Abstract
A severe form of autoimmune-mediated inflammatory bowel disease (IBD) is termed as ulcerative colitis (UC) which ultimately results in significant mucosal damage and ulceration. Herbal remedies may be employed as an alternative for treatment of UC instead of conventional medications such as Sulfasalazine. Promising natural remedies for the treatment of IBD, including colitis, are propolis extract (PP) and thymoquinone (TQ). This study is aimed at assessing the potential of liposomal formulations of TQ and Egyptian PP in combination therapy on improving their therapeutic efficacy against ulcerative colitis in order to maximize the potential of their beneficial clinical effects. Clinical, biochemical, and histological evaluations of colonic mucosal damage and inflammation were evaluated. The results exhibited a significant increase in tissue MDA, TNFα, and nitrite levels with activation of caspase-3 in the acetic acid-induced colitis group, which is predominantly downregulated in the treatment groups. The prepared formulations of TQ and PP revealed liposomal vesicles in a nanoscale size (192 ± 20.3 and 98.2 ± 20.3 nm, respectively) and accepted stability indicated with a zeta potential of 19.3 ± 0.11 and 17.1 ± 0.25 mV, respectively. They showed an entrapment efficiency of 85.3 ± 12.6% and 69.3 ± 11.8%, respectively. At comparable doses, combination therapy with thymoquinone liposomes and propolis liposomes considerably outperformed free TQ and free PP in reducing inflammation of UC as shown in the present study by clinical, biochemical, and histological evaluations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory bowel disease (IBD) is a prevalent chronic inflammatory disorder of the GIT. Various etiological factors including hereditary, immunological, and ecological have been associated with its pathophysiology. Crohn’s disease (CD) and ulcerative colitis (UC) are two major subdiseases of IBD. UC involves only the colon and rectum [1]. Certain data suggest that IBD in humans is a one of the most common risk factors leading to colorectal cancer and potentially fatal respiratory or circulatory complications [2].
There is still much to learn about UC’s pathogenic mechanisms and etiology. The pathogenesis of UC is believed to include a number of factors, including an erratic immunological response [3]. Recent evidence has shown that pivotal intracellular processes, such as oxidative stress, epithelial barrier disturbance, accelerated epithelial apoptotic cell death, and suppression of immune and inflammatory cell apoptosis, are intimately connected to the immunological anomaly caused by UC and the subsequent colonic tissue damage. As a result, apoptosis is crucial for controlling intestinal epithelial homeostasis [4].
Numerous mechanisms, such as neutrophil infiltration, excessive generation of proinflammatory mediators, and increased reactive oxygen species (ROS), are thought to play a role in its pathogenesis. Tumor necrosis factor alpha (TNF-α) is an essential proinflammatory mediator involved in the pathogenesis of IBD [5]. TNF-α is a pleiotropic proinflammatory cytokine that is involved in a variety of cellular functions, including cell proliferation, survival, and death. Additionally, various inflammatory pathways, such as cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (iNOS) pathways, are mediated by TNF-α signaling. The large intestine mucosa is harmed by the activation of COX-2 and inducible nitric oxide synthase (iNOS), which increases free radical production while suppressing the anti-oxidative system. In fact, the intestinal mucosa’s defense mechanism is impacted by the excessive formation of ROS and nitrogen metabolites [6].
The most widely used medication for the treatment of IBD, including UC, is Sulfasalazine, which aims to reduce mucosal inflammation, complications, and disease recrudescence. Regrettably, since they require lengthy usage and can cause drug intolerance, adverse drug responses, and allergic reactions, the present medications are not much efficient. Therefore, natural remedies and medications derived from plants may be an alternative for the management of UC since, in conventional medicine, these are being given much consideration due to their few side effects, low cost, and the fact that the majority of individuals throughout the world still believe them. Several natural products, involving aloe vera, liquorice, turmeric, curcumin, Zingiber officinale, and green tea, have been reported to have an impact on UC in numerous trials [7].
Propolis is a waxy substance formed by bees through mixing exudates of plants with their saliva and beeswax [8]. Propolis extract is proposed as a promising natural product for controlling IBD including colitis [9, 10]. Results showed that administration of Korean propolis minimized the Dextran Sulfate Sodium (DSS)-induced colitis in mice in a dose-dependent style [9]. Other studies revealed the impact of oral administration of rats of either Brazilian or Chinese propolis on the prevention of DSS-induced colitis in rats [11, 12]. Thymoquinone, the main active constituent of Nigella sativa, is another natural component with remarkable anti-inflammatory effect in the IBD [13]. A previous study has reported the role of antioxidant and anti-inflammatory activity of TQ in management of inflammation and colitis [13,14,15].
Unfortunately, the therapeutic effects of most natural components are diminished due to either poor solubility and instability, as in the case of TQ which is photosensitive [16], or the inappropriate resinous nature and difficult administration, as in propolis extract. Well-designed nanocarriers have the advantages of enhancing the physical characterization of entrapped natural extracts, increasing their stability, promoting the cellular permeation, and enhancing the therapeutic effect [17,18,19]. Liposomes are lipid-based nanoarchitectures that are superior to other nanocarriers due to their biological compatibility and ability to entrap both hydrophilic and lipophilic components [20, 21]. The efficiency of liposomes in enhancing the stability, delivery, and targeting of entrapped cargo for the treatment of ulcerative colitis has been reported in previous studies [22,23,24,25]. This study is aimed at evaluating the potential of combination therapy of liposomal formulations of TQ and Egyptian PP on enhancing their therapeutic efficiency against ulcerative colitis to maximize the potential of their favorable clinical effects.
