Abstract
Although nasal inhalation products are becoming more and more important for the delivery of medicines, characterization of these products for quality control and assessment of bioequivalence is complicated. Most of the problems encountered are associated with the assessment of aerodynamic droplet/particle size distribution (APSD). The droplets produced by the various nasal devices are large, and for suspension products, individual droplets may contain multiple drug particles or none at all. Assessment of suspension products is further complicated by the presence of solid excipient particles. These complications make it imperative that the limitations of the instruments used for characterization as well as the underlying assumptions that govern the interpretation of data produced by these instruments are understood. In this paper, we describe various methodologies used to assess APSD for nasal inhalation products and discuss proper use, limitations, and new methodologies on the horizon.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inhaled medication delivery by the nasal route has been available to patients as a therapeutic modality for many years. However, there is increasing interest in this route of administration for a number of reasons, in particular for access to the brain via the olfactory bulb [1] and topical vaccine delivery to receptors in the nasal epithelium [2]. Hitherto, in the United States Pharmacopeia, the methodologies for assuring nasal product quality have been grouped with those for oral inhaled products [3, 4]. An argument can be made, however, for treating the assessment of size distribution from nasal products separately, as is done in the European Pharmacopoeia [5], given that the typical size range of the bulk of the droplets from nasal spray pumps is between 20 to around 200 µm, more than an order of magnitude larger than droplets from devices intended for oral delivery to the lungs since the nasal cavity is directly accessible by the spray [6]. These large droplets cannot be effectively size segregated by multi-stage inertial impaction, the mainstay method for assessing the aerodynamic particle size distribution of orally inhaled products. Alternative size-measurement methods are therefore necessary. However, the tail of the fine droplet component of the overall droplet size distribution from nasal sprays can potentially extend to sizes that could penetrate beyond the nasopharynx and reach the lungs. Such small droplets have been quantified separately from the bulk of the nasal spray using inertia-based methods that presently are not included in the pharmacopeial compendia. The purpose of this review is to raise awareness of how the drug product profile associated with entire size distribution from aqueous nasal products can be quantified. In view of the importance of this aspect in terms of defining the likely dose of medication delivered to the nasal space, other aspects of nasal product assessment, including delivered dose uniformity and spray geometry/pattern, are intentionally beyond scope, while recognizing the desirability of exploring the other important metrics in future similar review articles.
Droplet/particle size analysis of aqueous nasal sprays has long been a component of product development and routine quality control tests [7]. For suspension formulations, measurement is complicated because particles of the active pharmaceutical ingredient (API) are contained within these droplets, and it is possible that a given droplet may either not contain an API particle, or more than one particle as has been noted for suspension pressurized metered dose inhalers (pMDIs) [8]. Characterization of such products is further complicated by the presence of excipient particles [9]. As there are multiple techniques available for measuring droplet and particle size in aerosols, it is essential to be aware of both the underlying instrument method parameters and limitations when applying these measurements to nasal drug products.
Droplet and particle size measurements have also evolved as one of the indicators of in vitro bioequivalence (BE) [9]. For this reason, these techniques are the cornerstone of many regulatory BE guidances. Although laser diffraction (LD) is suggested as a method of choice for the determination of droplet size [9], in order to develop more discriminatory methods to support BE, particle size measurement methodology has evolved to include novel techniques, in particular, Morphology Directed Raman spectroscopy (MDRS) as well as other advanced laser-based techniques including Phase-Doppler Particle Analysis (PDPA) [10, 11].
At present, there is a lack of consistent technical guidance for the size assessment of droplets and API particles in nasal sprays; so, the purpose of this article is to highlight regulatory applications where such analyses are required. It is also necessary to present background material on these techniques in order to highlight their merits and limitations, as well as to identify developing analytical applications.
Regulation
USA
In the most recent guidance covering bioavailability (BA) and bioequivalence (BE) for nasal products [9], US FDA requests droplet size distribution obtained via LD (or appropriately validated alternative methodology) during the fully developed phase of the spray (Fig. 1). These measurements are to be performed at the beginning and end of unit lifetime and at two distances from the actuator orifice [7, 9]. A statistical evaluation (population bioequivalence, PBE) [12] is also required for the volume (mass)-weighted median diameter (D50) and span, defined as (D90 – D10)/D50, where D90 and D10 are the sizes corresponding to the 90th and 10th volume (mass) percentiles of the distribution. Importantly, the corresponding guideline from the European Medicines Agency (EMA) does not specify the time-portion of the plume to be analyzed [13].
Example laser diffraction output showing Transmission vs Time (y-axis) and Particle Diameter vs Time (z-axis). As the spray begins to form, Transmission levels decrease. As the Transmission level plateaus, the spray enters the fully developed or stable phase. (NextBreath, an Aptar pharma company, Baltimore, MD, used with permission)
The 2002 FDA nasal CMC guidance [7] indicates that droplet size by LD is an expected release and stability test. This guidance added the requirement to report the mass percentage of particles/droplets <10 µm diameter. Such small particles have the potential to penetrate beyond the nasopharyngeal region to reach the lungs where the API may not have an indication for use. In addition, delivering locally-acting API to the lungs can result in systemic absorption and potential adverse effects. It is important to note that one of the primary purposes of locally acting nasal products is to prevent systemic adverse effects, such as growth suppression in children caused by systemic absorption of corticosteroids.
Quantification of the drug mass contained in small particles or particle/droplet size distribution by cascade impaction (CI) is also requested for BE. However, such data need only be reported for the beginning life-stage. For nasal sprays, current CI methodology utilizes a 2-L or larger expansion chamber (Induction Port). The total API mass collected below the top stage of the CI should be reported in order to account for small particles that may be delivered to regions of the airway beyond the nose. The mass balance should also be reported as a percentage of label claim (LC). It is notable that neither the United States nor European Pharmacopeial compendia specify a method for quantifying the mass percentage of small particles from an aqueous nasal product.
Light (optical) microscopy is suggested as a suitable technique for estimating drug particle size distribution (PSD) in suspension products, including API-excipient aggregates. This determination should be carried out on samples taken directly from the bottle. PSD is still performed for CMC programs; however, in 2015, PSD by microscopy was removed from FDA-regulated nasal spray bioequivalence programs [14]. In addition, it should be noted that neither LD nor light microscopy directly provide aerodynamic PSD (APSD). Because light microscopy does not provide chemical identification of the size-characterized particles and since some nasal suspension products contain insoluble excipient particles as well as API-excipient agglomerates, it is recommended that “studies of nasal sprays include placebo product to provide an estimate of the occurrence of apparent drug particles (false positives)” [15].
