Abstract
The humanoid nail is considered an exceptional protective barrier that is formed mainly from keratin. Onychomycosis is the cause of 50% of nail infections that is generally caused by dermatophytes. Firstly, the infection was regarded as a cosmetic problem but because of the tenacious nature of onychomycosis and its relapses, these infections have attracted medical attention. The first line of therapy was the oral antifungal agents which were proven to be effective; nevertheless, they exhibited hepato-toxic side effects, alongside drug interactions. Following, the opportunity was shifted to the topical remedies, as onychomycosis is rather superficial, yet this route is hindered by the keratinized layers in the nail plate. A potential alternative to overcome the obstacle was applying different mechanical, physical, and chemical methods to boost the penetration of drugs through the nail plate. Unfortunately, these methods might be expensive, require an expert to be completed, or even be followed by pain or more serious side effects. Furthermore, topical formulations such as nail lacquers and patches do not provide enough sustaining effects. Recently, newer therapies such as nanovesicles, nanoparticles, and nanoemulsions have emerged for the treatment of onychomycosis that provided effective treatment with possibly no side effects. This review states the treatment strategies such as mechanical, physical, and chemical methods, and highlights various innovative dosage forms and nanosystems developed in the last 10 years with a focus on advanced findings regarding formulation systems. Furthermore, it demonstrates the natural bioactives and their formulation as nanosystems, and the most relevant clinical outcomes.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The nail unit is considered a shield to the fingers’ and toes’ edge phalanges against trauma. The nail plate is a rough construction covering a thin glabrous epidermis, which is the nail bed or matrix [1]. At the nail root, the basal cells of the nail matrix are unceasingly divided by mitosis, and thus the plate keeps growing interminably during its lifetime, where the new cells are differentiated, and keratinized, thus forcing the old cells towards the dorsal surface [2]. The nail is composed mainly of protein (about 80%), water (7–12%), lipids (< 1.5%), and minute quantities of minerals and electrolytes. Keratin, as a main component of the nail plate, is linked with disulfide bonds, electrostatic bonds, and hydrogen bonds, with the presence of phospholipid in low amounts; therefore, the nail plate represents a hydrogel membrane barrier with a limited degree of permeability [3]. Hyponychium is the epithelium under the nail plate at the junction between the nail-free edge and the skin of the fingertip, which acts as a seal for the nail bed [4]. The mean growth rate of fingernails and toenails per month is 3 mm and 1 mm respectively, where complete regeneration of a fingernail occurs in 4–6 months and 8–12 months for a toenail [3]. More than half of the diseases that affect nails are triggered by fungi, including dermatophytes, non-dermatophytes, molds, and yeasts, where the main species belong to the genera Trichophyton, Epidermophyton, or Microsporum [5]. Infection idiosyncrasies are correlated to the microorganism, general health of patient health, and nail features.
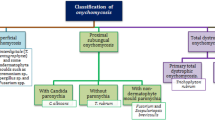
Onychomycosis is caused by nail fungal infestation resulting in thickening, roughness, yellow–brown discoloration, distortion, splitting, and finally detachment of the nail [6]. Onychomycosis could be classified into four categories: distal subungual onychomycosis (DSO), proximal subungual onychomycosis, superficial white onychomycosis, endonyx onychomycosis, and total dystrophic onychomycosis [7]. Trichophyton rubrum is the causative agent of DSO. It is presented at the sides of the nail plate including its bed, where the spread begins at the hyponychium and then to the nail matrix. Proximal sub-ungual onychomycosis is usually occurred in immunocompromised patients and is caused by T. rubrum that passes in the proximal nail folds by permeating the developing nail plate. White superficial onychomycosis occurs in 10% of patients and is caused by Trichophyton mentagrophytes at the external part of the nail plate forming deep white impressions on the nail plate. Endonyx onychomycosis is caused by Trichophyton soudanense and Trichophyton violaceum, and invades the superficial surface and goes deeper into the nail plate. The end stage of the disease is total nail dystrophy which is characterized by thickening and yellow discoloration of the nail plate [5, 8, 9].
The prevalence of the disease also upsurges with age, with the prevalence in those younger than 18 years (0.5–3%) [10], due to the existence of diseases, impaired immunity, and unhygienic conditions of toenails with improper foot cleanliness [11]. The prevalence is increased by 25% in patients with human immunodeficiency virus disease. Although onychomycosis causes cosmetic discomfort and social concern, the disease may be accompanied by distress and might be allied with physical and work-related limits, and thus reduced quality of life [12]. Moreover, onychomycosis is extremely difficult to treat due to rigid nail structure, increased treatment time, and the high probability of disease relapse.