Materials and Methods
Materials
Chemicals
Thymoquinone (TQ) (2-isopropyl-5-methylbenzo-1,4-quinone), chloroform, and cholesterol (more than 99%) Pluronic F127® (Mw 12,600) were bought from Sigma-Aldrich (St. Louis, MO, USA). Propolis extract (PP) was supplied from VACSERA-EGYPT (Cell Culture Department). Phospholipon 90 H® (PL 90H) and Lipoid S75 (soybean phospholipids (fat-free type)) with 70% phosphatidylcholine were obtained from Lipoid GmbH (Germany). Deionized water was obtained from the chemistry laboratory, Deraya University.
Formulation of Thymoquinone and Propolis Liposomes
Thymoquinone-containing liposomes (Lip-TQ) were prepared adopting the reported spraying technique [26]. Briefly, thymoquinone (TQ) (2.5 mg/ml), cholesterol (33.33% molar concentration), and PL 90H® (80 mmol/ml) were dissolved in 2 ml of ethanol and then moved to umber glass closed spraying device. The organic phase was sprayed on the surface of 2 ml sucrose solution (9% w/v) at 37°C with continuous stirring at 1200 rpm until complete evaporation of ethanol.
Propolis liposomes (Lip-PP) were prepared in the same procedures. The organic phase consisted of lipoid S75 (40 mmol/ml), CH% (20% molar concentration), and propolis extract (PP) (3.25 mg/ml) dissolved in 2 ml ethanol. Organic phase was sprayed on the surface of stirred sucrose (9% w/v) at 80°C and 1200 rpm [19].
Formulated liposomes were stored at 4°C overnight to permit the stabilization of the formed bilayer [27]. The liposomal formulations were then ready for further investigations. Both particle size and polydispersity index (PDI) were estimated after dilution with deionized water using a Mastersizer 3000E (Malvern Instruments, Malvern WR14 1X, UK). Average size and PDI were calculated from triplicate measurements. Scanning electron microscopy (SEM) was adopted for imaging of diluted samples with JEOL (JM 1000 EX, Peabody, MA, USA) after drying on carbon grid.
Entrapment Efficiency (EE %) of TQ and PP in Liposomes
Unentrapped TQ and PP were separated from Lip-TQ and Lip-PP, respectively, by centrifugation using cooling centrifuge (Hermle® Z326 K, Germany) at 12,000 rpm for 60 min at 4°C. Two washing cycles were maintained for Lip-TQ and Lip-PP. The supernatants were collected after each washing cycle and analyzed using Spectronic Genesys® (Winspec Software, Spectronic, USA) at 257 nm and 410 nm, respectively, to estimate the unencapsulated TQ and PP, after proper dilution, using the standard calibration curves [27, 19]. Percentage of encapsulated drug was determined by indirectly subtracting the free amount of the drug from the total added amount [28] using the equation [28].
Particle Size Analysis and Zeta Potential Determination
Liposomal size was measured using laser light diffraction methods (Mastersizer 3000E Malvern Instruments, UK). In a summary, pure deionized water was used to dilute the liposomal formulation before it was analyzed at 25°C. Average data were utilized after the procedures were performed three times [29].
Using Mastersizer, the charges on the liposomal surface were also evaluated using Malvern Zetasizer. Using Millipore water, the produced liposomes were diluted, and their zeta potential was assessed [30].
In Vitro Release Study
Using the semipermeable membrane that had been submerged in normal saline solution 0.9% for an hour prior to usage, the in vitro release of TQ and PP from the produced TQ-Lip and PP-Lip was investigated. The membrane was then attached to a reservoir compartment of Franz cell containing 20 ml of receptor media (pH 7.4) made of phosphate citrate buffer and 1% tween 80. To the sample compartment, aliquots of the TQ-Lip and PP-Lip formulations were added; both of which contained 1 mg of the active ingredient. In a thermostatic shaker, the system was shaken at 37 ± 0.5°C and 50 ± 10 rpm. Over the course of 24 h, each 1 ml withdrawn of the release medium was substituted with equal volume of fresh media and kept at the same temperature. Flavonoidal levels (TQ and PP concentrations) were measured spectrophotometrically at 257 and 410 nm, respectively. All experiments were carried out in triplicate. The average values from each experiment were reported, and the cumulative percentage of the released flavonoids was determined and plotted versus time.
Ethical Approval
The Animal Care Committee of the Faculty of Pharmacy, Minia University, Minia, Egypt, approved the study (ES 14/2021) and issued recommendations for the careful handling of animals that were adhered to in accordance with all applicable international standards and guarantee compliance with the European Union Directive 2010/63/EU on animals.