In March 2015, the FDA Office of Generic Drugs began issuing Product Specific Guidance (PSG) documents for nasal products (Table I). These PSGs are updated periodically by FDA’s Office of Generic Drugs and major changes that apply globally to all similar products are typically referenced to the first product where mentioned (https://www.accessdata.fda.gov/scripts/cder/psg/index.cfm). For example, all nasal spray PSGs issued in or after September 2015 reference the first PSG for fluticasone propionate metered nasal spray [16]. The fluticasone propionate metered nasal spray PSG was last updated in 2023 [17].
The FDA has long recognized that, for nasal suspensions, “when the currently available technology cannot be acceptably validated” alternative methodology may be considered [7]. Specifically, with the product specific guidance (PSG) recommendation Draft Guidance on Triamcinolone Acetonide, metered nasal spray (October 2016) [11], the Office of Generic Drugs introduced the recently developed combination technique of MDRS [18, 19] as an alternative approach to the comparative clinical endpoint BE study. Although this newly commercialized technique also does not provide aerodynamic data, it affords chemical identification of the imaged particles such that API can be distinguished from excipient and agglomerates. Notably, all subsequent PSG recommendations or revisions also suggest this alternative approach. However, although this methodology provides chemical identification of aerosolized particles, the fixed resolution limit for optical microscopy (about 0.5 µm) renders it less than ideal for sizing submicron particles although this is not seen as a real problem for the characterization of nasal aerosols.
The current in vitro droplet size expectations from the FDA are presented in Table II.
EU, Canada, Australia, Brazil, and China
Nasal spray droplet size regulatory requirements for applications to the EMA [13], Health Canada [20], and Brazil [21] are mostly similar to those from the FDA. From a bioequivalence standpoint, only the FDA and ANVISA have issued official BE guidelines. However, the EMA Guideline on the Pharmaceutical Quality of Inhalation and Nasal Products notes that comparative data using a validated droplet method should be provided [13]. With respect to inhalation and nasal products, Australia has adopted the EMA guidelines [22]. At the time of this publication, China has also proposed draft bioequivalence guidelines. Table II highlights in vitro droplet size expectations from the major regulatory agencies.
Methodology
Cascade Impaction
Although CI is the recommended methodology for determination of the APSD for pharmaceutical aerosols from orally inhaled products [4, 21, 23, 24], this approach is less than ideal for such use with nasal sprays. This is so because most droplets/particles emitted by nasal spray devices are larger than the cut-off diameter (size at which 50% of incoming particles are collected) for the uppermost stage of the most used cascade impactors (i.e., about 9 µm aerodynamic diameter for the 8-stage Andersen Cascade Impactor (ACI) sampling at 28.3 Lpm). However, it is also important to assess the amount of excipients contained in small droplets (using API as a surrogate) as some of those compounds are not approved for pulmonary use and to assure that the amount is no greater for the test product than for the precursor product [9]. For these purposes, CI-based particle size analysis can be of benefit. A description of CI methodology that can be used as the basis for evaluating aqueous nasal products can be found in normative USP <601>. However, this chapter does not provide information concerning how to present the spray to the measurement apparatus, simply stating “In all cases and for all tests, prepare and test the spray as directed in the labeling and the instructions for use.” Informative USP <1603> provides useful background information by comprehensively covering good cascade impactor practices [25].
Some attempts have been made to circumvent this limitation by using modified ACIs designed for use at higher than standard flow rate (i.e., 60 or 90 L/min) but operated at 28.3 L/min to extend the functional size range to larger droplet sizes. For example, Doub and Adams looked at four different configurations of the ACI each with three different induction ports (inverted round glass flasks) and evaluated manual vs automated actuation [26, 27]. Use of a 1-L flask was shown to provide an inadequate path length for good development of the aerosol spray. Using either a 2-L or 5-L flask with automated actuation yielded more than 2½-times better precision relative to manual actuation [27]. Figure 2 shows the use of a 2-L glass flask with a SprayVIEW® NSX automatic actuator (Proveris Scientific, Hudson, MA). These authors, balancing measurement of total and small particle mass (SPM) deposition vs reproducibility, recommended the use of the 8-stage ACI at 28.3 lpm with a 2-L inlet as the optimal configuration. Garmise and Hickey took a similar approach with a modified version of the ACI (stages −2, −1, −0, filter) operated at 15 Lpm and calibrated this instrument using monodisperse particles in the 9–22 µm range to improve size-resolution of the emitted particles greater than 10 µm aerodynamic diameter [28].
The FDA recommends using automated actuation systems for BE assessments to decrease variability in drug delivery thus increasing the ability to differentiate between test and reference products [9]. This enhanced differentiation has been observed in several studies [29, 30]. However, the Guidance also recommends that actuation settings should be relevant to proper usage by the target patient population. Typically, the manufacturers of automated actuation devices can assist users to establish appropriate parameters [31]. For example, Spivey et al. found that by optimizing a set of eight parameters using an automated actuation device they could obtain D50 values within the expected 85 to 115% range of the average manual values [32]. Additional factors affecting droplet size are appropriate shaking and priming of nasal products prior to actuation. This precaution is especially important for thixotropic formulations which are able to change their physical properties under agitation, and thus optimize exposure of the product to the nasal mucosa [33].
A recent stimulus article published by the USP Expert Panel for Inhalation and Nasal Drug Products notes that the use of in vivo-predictive inlet ports in combination with simulated breathing patterns, rather than sampling the spray at one or more fixed flow rates, may be more predictive of delivery and deposition [34]. The authors of this article further recognized that there is no consensus on the most appropriate in vivo-predictive inlet port for development or routine testing. Examples of realistic or anatomical models are described as follows.
