV. Release kinetics – concepts and applications. Int J Pharm Res Technol. 2019;8:12–20.
Siepmann J, Peppas NA. Higuchi equation: Derivation, applications, use and misuse. Int J Pharm. 2011;418:6–12.
Camelo SRP, Franceschi S, Perez E, Fullana SG, Ré MI. Factors influencing the erosion rate and the drug release kinetics from organogels designed as matrices for oral controlled release of a hydrophobic drug. Drug Dev Ind Pharm. 2016;42:985–97.
Mircioiu C, Voicu V, Anuta V, Tudose A, Celia C, Paolino D, et al. Mathematical modeling of release kinetics from supramolecular drug delivery systems. Pharmaceutics. 2019;11(3):40.
Martonen TB, Katz I. Deposition patterns of polydisperse aerosols within human lungs. J Aerosol Med-Depos Clearance Eff Lung. 1993;6:251–74.
Edwards DA. The macrotransport of aerosol particles in the lung: Aerosol deposition phenomena. J Aerosol Sci. 1995;26:293–317.
Eijkelboom NM, van Boven AP, Siemons I, Wilms PFC, Boom RM, Kohlus R, et al. Particle structure development during spray drying from a single droplet to pilot-scale perspective. J Food Eng. 2023;337:111222.
Thomas RJ. Particle size and pathogenicity in the respiratory tract. Virulence. 2013;4:847–58.
Champion JA, Walker A, Mitragotri S. Role of particle size in phagocytosis of polymeric microspheres. Pharm Res. 2008;25:1815–21.
Hao T. Tap density equations of granular powders based on the rate process theory and the free volume concept. Soft Matter. 2015;11:1554–61.
Chaurasiya B, Zhao YY. Dry powder for pulmonary delivery: A comprehensive review. Pharmaceutics. 2021;13:1–28.
Acknowledgements
The authors thank the Rhode Island Consortium of Nanoscience and Nanotechnology (RIN2) for SEM and XRD access.
Funding
Research was made possible through the Rhode Island Institutional Development Award (IDeA) Network of Biomedical Research Excellence from the National Institute of General Medical Sciences of the National Institutes of Health under grant number P20GM103430 and the National Institutes of Health under grant number R01HL148727.
Author information
Authors and Affiliations
Contributions
Ryan Ivone: conceptualization, writing (original draft preparation), literature search, data acquisition and analysis. Ana Karabots: conceptualization, writing (original draft preparation), data acquisition. Samantha Meenach: conceptualization, review, editing, supervision, resources, and funding.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ivone, R., Karabots, A. & Meenach, S.A. Development of Aerosol Dry Powder Chemotherapeutic-Loaded Microparticles for the Treatment of Lung Cancer. AAPS PharmSciTech 25, 42 (2024). https://doi.org/10.1208/s12249-024-02751-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-024-02751-8