Animal Study
Animals
Male Sprague Dawley rats that were 4–6 weeks old and weighed 150–200 g were housed in the Faculty of Medicine at Minia University’s laboratory animal house. They were housed in standard lab settings with a regular day/night cycle. Standard stainless-steel cages were utilized to keep all rats. For 1 week prior to the beginning of the study, they were allowed to roam freely in their cage and were fed commercial rat chow.
Induction of Ulcerative Colitis
Induction of ulcerative colitis was maintained by the method outlined by Mousavizadeh et al. (2009), where colon tissue was experimentally ulcerated with little modification. Rats were left fasting for 24 h and then anesthetized with ether, and a gel-lubricated soft pediatric catheter (2.7 mm) was inserted 6–8 cm proximal to the anus containing 4% acetic acid (AA). To stop AA leakage after administration, rats were kept horizontally for 2 min. Animals used as controls performed the same procedure using equal volume of saline in place of the AA solution. Rats’ body weights were recorded every day.
Experimental Design
Six groups of 10 rats each were divided as follows:
-
1.
Group I (control group): rats received normal saline intrarectally with no other treatment and were kept randomly wandering in their cages for 10 days.
-
2.
Group II (AA-induced colitis group): rats received acetic acid (AA) intrarectally and were sacrificed 10 days later.
-
3.
Group III (Sulfasalazine-treated group): rats received oral Sulfasalazine (25 mg/kg) after induction of colitis for 10 days [31].
-
4.
Group IV (TQ and PP-treated group): rats received combination of oral free thymoquinone (TQ) (10 mg/kg) [15] and oral free propolis extract (PP) (600 mg/kg) [32] after induction of colitis for 10 days.
-
5.
Group V (LIP-TQ and LIP-PP-treated group): rats received combination of thymoquinone liposomes (LIP-TQ) (10 mg TQ/kg) and propolis liposomes (LIP-PP) (600 mg/kg) after induction of colitis for 10 days.
-
6.
Group VI (empty LIP-treated group): rats received empty liposomes after induction of colitis for 10 days.
General Assessment of Colitis
The activity index of the disease (DAI), which employs a score system for evaluating weight loss, rectal bleeding, and stool consistency, was used to evaluate disease activity. The sum of all the grades was determined for each animal: body weight loss (0 indicates none; 1 indicates 1–5%; 2 indicates 6–10%; 3 indicates 11–20%; and 4 indicates > 20%); stool consistency (0 indicates normal dry stool consistency; 1 indicates wet stools; 2 indicates pasty (greasy and pale) stools; 3 indicates semiliquid stools; 4 indicates watery (entirely liquid with no solid pieces) diarrhea). Concerning rectal bleeding, 0 indicates normal (none); 1 indicates positive hemoccult (hidden blood) by laboratory Guaiac fecal occult blood test; 3 indicates minor bleeding observed by the naked eyes; 4 indicates severe bleeding. DAI values were calculated using the parameters’ average values in each group and then comparing different values by using statistical evaluation [33].
Biochemical Analysis
Ten days after the treatment and after determining DAI, animals were deeply anesthetized then sacrificed [34], blood samples were collected from the left jugular vein at room temperature, and sera were separated by centrifugation at 3000 × g for 10 min at 4°C and then stored in aliquots at − 80°C till used. Five- to six-centimeter-long colon specimens were dissected and washed with saline solution. Samples were photographed and weighed and then divided into two parts, one for molecular and the other for histological examination. For histopathological evaluation, cross sections were fixed in 10% formaldehyde solution. Until analysis, the tissues were kept at − 80°C.
Serum Samples Used for Measuring
Collected sera were used to determine the values of white blood cells (WBCs), lymphocytes, hemoglobin, albumin, and triglycerides in control and treated groups.
Molecular Assessment of the Colon
Predetermined weight of the colon was homogenized in phosphate buffer and centrifuged at 5000 rpm for 10 min at 4°C. Supernatants were utilized for determination of malondialdehyde (MDA) as described by Ohkawa et al. [35]. ELISA kit (Lab Vision Corporation, USA) was used to evaluate concentration of tumor necrosis factor-α (TNF-α) according to the manufacturer’s instructions. Colorimetric kit (Biodiagnostic, Egypt) was used to evaluate concentration of nitrite, an indicator of nitric oxide (NO) production.
Histological and Immunohistochemical Examination
Half of dissected distal colon specimens (5–6 cm) were cleaned with saline solution, photographed and weighed, preserved in 10% neutral-buffered formal saline, dehydrated in a graded ethanol series, cleared in xylene, and embedded in melted paraffin wax. Paraffin-embedded serial Sects. (5–6 μ thick) were stained with hematoxylin and eosin [36] and immune-stained with “caspase-3” antibody [37].
Morphometric Analysis
Using monoclonal anti-caspase-3 antibodies, a digital image analysis assay was performed in order to evaluate the results using the light microscope (Olympus CX-31, Tokyo, Japan) (equipped with ImageJ software). Four tissue blocks for cross and longitudinal sectioning/animal were randomly selected, and serial sections (one cross and one longitudinal section per block) were selected, and three microscopic fields/sections were randomly selected. Area % of caspase-3 immunopositivity was quantified from 10 non-overlapping fields for each rat in each group.