In vivo-Predictive Inlet Ports
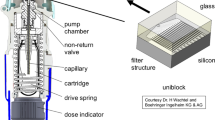
Glass inlet ports for nasal products can be as simple as inverted round flasks [27]. However, the use of more anatomically relevant devices such as models based on casts prepared at autopsy [35] have allowed more detailed identification of deposition sites such as separate determination of API within the anterior or posterior cavities of the nose. Williams et al. through the work of the European Pharmaceutical Aerosol Group (EPAG) have more recently reported collaborative studies looking at other simple inlets (both glass and metal) aimed specifically at evaluating those nasal spray components that have the potential to reach the lungs [36, 37]. Typically, regardless of material of construction, these inlets superficially resemble the USP induction port in design, but with an angle of 25° between the two sections allowing the nasal spray to be actuated in a more natural (i.e., per patient use) manner as opposed to horizontal actuation as is required when using the USP throat or other right-angle induction ports (Fig. 3). Ideally, the angle should be within the range specified in the patient use brochure. Initial findings testing an aqueous nasal spray were encouraging in terms of being able to detect azelastine, as model API, contained in small droplets [34]. However, further testing of the new inlet indicated [38] that more work needed to be done to mitigate drip-back out of the inlet to enable more reproducible determinations of the low-level emissions from currently marketed nasal spray products. In addition, EPAG are evaluating these inlet ports, using the Fast Screening Impactor (FSI) as an alternative to a full resolution impactor (Fig. 4). A new nasal inlet has recently been introduced by Baltz and Scherließ [39] (Fig. 5). This inlet, referred to as the Kiel Nasal Inlet (KNI), slips onto the end of the USP throat. The inlet is covered with a lid that has air inlet holes in line with the axis of the throat allowing for the constant airflow required for the target cascade impactor. The nozzle of the nasal spray is inserted through an elastic seal at the bottom of the inlet. The seal allows for insertion at any angle between vertical and 60°. An assessment of a sodium cromoglycate nasal inhaler looked promising as it resulted in a sub 10 µm fraction which was comparable across analysis using a FSI with a 10 micron cut-off plate, an NGI, and a reduced NGI. Additional KNIs have been sent to other laboratories for further testing and acquisition of performance data. The KNI was designed specifically for testing nasal sprays and additional evaluation will be required if it is to be applied for testing other dosage forms such as nasal aerosols or nasal powders.
Schematic for Kiel Nasal Inlet (Fig. 1 from reference 40 – used with permission)
An idealized nasal inlet, the Alberta Idealized Nasal Inlet (AINI), has been developed to mimic in vivo deposition by the group led by Finlay (Fig. 6) [40]. The AINI consists of four anatomical regions: vestibule, turbinates, olfactory, and nasopharynx. Chen et al. recently evaluated a commercially available nasal spray solution, suspension, and HFA-based nasal aerosol, comparing in vitro deposition with the AINI, over a range of actuation angles, to in vivo deposition by gamma scintigraphy [40, 41]. Their outcomes indicated that the AINI represented well the average in vivo deposition across this range of drug products (see Table III). The AINI predictions for deposition of solutions and suspensions were statistically comparable (Welch’s t-test, α = 0.05) to the previously obtained in vivo results. Predictive results for the nasal pMDI, particularly for the anterior region, were found to be especially poor but, because this device had a form factor much different from that of a traditional nasal spray, the appropriate range of angles is uncertain.
Recent CFD results from an FDA-commissioned study by Walenga et al. [42] seem to confirm this advantage., Xi et al. [43], via studies also funded by FDA, showed that anatomically accurate nasal casts along with digital simulation can be used to visualize regional deposition. However, another FDA funded project authored by Manniello et al. [44] showed that there is high inter-subject variability in posterior deposition (i.e., deposition in site of action), which was mainly due to the interaction of the device with the nose (i.e., the angle of insertion and the plume angle). This study involved 40 distinct anatomically accurate nasal casts with device specific instructions for patient use and sinusoidal breathing patterns. This high variability in posterior deposition is also reflected in similar studies by Alfaini et al. [45]. The large effect of plume angle on posterior deposition was shown earlier by Kolanjiyil et al. [46].
Currently, the use of anatomical nasal cavity-based models is expanding for the characterization of nasal drug products. Some commercial sources of relevant anatomical nasal models are those provided by the RDD Online organization (https://www.rddonline.com/rdd/rdd.php?sid=106”), and Copley Scientific Ltd. (https://www.copleyscientific.com/en/inhaler-testing/), although recent advances in 3D printing have enabled various research groups to create such models based on CT scans, while other groups have generated casts from cadavers, or other sources of anatomical data [47,48,49,50]. Williams and Suman have recently reviewed the use of such models for nasal drug development and the enhancement of understanding nasal drug delivery [47]. They made the important caution that to be considered valuable in the real-world sense, these in vitro methods need to be validated against in vivo results.
Optical/Imaging Techniques
By far, the most common technology for assessing particle/droplet size in nasal spray plumes is laser diffraction (LD), which the FDA has recommended for over 20 years [15]. LD is based on the angular scattering of coherent light which passes through the medium containing the particles or droplets of interest. LD is an ensemble technique, in that the size analysis takes place simultaneously with all the particles or droplets in the light pathway, in contrast to single particle light scattering methods (optical particle counters). The scattering angle is inversely proportional to the diameter of the particle and a mathematical model (Lorenz-Mie or Fraunhofer) is applied to interpret the angular light scattering signal to produce the size distribution that is weighted in terms of volume. It should be noted that exact solutions to the Lorenz-Mie theory, that incorporates the effect of refractive index of the particles/droplets on the light scattering profile, assumes particle sphericity. Sangolkar et al. pointed out the disadvantage that the refractive indices for both the particles and the media need to be known and that there must be a difference between them [51] and Luo et al. showed that the refractive index has a greater effect than does the assumption of sphericity [52]. Several thousand measurements per second are possible with current LD instruments such as the Spraytec (Malvern Panalytical, Malvern, UK) [53]. A major advantage of LD compared with other optical methods is that tens of thousands of particles can be measured. However, if the particle concentration is too high, secondary scattering can occur and must be avoided because the link between light scattering angle and particle size is lost. Sijs et al. found that in addition to being affected by the fitting model selected (due to droplet deviation from the expected shape), LD tends to overestimate the number of small droplets because the technique yields a continuously measured spatial distribution such that “small droplets traveling at a slow speed will appear at a higher concentration in the sample volume” [54]. Making the assumption that the measured particles are spherical becomes especially problematic when the aerosol contains small agglomerates and aggregates [55]. LD provides rapid analysis, especially compared to impaction methods, and does not require calibration as the light scattering-particle size relationship is absolute. Nevertheless, it requires rigorous method development and validation to ensure the resultant distribution is representative of the product.