Results
Preparation and Characterization of Lip-TQ and Lip-PP
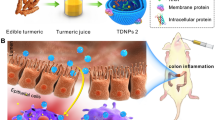
Liposomal formulations of thymoquinone (TQ) and propolis (PP) imaged by SEM were successfully formulated as spherical vesicles with homogenous size distribution (Fig. 1). LIP-TQ exhibited particle size of 192 ± 20.3, PDI 0.268 ± 0.05, and zeta potential 19.3 ± 0.11 while Lip-PP exhibited particle size of 98.2 ± 20.3, PDI 0.213 ± 0.03, and zeta potential 17.1 ± 0.25. LIP-TQ entrapped 85.3 ± 12.6% of added drug (EE%) while Lip-PP entrapped 69.3 ± 11.8 of added extract.
In Vitro Release Study
As shown in Fig. 2, the release of TQ from its free solution and LIP-TQ vesicles was found to be 85.3 ± 12.6 and 29.5% at 6-h timepoint, respectively. Also, the release of PP from its free extract and Lip-PP vesicles was found to be 89.2 and 45.1% at 6-h timepoint, respectively. After 24 h, Lip-TQ release reached 65.2% while Lip-PP release was 45.1%.
Assessment of Colitis
To investigate the severity of colitis, its clinical signs including body weight loss, diarrhea, and rectal bleeding were explored. Rats challenged with acetic acid (AA) in group II displayed with high DAI scores associated with incidence of diarrhea and rectal bleeding, a reliable marker of colon inflammation. Sulfasalazine in group III alleviated these changes and diminished the severity of colonic injury as compared to group II. Moreover, TQ and PP combination in group IV showed significant lower DAI scores as compared to group II and also group III treated by Sulfasalazine. Interestingly, LIP-TQ and LIP-PP-treated group (group V) ameliorates the severity of AA-induced injury in rats and showed the lowest DAI scores compared with all treated groups. On the other hand, rats that received lipid vesicle after induction of colitis showed insignificant effect on DAI scores as compared to AA-induced colitis rats in group II and significantly the highest as compared to all other treated groups (Fig. 3).
The disease activity index (DAI) in the different experimental groups. Data are expressed as mean ± S.E.M. of 10 rats in each group. aSignificant from control group I. bSignificant from group II. cSignificant from group III. dSignificant from group IV, P ≤ 0.05. Group I: control group; group II: AA (acetic acid)-induced colitis group; group III: Sulfasalazine-treated group; group IV: TQ and PP-treated group; group V: LIP-TQ and LIP-PP-treated group; group VI: empty LIP-treated group. Thymoquinone: TQ; propolis: PP; liposomes: LIP
Biochemical and Hematologic Parameters of Treated Groups
The elevated white blood cell and lymphocytes with reduced hemoglobin, albumin, and triglyceride values revealed that AA rectal treatment could induce severe inflammation in the mouse colon (Table I).
Interestingly, oral administration of combination of PP (25 mg/kg) and TQ (5 mg/kg) significantly reduced the number of WBCs compared to the AA-treated group (P < 0.001); further reduction in WBCs was obtained upon treatment with combination of LIP-TQ and LIP-PP (group V) compared to groups of animals treated with Sulfasalazine (group III) and combination of TQ and PP (group IV) (P < 0.001 and P < 0.01, respectively). Count of lymphocytes was also reduced significantly due to treatment with combination of TQ and PP. Simultaneously, administration of LIP-TQ and LIP-PP (group V) has significantly reduced lymphocyte count compared to treatment with Sulfasalazine or combination of PP and TQ, respectively (P < 0.01). In addition, the combined treatment of LIP-TQ and LIP-PP had significantly elevated hemoglobin and albumin levels compared to combined treatment with PP and TQ and treatment with Sulfasalazine (P < 0.05 and P < 0.001, respectively). However, both the combined treatment of PP and TQ and the combined treatment of their liposomal dosage forms caused comparable enhancement in the triglyceride level.
Assessment of the Colon Parameters
The data of the present study in Table II clearly demonstrated that the tissue MDA, TNFα, and nitrite levels were significantly higher in the acetic acid-induced colitis (group II) and in rats that received lipid vesicle (group VI) compared with all other treated groups. On the other hand, these parameters were significantly lower in all treated groups (III, IV, V), but rats in group V treated by combination of LIP-TQ and LIP-PP showed the lowest mean value among all the experimental treated groups followed by group IV than III.
Histological and Immune-Histochemical Assessments
H&E Sections
The control group showed normal histological structure of the colon. The mucosa was folded intact and continuous, with regular arranged tubular crypts, covered with simple columnar epithelium. The crypts are arranged perpendicular to the muscularis mucosae, and their bases contact the upper edge of the muscularis mucosae (Fig. 4 con).