A good example of the application of LD to size-characterize nasal sprays can be found in Kippax et al. [30]. Notably, Suman et al. showed that in vitro tests, such as LD-based droplet size measurement, are more sensitive to differences in performance between nasal spray pumps when compared to in vivo deposition in the human nasal cavity [56].
Major manufacturers of LD instrumentation are Malvern Panalytical and Sympatec GmbH (Clausthal-Zellerfeld, Germany). Bettersize Instruments Ltd. (Dandong, Liaoning, China) has recently introduced an instrument (model S3 plus: https://www.bettersizeinstruments.com/products/bettersizer-s3-plus/) that can perform simultaneous LD and particle/droplet image analysis (PDIA) measurements, but more details are needed on its performance compared with existing methods. The basic LD principles applied to nasal products can be found in USP Chapter <429>, but a more comprehensive explanation of the technique, including its limitations, is given in ISO 13320: 2020.
Additional efforts to circumvent limitations of using cascade impaction to characterize nasal spray drug products with respect to droplet/particle size and plume velocity have utilized various optical techniques other than LD. In a recent series of papers, Inthavong’s research group used data from PDIA and particle image velocimetry (PIV) measurements for nasal spray delivery device optimization [57,58,59]. In an earlier study, this group used PIV combined with computational fluid dynamics (CFD) to optimize nasal spray delivery [60]. An important result from Inthavong’s 2014 study with commercial nasal sprays is that, unless the inhalation is quite extreme, a user’s breathing profile is insufficient to have an influence on the measured droplet size distribution [57]. In a PDIA system, a high-power laser, used to illuminate the spray plume, is synchronized with a high-resolution CCD camera equipped with a long focal length microscope lens to obtain images of droplets and particles. Because the field of view (FOV) is small (approximately 3 mm × 4 mm), as many as 90 images (actuations) are required to image an entire plume out to 3 cm from the actuator. It is therefore reasonable to surmise that as many as 100 images may need to be collected for each FOV at each time point of plume life [58] in order to obtain an adequate statistical average.
Paired images (separated by as little as 100 ns) are recorded and later analyzed for PIV measurements, which typically make use of the same optical system as used for PDIA, to obtain an accurate velocity distribution. Renewed interest in PIV may be forthcoming as FDA has recently suggested use of this methodology to assess spray velocity for soft mist inhalers (SMIs, referred to as metered sprays for inhalation using FDA terminology) [61,62,63,64]. Despite the fact that plume velocity significantly impacts the efficacy and safety of nasal sprays by influencing the spray dispersion in the nasal cavity [7, 65,66,67], plume velocity characterization is not (yet) a requirement for nasal sprays. One drawback of PIV, similar to LD, is that the presence of excessively high concentrations of API particles in the measurement zone can compromise the accuracy, and result in invalid data [68]. Similar measurements can be made using plume geometry instrumentation [69].
Commercial sources for PDIA and PIV instruments are TSI Inc. (Shoreview, Minnesota, USA), Malvern Panalytical (Malvern, UK), and Oxford Lasers (Didcot, UK).
Phase- or (laser)-Doppler Anemometry (PDA or LDA) is another purely optical technique and can simultaneously provide both particle/droplet size and velocity measurements. PDA examines the scattered light from the probe volume formed by the intersection of two laser beams. Velocity is determined from intensity modulations within the probe volume and comparing the phase shift between the two beams. Analysis of the interference patterns in the scattered light created by these intersecting laser beams provides droplet size. The measured volume is extremely small (1.29 × 10−3 mm3) and the acceptance criteria have to be strict to ensure a valid light intensity profile at each detector, Therefore, mapping more than a few selected regions of the plume requires a very large number of measurements. As an example, Liu et al. showed that PDA could be used as a discriminating parameter for in vitro testing of nasal sprays [70] and later used this methodology to study the effect of actuation and formulation parameters on nasal spray velocity [66]. Hosseini et al. used PDA to characterize nasal sprays and study differences in dose and deposition patterns between adult and pediatric nasal airway models [71]. While regional deposition patterns were not statistically different between the pediatric and adult models, there were statistically different deposition amounts. Sijs et al. found that, for best results using PDA, “droplets need to be homogeneous, transparent, and spherical.” Non-spherical droplets tend to be slightly undersized by PDA which also sees air bubbles within droplets as small droplets [54]. The particle trajectory criteria for a successful transition across the interference fringes set up by the intersecting light pathways are severe and may be a limiting factor for this technique as it can be difficult to assure that the sampled particles/droplets are representative [72].
Among the commercial manufacturers of PDA instrumentation are Dantec (Skovlunde, Denmark) and TSI.
Chemically Distinctive Imaging
A major disadvantage of the optical/imaging methodologies discussed above is that, although particle/droplet size can be measured with varying degrees of precision and accuracy, there is no mechanism to provide the identity of those particles suspended within the sprayed droplets. Nasal spray suspension products contain solid excipients in addition to the API, so some means is essential to be able to differentiate and quantify API separately from excipient(s) and from API-excipient aggregates. One way to accomplish this goal is to use a spectroscopic technique to provide the chemical identity of each particle. An early attempt to address this problem involved wide-field Raman micro-spectroscopy (Raman chemical imaging, RCI). For RCI, a relatively low power laser light source is used to illuminate the sample and the scattered light is magnified onto a two-dimensional CCD detector. Typically, liquid-crystal tunable filters are used for wavelength selection. Optical (i.e., white light) images are also acquired which are fused with the Raman images, enabling differentiation between drug aggregates and individual particles. A proof-of-concept study conducted using in-house prepared beclomethasone dipropionate nasal sprays showed promise that RCI could provide PSD information for drug and drug aggregates [73]. The wide-field chemical imaging approach used in this study exhibits inherently higher spatial and spectral resolution than do other RCI techniques such as point mapping and line scanning. However, this methodology has not yet been widely adopted, likely because the instrumentation requires extensive operator training linking image and Raman spectra interpretation to make meaningful measurements.
A somewhat different version of Raman micro-spectroscopy has emerged in recent years and has gained sufficient favor within the FDA [18] that, going forward, it will possibly become the method of choice for particle sizing. Note that LD will remain as a routine quality control test. This methodology, called Morphologically-Directed Raman Spectroscopy (MDRS), first appeared in an FDA PSG for triamcinolone acetonide metered nasal spray (OTC), issued in October 2016 [11]. MDRS combines automated imaging and Raman spectroscopy, where the individual particles are first identified using an integrated microscope, and then Raman spectra are collected for each particle. The correlations between the spectral information and the morphological data collected for individual particles provide insight into particle morphological characteristics (size and shape) and chemical properties. Morphological characteristics and the upper and lower limits associated with those parameters need to be optimized for best differentiation between API and excipients.
Microscopic images (white light) of all particles in multiple FOVs are obtained for the target formulation dispersed on a quartz or metalized microscope slide using a computer-controlled stage for the first stage of a measurement by MDRS. Sample preparation is somewhat complicated by the joint requirements that the dispersed formulation needs to remain in a liquid state, but the particles must remain immobile. Image analysis algorithms are then applied to all images to define a subset of particles based on specific shape and size parameters. For example, particles might be selected that have a specific circularity and/or convexity within a certain size range. These parameters are chosen to select for the desired particle type, typically the API. Raman spectroscopy is then applied to the defined subset of particles. Typically, a full range spectrum is obtained for each particle. Because Raman signals are quite weak, this process can require as much as 20–30 s per particle such that acquisition of spectra for several thousand particles typically requires an over-night measurement. However, optimization of the many parameters (Table IV), will require numerous experiments encompassing several days. The optimized parameters will be very much product specific and, if cohesive aggregates are to be considered, much longer times will be required for optimization and validation. Spectral results are processed using accepted spectroscopic methods and then matched against library spectra obtained using pure substances in a dry state. While there is currently no specific FDA guidance on MDRS, scientists from this regulatory body have published multiple papers on analytical method development and other considerations for this technique [10, 19].
Summary
LD and impaction-based methodologies have a long history of use in pharmaceutical aerosol and nasal product development, as both these techniques are required for routine quality control testing. As regulatory bodies and industry look to establish a link between these in vitro tests and in vivo outcomes, new approaches such as MDRS have been adopted.
Debate over utilization and standardization of new technology and biorelevant methodologies, such as realistic inlets, is ongoing in an effort to delineate in vitro-in vivo correlations (IVIVC). Applications of LD and cascade impaction are evolving. For example, particle/droplet size data can be incorporated into physiologically based pharmacokinetic models (PBPK). Understanding the kinetics of particle dissolution, which relates partly to particle size, has both implications for local and systemic absorption. A recent study by Hochhaus et al. showed good correlation between PK and dissolution results [74]. Future discussions will determine which of these new approaches becomes a recognized standard practice.
Data Availability
No original/author generated data are included in this paper. For any data derived from previous publications, an appropriate citation is provided.
References
Martin V, Hoekman J, Aurora SK, Shrewsbury SB. Nasal delivery of acute medications for migraine: the upper versus lower nasal space. J Clin Med. 2021;10(11):2468. https://doi.org/10.3390/jcm10112468.
Cahn D, Amosu M, Maisel K, Duncan GA. Biomaterials for intranasal and inhaled vaccine delivery. Nat Rev Bioeng. 2023;1(2):83–4. https://doi.org/10.1038/s44222-022-00012-6.
US Pharmacopeial Convention. United States Pharmacopeia USP 37-NF 32_S1, General Chapter 5: Inhalation and nasal drug products-general information and product quality tests. 2014. Rockville, MD, USA. (http://www.uspnf.com/uspnf/pub/data/v37321/usp37nf32s1_c5.xml)
United States Pharmacopeial Convention. United States Pharmacopeia USP 42–NF37 , Chapter 601, Aerosols, nasal sprays, metered-dose inhalers and dry powder inhalers: 2018, Rockville, MD,USA.
EDQM Council of Europe, European Pharmacopia Section 0676, Nasal Preparations, Nasalia. Strausbourg, France, 2021.
Copley Scientific Limited. In: Driving results in inhaler testing. (2023) Available at: https://www.calameo.com/copleyscientific/read/006693220fa76cad62867. Accessed: 5/1/2023.
United States Food and Drug Administration. Nasal spray and inhalation solution, suspension, and spray drug products — chemistry, manufacturing, and controls documentation [Internet]. Silver Spring, MD: United States Food and Drug Administration; July 2002 Available from: https://www.fda.gov/media/70857/download. Accessed 26 Sep 2023.
Stein SW. Estimating the number of droplets and drug particles emitted from MDIs. AAPS PharmSciTech. 2008;9(1):112–5. https://doi.org/10.1208/s12249-007-9006-8.
United States Food and Drug Administration. Bioavailability and bioequivalence studies for nasal aerosols and nasal sprays for local action [Internet]. Silver Spring, MD: United States Food and Drug Administration; April 2, 2003 Available from: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM070111.pdf.
Thomas BJ, Absar M, Delvadia R, Conti DS, Witzmann K, Guo C. Analytical method development for characterizing ingredient-specific particle size distributions of nasal spray suspension products. J Pharm Sci. 2021;110(7):2778–88. https://doi.org/10.1016/j.xphs.2021.03.005.
United States Food and Drug Administration. Draft guidance on triamcinolone acetonide metered nasal spray [Internet]. Silver Spring, MD: United States Food and Drug Administration; Recommended Oct 2016; Revised Feb 2019, Jun 2020 Available from: https://www.accessdata.fda.gov/drugsatfda_docs/psg/PSG_020468.pdf. Accessed 5 Jun 2020.
United States Food and Drug Adminstration. Draft guidance on budesonide inhalation suspension [Internet]. Silver Spring, MD: United States Food and Drug Adminstration; Recommended Sep. 2012 Available from: https://www.accessdata.fda.gov/drugsatfda_docs/psg/Budesonide_Inhalation_Sus_20929_RC_09-12.pdf. Accessed 29 Mar 2016.