Photomicrographic plate I showing distal colon; group I “con” showing the normal colon, the crypts are uniformly spaced, arranged perpendicular to the muscularis mucosae. Group II (UC) “a–c,” “a” showing disorganized crypts, areas of extravasated blood “asterisks” in the mucosa “M” and in the widened submucosa “SM.” “b, c” The most numerous inflammatory cells seen are eosinophils “thin black arrows,” neutrophils “thin yellow arrows,” and mast cells “thick arrows” that appear beside a blood vessel “BV.” “d” showing superficial mucosal erosions “red arrow” and basal lymphocytosis “rectangles.” Group III “e” showing patchy inflammation (tailed arrows). Group IV “f” showing numerous macrophages (arrows). Group V “g–i”; “g” showing irregular and short crypts and “h” showing nuclear enlargement (black arrows), “i” showing numerous macrophages “yellow arrows.” Group VI “j” showing morphologic picture similar to the control group (H&E stain × 100 and 400)
Group II showed distorted mucosa that appeared with absent folding, lost columnar epithelial lining and goblet cells, and malformed and disorganized crypts. Heavy inflammatory cell infiltration associated with congested and dilated blood vessels and edema together with areas of extravasated blood was observed in the mucosa and in the widened submucosa (Fig. 4a). The most numerous inflammatory cells observed were eosinophils, mast cells, and neutrophils (Fig. 4b, c). Activity is defined as the presence of neutrophil infiltration of surface epithelium, crypt epithelium, and/or collecting within crypt lumens (focal crypt abscesses), less commonly superficial mucosal erosions. Rarely basal lymphocytosis between the bottom of the crypts and the upper edge of the muscularis mucosae was noticed (Fig. 4d).
In group III, patchy inflammation was noticed; mononuclear inflammatory cells were present in the lamina propria but not noticeably expand it (Fig. 4e). In group IV, healing was characterized by absence of active inflammatory cells and appearance of cells involved in resolution of inflammation and regeneration which are macrophages (Fig. 4f). The structural changes, e.g., atrophy, irregularity, shortening of the crypts, and thickening of the muscularis mucosae, were rarely observed (Fig. 4g). In group V, there may no longer be crypt injury (including erosion or ulceration); instead, the crypts showed signs of mitotic activity including varying degrees of nuclear enlargement and stratification (Fig. 4h). The lamina propria showed increased phagocytic cells (Fig. 4i). Morphologic picture of group VI resembled that of the control group (Fig. 4j).
Immune-Histochemical Changes of Caspase III
The control group I showed scarce brown cytoplasmic immune reaction (Fig. 5a). Group II showed widespread cytoplasmic and unclear immuno-reaction in the epithelial cells and mucosal and submucosal C.T cells (Fig. 5b). In addition, the recovered groups healed from UC groups III and IV showed a decrease in caspase-3 immuno-positivity when compared with the UC group (Fig. 5c, d). The reaction was the weakest in group V treated with thymoquinone and propolis carried on nanoparticles (Fig. 5e). Group VI showed widespread cytoplasmic and unclear immuno-reaction in the epithelial cells and C.T cells similar to that of the control group (Fig. 5f).
Photo-micrographic plate II showing distal colon. a The control group I showed scarce brown cytoplasmic immune-reaction. b Group II showed widespread cytoplasmic and nuclear immuno-reaction. c, d Treated groups III and IV showed a decrease in caspase-3 immuno-expression if compared with the UC group. e Group V shows the weakest reaction. f Group VI showed scarce brown cytoplasmic immune-reaction similar to that of the control group (caspase-3 immune-stain × 400)
Morphometric Results Using the Light Microscope
Regarding caspase-3 immunopositivity, as shown in Table III, the area % for caspase-3 immuno-positivity was significantly increased in group II if compared to that of the control and treated groups. In addition, the healing from UC in treated groups III and IV resulted in a decrease in % area for caspase-3 immuno-expression if compared with the UC group. The result was significant in group V treated with combination of LIP-TQ. Group VI showed an increase in area % for caspase-3 immuno-expression more or less similar to that of the UC group II.
Discussion
Despite having numerous advantageous therapeutic features, the clinical application of TQ and PP has been severely limited because of its hydrophobic nature, photosensitivity, temperature, and pH instability. Liposomes have long been regarded as an excellent drug delivery system because they may effectively be loaded with the lipophilic drugs that would otherwise have limited absorption and bioavailability. The lipophilic medications such as TQ and PP can be considered very effective when utilized as a liposomal formulation. This study revealed.
According to the results of the in vitro release profile, the inclusion of TQ and PP in liposomal formulation significantly slows down the release of the encapsulated drugs in comparison to the burst release of the free drug. These findings point to a drug’s sustained release impact as a result of its inclusion into liposomal formulations, which will be a controlled strategy for dealing with any side effects following clinical use. Moreover, the small molecular size of the prepared liposomes guarantees the enhanced cellular uptake of the entrapped cargo [38, 39] affording enhanced therapeutic effect compared to the free unencapsulated combination. This is apparent in the enhancement of biochemical, hematologic, histological, and different colon parameters in animals receiving the liposomal formulations of TQ and propolis compared to those receiving the free drugs.
Ulcerative colitis, induced by experimental technique, in various animal models has gained popularity in research to investigate the pathological pathway of the disease in addition to the study of novel drugs for their promising role in the management of UC owing to the increased similarity between experimentally induced UC in animals by acetic acid and UC in patients [40]. It is typically accompanied by a strong influx of neutrophils and macrophages to the site of damage, as well as superficial ulceration, inflammation, and increased vasopermeability [41]. This could result in the production of hydroxyl radicals and peroxides, which substantially enhances the progression of tissue necrosis and mucosal dysfunction [42].