EMEA. Guideline on the pharmaceutical quality of inhalation and nasal products [Internet]. London: EMEA; June 21, 2006 [cited 13 Aug 2018]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500003568.pdf. Accessed 6 Jul 2010
United States Food and Drug Administration. Draft Guidance on Mometasone Furoate Monohydrate Metered Nasal Spray [Internet]. Silver Spring, MD: United States Food and Drug Administration; Recommended Sept 2015, Revised Feb 2019. Available from https://www.accessdata.fda.gov/drugsatfda_docs/psg/Mometasone%20furoate%20nasal%20spray%20NDA%20020762%20RV%2002-2019.pdf#:~:text=Draft%20Guidance%20on%20Mometasone%20Furoate%20Monohydrate%20This%20draft,is%20not%20binding%20on%20FDA%20or%20the%20public. Accessed 26 Sep 2023.
United States Food and Drug Administration. Draft guidance: bioavailability and bioequivalence studies for nasal aerosols and nasal sprays for local action [Internet]. Silver Spring, MD: United States Food and Drug Administration; April 2003. Available from http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM070111.pdf. Accessed Apr 2023.
United States Food and Drug Administration. Draft guidance on fluticasone propionate metered nasal spray – OTC [Internet]. Silver Spring, MD: United States Food and Drug Administration; Recommended Sep 2015; Revised May 2021. Available at https://www.accessdata.fda.gov/drugsatfda_docs/psg/PSG_205434.pdf. Accessed 26 Sep 2023.
United States Food and Drug Administration. Draft guidance on fluticasone propionate metered nasal spray, 0.05 mg/spray [Internet]. Silver Spring, MD: United States Food and Drug Administration; Recommended Sep 2015; Revised Feb 2019, Jun 2020, May 2023. Available at https://www.accessdata.fda.gov/drugsatfda_docs/psg/PSG_020121.pdf. Accessed 26 Sep 2023.
Li B. FDA embraces emerging technology for bioequivalence evaluation of locally acting nasal sprays. FDA/CDER SBIA Chronicles. White Oak, MD: US Food and Drug Administration; 2016. Available at https://wayback.archive-it.org/7993/20170113101532/; http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/SmallBusinessAssistance/UCM502012.pdf. Accessed 26 Sep 2023.
Liu Q, Absar M, Saluja B, Guo C, Chowdhury B, Lionberger R, et al. Scientific considerations for the review and approval of first generic mometasone furoate nasal suspension spray in the United States from the bioequivalence perspective. AAPS J. 2019;21(2):14. https://doi.org/10.1208/s12248-018-0283-9.
Health Canada. Guidance for industry: pharmaceutical quality of inhalation and nasal products [Internet]. Ottawa: Health Canada; October 1, 2006 Available from: http://www.hc-sc.gc.ca/dhp-mps/alt_formats/hpfb-dgpsa/pdf/prodpharma/inhalationnas-eng.pdf. Accessed 4 Apr 2013.
Brazilian Health Surveillance Agency (ANVISA). 2019. Normative Instruction No. 33, 16 April 2019. In Vitro Performance Tests for OINDP. Available at https://antigo.anvisa.gov.br/en/english.
Therapeutic Goods Administration, AU. Guidance 19: inhalation and nasal spray registered medicines [Internet]. Woden ACT: Therapeutic Goods Administration, AU; Version1.0, August 2013 [cited 25 Nov 2019]. Available from: https://www.tga.gov.au/file/5212/download.
United States Food and Drug Administration. Draft guidance for industry: metered dose inhaler (MDI) and dry powder inhaler (DPI) products - quality considerations [Internet]. Silver Spring, MD: United States Food and Drug Administration; Revised April 2018. Available from: https://www.fda.gov/media/70851/download. Accessed 26 Sep 2023.
Therapeutic Goods Administration, AU. Inhalation and nasal spray registered medicines [Internet]. Woden ACT: Therapeutic Goods Administration, AU; October 2019.
US Pharmacopeial Convention. United States Pharmacopeia. Good cascade impactor practices, Chapter 1603: good cascade impactor practices: 2021, Rockville, MD, USA. Available at https://online.uspnf.com/uspnf/document/1_GUID-7054DEA7-8615-44AE-B612-960462CB4BCC_3_en-US.
Doub WH, Adams WP. Measurement of drug in small particles/droplets from aqueous nasal spray by cascade impaction. Poster session T3415 presented at Annual Meeting of the American Association of Pharmaceutical Scientists; Nov. 12, 2002. Toronto, Ontario.
Doub W, Adams W, Wokovich A, Black J, Shen M, Buhse L. Measurement of drug in small particles from aqueous nasal sprays by Andersen Cascade Impactor. Pharm Res. 2012;29(11):3122–30. https://doi.org/10.1007/s11095-012-0804-7.
Garmise RJ, Hickey AJ. Calibration of the Andersen cascade impactor for the characterization of nasal products. J Pharm Sci. 2008;97(8):3462–6. https://doi.org/10.1002/jps.21267.
Chauhan H, Liao LL. Reducing variability in test results for OINDPs with automated actuation. On Drug Delivery. 2018. p. 52–7. Available at https://www.ondrugdelivery.com/reducing-variability-in-test-results-for-oindps-with-automated-actuation/. Accessed 26 Sep 2023.
Kippax PG, Krarup H, Suman JD. Applications for droplet sizing: manual versus automated actuation of nasal sprays. Pharm Tech. 2004:30, 2, 4, 6, 8, 40. Available at https://cdn.sanity.io/files/0vv8moc6/pharmtech/f69a494e142d8f7450ca15a24793462c70299549.pdf/article-112226.pdf. Accessed 26 Sep 2023.
Guo C, Doub WH. The influence of actuation parameters on in vitro testing of nasal spray products. J Pharm Sci. 2006;95(9):2029–40. https://doi.org/10.1002/jps.20678.
Spivey R, Ware L, Hamby K. Comparative analysis of manual versus automated actuation parameters for droplet size determinations by Laser Diffraction for Spray Devices. 2008.
Koźmiński M, Kupczyk M. Thixotropy of nasal medications — its role in clinical practice. Adv Respir Med. 2015;83(2):157–63. https://doi.org/10.5603/PiAP.2015.0025.
USP Expert Panel. Testing the in vitro product performance of inhalation and nasal drug products: views of the USP expert panel. Pharmaceutical Forum. 2022;48(5):11.
Hallworth GW, Padfield JM. A comparison of the regional deposition in a model nose of a drug discharged from metered aerosol and metered-pump nasal delivery systems. J Allergy Clin Immunol. 1986;77(2):348–53.
Williams G, Bickmann D, Schiewe J, Hauviller C, Blatchford C, Doub W, et al. Towards standardizing methodology for quantifying the fine particle mass (dose) of active pharmaceutical ingredient (api) from nasal products (nps). J Aerosol Med Pulm Drug Deliv. 2014;27(4):A14.
Williams G, Blatchford C, Mitchell JP. Evaluation of nasal inlet ports having simplified geometry for the pharmacopeial assessment of mass fraction of dose likely to penetrate beyond the nasopharynx: a preliminary investigation. AAPS PharmSciTech. 2018;19(8):3723–33. https://doi.org/10.1208/s12249-018-1179-9.
Baltz N, Scherließ R. Assessment of sub-10 micron mass fraction in nasal products: method considerations. Drug Delivery to the Lungs. Edinburgh: Aerosol Society; 2022.
Baltz N, Scherließ R. Assessment of nasal products – proposing a new inlet. Drug Delivery to the Lungs. Edinburgh; Aerosol Society 2022.
Chen JZ, Finlay WH, Martin AR. In vitro regional deposition of nasal sprays in an idealized nasal inlet: comparison with in vivo gamma scintigraphy. Respiratory Drug Delivery 2022. Orlando: RDD Online; 2022.
Chen JZ, Kiaee M, Martin AR, Finlay WH. In vitro assessment of an idealized nose for nasal spray testing: comparison with regional deposition in realistic nasal replicas. Int J Pharm. 2020;582:119341. https://doi.org/10.1016/j.ijpharm.2020.119341.
Walenga R, Dhapare S, Newman B, Babiskin A, Zhao aL. In silico and experimental methods to support generic nasal drug product (NDP) development. Respiratory Drug Development 2021. Virtual; 2021.
Xi J, Wang Z, Nevorski D, White T, Zhou Y. Nasal and olfactory deposition with normal and bidirectional intranasal delivery techniques: in vitro tests and numerical simulations. J Aerosol Med Pulm Drug Deliv. 2017;30(2):118–31. https://doi.org/10.1089/jamp.2016.1295.
Manniello MD, Hosseini S, Alfaifi A, Esmaeili AR, Kolanjiyil AV, Walenga R, et al. In vitro evaluation of regional nasal drug delivery using multiple anatomical nasal replicas of adult human subjects and two nasal sprays. Int J Pharm. 2021;593:120103. https://doi.org/10.1016/j.ijpharm.2020.120103.
Alfaifi A, Hosseini S, Esmaeili AR, Walenga R, Babiskin A, Schuman T, et al. Anatomically realistic nasal replicas capturing the range of nasal spray drug delivery in adults. Int J Pharm. 2022;622:121858. https://doi.org/10.1016/j.ijpharm.2022.121858.
Kolanjiyil A, Hosseini S, Alfaifi A, Hindle M, Golshahi L, Longest P. How spray metric variability impacts the initial deposition of nasal sprays. In Dalby RN, Peart J, Suman JD, Young PM, Traini D (eds) Respiratory Drug Delivery 2021. Richmond, VA: RDD Online; 2021. Available at https://www.rddonline.com/rdd/rdd.php?sid=103. Accessed 26 Sep 2023.
Williams G, Suman JD. In vitro anatomical models for nasal drug delivery. Pharmaceutics. 2022;14(7):1353. https://doi.org/10.3390/pharmaceutics14071353.
Howe C, Momin MAM, Bass K, Aladwani G, Bonasera S, Hindle M, et al. In vitro analysis of nasal interface options for high-efficiency aerosol administration to preterm infants. J Aerosol Med Pulm Drug Deliv. 2022;35(4):196–211. https://doi.org/10.1089/jamp.2021.0057.
Chari S, Sridhar K, Kleinstreuer C. Effects of subject-variability on nasally inhaled drug deposition, uptake, and clearance. J Aerosol Sci. 2022;165:106021. https://doi.org/10.1016/j.jaerosci.2022.106021.
Golshahi L, Hosseini S. Intranasal filtration of inhaled aerosol in human subjects as a function of nasal pressure drop. J Aerosol Med Pulm Drug Deliv. 2019;32(1):13–23. https://doi.org/10.1089/jamp.2018.1476.
Sangolkar SS, Adhao VS, Mundhe DG, Sawarkar HS. Particle size determination of nasal drug delivery system: a review. Int J Pharm Sci Rev Res. 2012;17(1):66–73.
Luo S, Weinell CE, Kiil S. Laser diffraction measurements of pigment size distributions of coatings and mill bases: implications of dilution medium and dispersion process parameters. J Coat Technol Res. 2023. https://doi.org/10.1007/s11998-022-00742-7.
Mitchell JP, Nagel MW, Nichols S, Nerbrink O. Laser diffractometry as a technique for the rapid assessment of aerosol particle size from inhalers. J Aerosol Med. 2006;19(4):409–33.
Sijs R, Kooij S, Holterman HJ, Zande Jvd, Bonn D. Drop size measurement techniques for sprays: comparison of image analysis, phase Doppler particle analysis, and laser diffraction. AIP Adv. 2021;11(1):015315. https://doi.org/10.1063/5.0018667.
de Boer AH, Gjaltema D, Hagedoorn P, Frijlink HW. Characterization of inhalation aerosols: a critical evaluation of cascade impactor analysis and laser diffraction technique. Int J Pharm. 2002;249(1–2):219–31. https://doi.org/10.1016/S0378-5173(02)00526-4.
Suman JD, Laube BL, Lin T-c, Brouet G, Dalby R. Validity of in vitro tests on aqueous spray pumps as surrogates for nasal deposition. Pharm Res. 2002;19(1):1–6.
Inthavong K, Fung M, Tong X, Yang W, Tu J. High resolution visualization and analysis of nasal spray drug delivery. Pharm Res. 2014;31(8):1930–7. https://doi.org/10.1007/s11095-013-1294-y.
Inthavong K, Fung MC, Yang W, Tu J. Measurements of droplet size distribution and analysis of nasal spray atomization from different actuation pressure. J Aerosol Med Pulm Drug Deliv. 2015;28(1):59–67. https://doi.org/10.1089/jamp.2013.1093.
Shrestha K, Strien J, Singh N, Inthavong K. Primary break-up and atomization characteristics of a nasal spray. PLOS ONE. 2020;15:e0236063. https://doi.org/10.1371/journal.pone.0236063.