The administration of AA in the current study led to significantly reduced body weight, which might be related to malabsorption or reduced food intake, as well as extensive fluid loss via rectal bleeding and diarrhea. Additionally, it has been previously shown that elevated levels of cytokines, such as TNF-α, as observed in the current study, significantly contribute to body weight loss through releasing of appetite-suppressing neuropeptides in colitis [43]. The DAI score could be used to determine the severity of the AA-induced colitis. The observed results revealed an elevated DAI score. The existence of at least partial surface maturation, which means that the nuclear changes in the regenerative crypts do not extend to the surface mucosa, is an indicator of regenerative changes.
In the current investigation, AA-induced colitis rats showed an elevated oxidative stress, which was proven by elevated MDA levels. According to [7], oxidative stress and inhibited antioxidant defense systems that control the production of reactive oxygen species (ROS) are one of the major causes of inflammatory illnesses.
IBD in humans is largely a pathology of reactive NO radicals. Numerous studies have suggested that excessive NO, as seen in the current study by elevated levels of nitrites, may make the pathological characteristics of UC worse through mechanisms like direct damage to gut epithelial cells, neutrophil activation, and vasodilation. Additionally, NO has the ability to react with superoxide to create the extremely harmful peroxynitrite radical, which reversibly upregulates the expression of iNOS by activating NF-κB and results in a chain of harmful events [44].
Tissue sections of the distal colon of UC group II were associated with superficial ulceration and inflammatory cell infiltration including mainly eosinophils and mast cells, together with neutrophils and macrophages in the mucosa and submucosa. This was in the same line of Kandhare et al. [41] who stated that UC was associated with enhanced vasopermeability as well as severe influx of neutrophils and macrophages. This could be explained that histiocytic “macrophages” respond to extravasated mucin or fecal material, as a result of crypt injury or surface erosion [45]. Ismail and Aboulkhair [46] reported that in acute UC there was a significant decrease in the number of goblet cells but a significant increase in the number of mast cells, area % of collagen fibers, and COX-2 immuno-expression.
The significant increase in area % for caspase-3 immuno-expression seen in tissue sections of UC group “II” in this study indicated enhanced apoptosis in both epithelial and connective tissue cells of the diseased colon. This was in accordance with [47] who reported that analysis of biopsies from ulcerative colitis patients demonstrated that disease-associated tight junction protein occluding regulates apoptosis by enhancing caspase-3 transcription. Yang et al. [48] reported increases in the levels of apoptosis-related proteins, such as caspase-3 in inflammatory bowel diseases.
Conclusion
The results of the current investigation, which demonstrated that combination therapy of Lip-TQ and Lip-PP had a stronger anti-inflammatory impact in the AA-induced colitis rats, also corroborate the greater efficacy of the combination therapy of Lip-TQ and Lip-PP when compared to the combination therapy with free TQ and free PP.
References
Al-Rejaie SS, Abuohashish HM, Al-Enazi MM, Al-Assaf AH, Parmar MY, Ahmed MM. Protective effect of naringenin on acetic acid-induced ulcerative colitis in rats. World J Gastroenterol. 2013;19:5633–44.
Chu TPC, Moran GW, Card TR. The pattern of underlying cause of death in patients with inflammatory bowel disease in England: a record linkage study. J Crohns Colitis. 2017;11:578–85.
Sun P, Zhang S. Correlations of 25-hydroxyvitamin D3 level in patients with ulcerative colitis with inflammation level, immunity and disease activity. Eur Rev Med Pharmacol Sci. 2018;22:5635–9.
Helal MG, Abd Elhameed AG. Graviola mitigates acetic acid–induced ulcerative colitis in rats: insight on apoptosis and Wnt/Hh signaling crosstalk. Environ Sci Pollut Res. 2021;28:29615–28.
Pecere S, Petito V, Amato A, Poscia A, Armuzzi A, Lopetuso LR, Sgambato A, Cammarota G, Papa A, Gasbarrini A. Infliximab and tumour necrosis factor alpha measurement on intestinal mucosa: a new tool for the clinic? Emj Gastroenterol. 2016;59:107–15.
El-Akabawy G, El-Sherif NM. Zeaxanthin exerts protective effects on acetic acid-induced colitis in rats via modulation of pro-inflammatory cytokines and oxidative stress. Biomed Pharmacother. 2019;111:841–51.
Ansari MN, Rehman NU, Karim A, Soliman GA, Ganaie MA, Raish M, Hamad AM. Role of oxidative stress and inflammatory cytokines (TNF-α and IL-6) in acetic acid-induced ulcerative colitis in rats: ameliorated by Otostegia fruticosa. Life. 2021;11:195.
Bankova VS, de Castro SL, Marcucci MC. Propolis: recent advances in chemistry and plant origin. Apidologie. 2000;31:3–15.
Hwang S, Hwang S, Jo M, Lee CG, Rhee K-J. Oral administration of Korean propolis extract ameliorates DSS-induced colitis in BALB/c mice. Int J Med Sci. 2020;17:1984.