Inthavong K, Tian ZF, Tu JY, Yang W, Xue C. Optimising nasal spray parameters for efficient drug delivery using computational fluid dynamics. Comput Biol Med. 2008;38(6):713–26. https://doi.org/10.1016/j.compbiomed.2008.03.008.
United States Food and Drug Administration. Draft guidance on tiotropium bromide, metered inhalation spray [Internet]. Silver Spring: United States Food and Drug Administration; Recommended Nov 2020. Available at https://www.accessdata.fda.gov/drugsatfda_docs/psg/PSG_021936.pdf. Accessed 26 Sep 2023.
United States Food and Drug Administration. Draft guidance on olodaterol hydrochloride metered inhalation spray [Internet]. Silver Spring, MD: United States Food and Drug Administration; Recommended Aug 2021. Available at https://www.accessdata.fda.gov/drugsatfda_docs/psg/PSG_203108.pdf. Accessed 26 Sep 2023.
United States Food and Drug Administration. Draft guidance on albuterol sulfate; ipratropium bromide metered inhalation spray [Internet]. Silver Spring. MD: United States Food and Drug Administration; Recommended Aug 2021. Available at https://www.accessdata.fda.gov/drugsatfda_docs/psg/PSG_021747.pdf. Accessed 26 Sep 2023.
United States Food and Drug Administration. Draft guidance on olodaterol hydrochloride; tiotropium bromide metered inhalation spray [Internet]. Silver Spring, MD: United States Food and Drug Administration; Recommended July 2021 Silver Spring. Available at https://www.accessdata.fda.gov/drugsatfda_docs/psg/PSG_206756.pdf. Accessed 26 Sep 2023.
Seifelnasr A, Talaat M, Ramaswamy P, Si XA, Xi J. A supine position and dual-dose applications enhance spray dosing to the posterior nose: paving the way for mucosal immunization. Pharmaceutics. 2023;15(2):359. https://doi.org/10.3390/pharmaceutics15020359.
Liu X, Doub WH, Guo C. Assessment of the influence factors on nasal spray droplet velocity using phase-doppler anemometry (PDA). AAPS PharmSciTech. 2011;12(1):337–43. https://doi.org/10.1208/s12249-011-9594-1.
Kolanjiyil AV, Hosseini S, Alfaifi A, Hindle M, Golshahi L, Longest PW. Importance of cloud motion and two-way momentum coupling in the transport of pharmaceutical nasal sprays. J Aerosol Sci. 2021;156:105770. https://doi.org/10.1016/j.jaerosci.2021.105770.
Inthavong K, Yang W, Fung MC, Tu JY. External and near-nozzle spray characteristics of a continuous spray atomized from a nasal spray device. Aerosol Sci Technol. 2012;46(2):165–77. https://doi.org/10.1080/02786826.2011.617793.
Liao L, Ramos K, Farina D. A novel characterization of emitted aerosol velocity profiles from metered dose and soft mist inhaler. Drug Delivery to the Lungs, 30, 287-290, Edinburgh; 2019.
Liu X, Doub WH, Guo C. Evaluation of droplet velocity and size from nasal spray devices using phase Doppler anemometry (PDA). Int J Pharm. 2010;388(1–2):82–7. https://doi.org/10.1016/j.ijpharm.2009.12.041.
Hosseini S, Wei X, Wilkins JV Jr, Fergusson CP, Mohammadi R, Vorona G, et al. In vitro measurement of regional nasal drug delivery with Flonase,® Flonase® Sensimist,™ and MAD Nasal™ in anatomically correct nasal airway replicas of pediatric and adult human subjects. J Aerosol Med Pulm Drug Deliv. 2019;32(6):374–85. https://doi.org/10.1089/jamp.2019.1523.
Bachalo WD. Experimental methods in multiphase flows. Int J Multiph Flow. 1994;20:261–95. https://doi.org/10.1016/0301-9322(94)90075-2.
Doub W, Adams W, Spencer J, Buhse L, Nelson M, Treado P. Raman chemical imaging for ingredient-specific particle size characterization of aqueous suspension nasal spray formulations: A Progress Report. Pharm Res. 2007;24(5):934–45. https://doi.org/10.1007/s11095-006-9211-2.
Hochhaus G, Amini E, Berger S, Shur J, Kurumaddali A, Schilling U, et al. Evaluating particle size differences of suspension-based nasal sprays through in vitro and pharmacokinetic approaches. In: Dalby RN, Peart J, Suman JD, Young PM, Traini D, Watts A (eds) Respiratory Drug Delivery, Champions Gate, FL 2022. RDD Online, Richmond, VA. 2022. Available at https://www.rddonline.com/rdd/rdd.php?sid=103. Accessed 26 Sep 2023.
Acknowledgements
The authors wish to acknowledge the support of the IPAC-RS Board of Directors and the members of the Cascade Impaction Working Group.
Funding
This work was sponsored by the International Pharmaceutical Aerosol Consortium on Regulation and Science (IPAC-RS).
Author information
Authors and Affiliations
Contributions
William H. Doub: conceptualization; writing—co-wrote original draft, review and editing; supplied specialized knowledge regarding certain topics.
Julie M. Suman: writing—co-wrote original draft, review and editing; supplied specialized knowledge regarding certain topics; supplied several figures with descriptors.
Mark Copley: writing—review and editing; supplied specialized knowledge regarding certain topics.
Adrian P. Goodey: writing—review and editing; supplied specialized knowledge regarding certain topics.
Sana Hosseini: writing—review and editing; supplied specialized knowledge regarding certain topics; supplied several figures with descriptors.
Jolyon P. Mitchell: writing—review and editing; supplied specialized knowledge regarding certain topics.
Corresponding author
Ethics declarations
Conflict of Interest
Apart from MC, who is the CEO of a company that manufactures inhaler test equipment, there are no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Doub, W.H., Suman, J.M., Copley, M. et al. Laboratory Performance Testing of Aqueous Nasal Inhalation Products for Droplet/Particle Size Distribution: an Assessment from the International Pharmaceutical Aerosol Consortium on Regulation and Science (IPAC-RS). AAPS PharmSciTech 24, 208 (2023). https://doi.org/10.1208/s12249-023-02665-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-023-02665-x