Silva LMd, Souza Pd, Jaouni SKA, Harakeh S, Golbabapour S, de Andrade SF. Propolis and its potential to treat gastrointestinal disorders. Evid-Based Complement Altern Med. 2018;2018:1–12.
Mariano LNB, Arruda C, Somensi LB, Costa APM, Perondi EG, Boeing T, Mariott M, da Silva RdCMVd, Fonseca A, de Souza P. Brazilian green propolis hydroalcoholic extract reduces colon damages caused by dextran sulfate sodium-induced colitis in mice. Inflammopharmacology. 2018;26:1283–92.
Wang K, Jin X, Li Q, Sawaya ACHF, Le Leu RK, Conlon MA, Wu L, Hu F. Propolis from different geographic origins decreases intestinal inflammation and Bacteroides spp. populations in a model of DSS-Induced colitis. Molec Nutr Food Res. 2018;62:1800080.
Samak YO, Santhanes D, El-Massik MA, Coombes AG. Formulation strategies for achieving high delivery efficiency of thymoquinone-containing Nigella sativa extract to the colon based on oral alginate microcapsules for treatment of inflammatory bowel disease. J Microencapsul. 2019;36:204–14.
Lei X, Liu M, Yang Z, Ji M, Guo X, Dong W. Thymoquinone prevents and ameliorates dextran sulfate sodium-induced colitis in mice. Dig Dis Sci. 2012;57:2296–303.
Mahgoub AA. Thymoquinone protects against experimental colitis in rats. Toxicol Lett. 2003;143:133–43.
Salmani JMM, Asghar S, Lv H, Zhou J. Aqueous solubility and degradation kinetics of the phytochemical anticancer thymoquinone; probing the effects of solvents, pH and light. Molecules. 2014;19:5925–39.
Alaaeldin E, Mostafa M, Mansour HF, Soliman GM. Spanlastics as an efficient delivery system for the enhancement of thymoquinone anticancer efficacy: fabrication and cytotoxic studies against breast cancer cell lines. J Drug Deliv Sci Technol. 2021;65: 102725.
Elkot M, Elsayed M, Alaaeldin E, Sarhan H, Shaykoon MSA, Elsadek B. Accelerated stability testing of microcapsulated sorafenib-loaded carbon nanotubes prepared by emulsification/internal gelation method. Int J Pharm Pharm Res. 2019;16:126–39.
Refaat H, Naguib YW, Elsayed MM, Sarhan HA, Alaaeldin E. Modified spraying technique and response surface methodology for the preparation and optimization of propolis liposomes of enhanced anti-proliferative activity against human melanoma cell line A375. Pharmaceutics. 2019;11:558.
Mostafa M, Alaaeldin E, Aly UF, Sarhan HA. Optimization and characterization of thymoquinone-loaded liposomes with enhanced topical anti-inflammatory activity. AAPS PharmSciTech. 2018;19:3490–500.
Musa A, Elmaidomy AH, Sayed AM, Alzarea SI, Al-Sanea MM, Mostafa EM, Hendawy OM, Abdelgawad MA, Youssif KA, Refaat H. Cytotoxic potential, metabolic profiling, and liposomes of Coscinoderma sp. crude extract supported by in silico analysis. Int J Nanomed. 2021;16:3861.
Ahmad A, Vaghasiya K, Kumar A, Alam P, Raza SS, Verma RK, Khan R. Enema based therapy using liposomal formulation of low molecular weight heparin for treatment of active ulcerative colitis: new adjunct therapeutic opportunity. Mater Sci Eng, C. 2021;121: 111851.
Tang Q, Zhang W, Zhang C, Guan Y, Ding J, Yuan C, Tan C, Gao X, Tan S. Oxymatrine loaded nitric oxide-releasing liposomes for the treatment of ulcerative colitis. Int J Pharm. 2020;586: 119617.
Wang C, Han Z, Wu Y, Lu X, Tang X, Xiao J, Li N. Enhancing stability and anti-inflammatory properties of curcumin in ulcerative colitis therapy using liposomes mediated colon-specific drug delivery system. Food Chem Toxicol. 2021;151: 112123.
Xian J, Zhong X, Gu H, Wang X, Li J, Li J, Wu Y, Zhang C, Zhang J. Colonic delivery of celastrol-loaded layer-by-layer liposomes with pectin/trimethylated chitosan coating to enhance its anti-ulcerative colitis effects. Pharmaceutics. 2021;13:2005.
Refaat H, Mady FM, Sarhan HA, Rateb HS, Alaaeldin E. Optimization and evaluation of propolis liposomes as a promising therapeutic approach for COVID-19. Int J Pharm. 2021;592: 120028.
Odeh F, Ismail SI, Abu-Dahab R, Mahmoud IS, Al Bawab A. Thymoquinone in liposomes: a study of loading efficiency and biological activity towards breast cancer. Drug Delivery. 2012;19:371–7.
Lopez-Pinto J, Gonzalez-Rodriguez M, Rabasco A. Effect of cholesterol and ethanol on dermal delivery from DPPC liposomes. Int J Pharm. 2005;298:1–12.
New RR (1990) Preparation of liposomes. Liposomes: a practical approach, 33–104
Ruozi B, et al. Atomic force microscopy and photon correlation spectroscopy: two techniques for rapid characterization of liposomes. Eur J Pharm Sci. 2005;25:81–9.
Shin M-R, Kim KJ, Kim SH, Kim SJ, Seo B-I, An H-J, Roh S-S. Comparative evaluation between sulfasalazine alone and in combination with herbal medicine on DSS-induced ulcerative colitis mice. BioMed Res Int. 2017;2017:1–10.
Aslan A, Temiz M, Atik E, Polat G, Sahinler N, Besirov E, Aban N, Parsak CK. Effectiveness of mesalamine and propolis in experimental colitis. Adv Ther. 2007;24:1085–97.
Niu X, Zhang H, Li W, Wang Y, Mu Q, Wang X, He Z, Yao H. Protective effect of cavidine on acetic acid-induced murine colitis via regulating antioxidant, cytokine profile and NF-κB signal transduction pathways. Chem Biol Interact. 2015;239:34–45.
Kannan N, Guruvayoorappan C. Protective effect of Bauhinia tomentosa on acetic acid induced ulcerative colitis by regulating antioxidant and inflammatory mediators. Int Immunopharmacol. 2013;16:57–66.
Ohkawa H, Ohishi N, Yagi K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem. 1979;95:351–8.
Drury R, Wallington E. Carleton’s histological technique. 5th ed. New York: Churchill Livingstone; 1980.
Bancroft JD, Gamble M (2008) Theory and practice of histological techniques (Elsevier health sciences).
Abou-Taleb HA, Sayed AM, Refaat H, Alsenani F, Alaaeldin E, Mokhtar FA, Abdelmohsen UR, Shady NH. Network pharmacological analysis of the red sea sponge hyrtios erectus extract to reveal anticancer efficacy of corresponding loaded niosomes. Mar Drugs. 2022;20:628.
Musa A, Elmaidomy AH, Sayed AM, Alzarea SI, Al-Sanea MM, Mostafa EM, Hendawy OM, Abdelgawad MA, Youssif KA, Refaat H. Cytotoxic potential, metabolic profiling, and liposomes of Coscinoderma sp. crude extract supported by in silico analysis. Int J Nanomed. 2021;16:3861–74.
Sadraei H, Asghari G, Khanabadi M, Minaiyan M. Anti-inflammatory effect of apigenin and hydroalcoholic extract of Dracocephalum kotschyi on acetic acid-induced colitis in rats. Res Pharm Sci. 2017;12:322–9.
Kandhare A, Patil A, Guru A, Mukhrjee A, Sarkar A, Sengupta A, Parmar H, Muthal A, Wangikar P, Bodhankar S. Ameliorative effect of ferulic acid against acetic acid induced ulcerative colitis: role of HO-1 and Nrf2. Pharmacologia. 2016;7:114–24.
Colombo BB, Fattori V, Guazelli CFS, Zaninelli TH, Carvalho TT, Ferraz CR, Bussmann AJC, Ruiz-Miyazawa KW, Baracat MM, Casagrande R, et al. Vinpocetine ameliorates acetic acid-induced colitis by inhibiting NF-κB activation in mice. Inflammation. 2018;41:1276–89.
Hunschede S, Kubant R, Akilen R, Thomas S, Anderson GH. Decreased appetite after high-intensity exercise correlates with increased plasma interleukin-6 in normal-weight and overweight/obese boys. Curr Dev Nutr. 2017;1: e000398.
Joo M, Kim HS, Kwon TH, Palikhe A, Zaw TS, Jeong JH, Sohn UD. Anti-inflammatory effects of flavonoids on TNBS-induced colitis of rats. KJPP. 2014;19:43–50.
DeRoche TC, Xiao S-Y, Liu X. Histological evaluation in ulcerative colitis. Gastroenterol Rep. 2014;2:178–92.
Ismail DI, Aboulkhair AG. Royal jelly protects against experimentally-induced ulcerative colitis in adult male albino rats: a histological study. Egypt J Histol. 2018;41:192–203.
Kuo W-T, Shen L, Zuo L, Shashikanth N, Ong MLDM, Wu L, Zha J, Edelblum KL, Wang Y, Wang Y. Inflammation-induced occludin downregulation limits epithelial apoptosis by suppressing caspase-3 expression. Gastroenterology. 2019;157:1323–37.
Yang L, Shen L, Li Y, Li Y, Yu S, Wang S. Hyperoside attenuates dextran sulfate sodium-induced colitis in mice possibly via activation of the Nrf2 signalling pathway. J Inflamm. 2017;14:1–10.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
Contribution of authors to the paper is almost equal including experimental work, data analysis, interpretation of the results, and editing the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alaaeldin, E., Refaat, H., Saber, E.A. et al. Co-administration of Thymoquinone and Propolis in Liposomal Formulations as a Potential Approach for Treatment of Acetic Acid-Induced Ulcerative Colitis: Physiological and Histopathological Analysis. AAPS PharmSciTech 24, 190 (2023). https://doi.org/10.1208/s12249-023-02637-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-023-02637-1