The diagnosis is accomplished through the laboratory and microscopy method, fungal culture, and biopsy [13, 14]. For the treatment of onychomycosis, terbinafine (the gold standard), griseofulvin, and itraconazole are given orally, and ketoconazole and fluconazole might be used as off-label treatment [15]. The topically applied antifungal agents are amorolfine, ciclopirox, efinaconazole, and tavaborole [16]. Oral therapy is effective and at a low cost; however, hepatotoxicity, cardiac disturbances, and drug interactions are chief drawbacks that lead to patient nonadherence and adverse events [5]. On the other side, topical treatment is associated with fewer side effects and high patient compliance, while poor drug diffusion into the rigid nail structure is the main barrier [17]. In the last few years, different physical and chemical approaches emerged along with topically applied treatments including nail solutions and lacquers. The physical and chemical methods displayed a set of drawbacks and are not commercially available in the market, while nail solutions and lacquers were not effective enough because of the keratin content of the nails leading to insufficient drug permeability.
Therefore, there was a need for a transungual drug delivery system that involves better drug penetration through nails to resolve nail diseases, advance patient compliance, and show efficient results. Here comes the role of nanoformulations which would enhance targeted drug delivery, increase drug retention, minimize the doses, and thus reduce toxicity. Different delivery systems have been utilized for the treatment of onychomycosis such as polymeric films, in situ gels, and nano-based systems. This review outlines various treatment approaches such as mechanical, physical, and chemical methods, and demonstrates in detail the formulated nanoparticle-based modalities presented since 2012, as innovative and alternative ways of therapy for onychomycosis. Moreover, it states the natural bioactives and their formulation as nanosystems, and the most relevant clinical outcomes.
Modes of Therapy
Mechanical Methods
Nail Avulsion
It involves complete surgical of the nail plate from other units, either by physical removal (inserting Free’s elevator) or by chemical treatment (applying urea ointment). This procedure might display postoperative nail deformity or pain [18].
Nail Abrasion
This procedure is accomplished via filing or sanding of the nail plate with sandpaper attached to the dermabrader device. It is usually applied in combination with topical antifungal agents. The technique reduces the fungal load and enhances drug diffusion without complications [19].
Physical Methods
The physical methods are widely used for topically applied and transdermal modes of delivery, and even though they are efficient in enhancing the nail penetration of topical medications, they are not cheap due to the complicated technology and equipment [15].
Microporation of the Nail Plate
Microporation is the process of piercing discrete small pits in the nail plate, but not the nail bed, using PathFormer (Path Scientific, Carlisle, USA), which is mainly used to drain hematomas. The procedure was used along with the topical application of terbinafine cream, where enhanced permeation was achieved [15, 20, 21].
Etching the Nail Surface
Etching, sometimes called acid etching, is the process of applying a surface-modifying chemical (e.g., phosphoric acid) to form profuse microporosities with increased surface area and enhanced wettability. The resultant rough surface provides higher opportunities for the adhesiveness and attachment of the delivery system (mainly polymeric) and thus improves the penetration of drugs [22]. This procedure was found to enhance the permeability of ketoconazole through the nails [23].
Iontophoresis
Iontophoresis involves the application of a mild electric current to boost the penetration of molecules through various barriers [24]. The process is accomplished through a small device that consists of an anode and a cathode along with a source of power, where the ionized drug is sited at the electrode carrying a similarly electric charge, and the oppositely charged electrode is attached to the body. Upon running the electric field, anions flow from the cathode towards the anode, whereas cations move in the opposite direction. In this method, the structure of the nail is preserved and is of low cost; therefore, patients are compliant; however, long-term safety should be determined due to cutaneous adverse effects [5, 15]. Terbinafine is the drug of choice along with iontophoresis, being transported at acidic pHs (around 3) where full ionization of the drug is accomplished [25].
Laser
Laser stands for “light amplification by stimulated emission of radiation” which was found effective in fungi through photoselective damage to their pigmented structures [15]. The short-pulse neodymium yttrium–aluminum garnet (Nd:YAG) 1064 device, titanium sapphire, and diode lasers are used in onychomycosis treatment [26]. The abrasion of the nail plate is achieved by the application of a laser at 5000 W/cm2, where thermal damage has fungistatic or fungicidal activities [27]. These lasers are FDA-labeled as “temporary increase of clear nail in onychomycosis” due to their beautifying result, and because of their undetermined long-term microbiological and clinical effects [28]. Moreover, their drawbacks include high cost and photoaging. Another research work has discussed the active transport of methylene blue solution as a drug via applying the Er: YLF-laser for nail perforation by means of pulsed radiation of microsecond Yb, Er: Glass laser, and the method was proved to be successful [29].
Photodynamic Therapy
Photodynamic therapy aims to combine both a photosensitizer (PS) and a light source, where the former excites the photosensitizer to produce reactive oxygen species, which then destroy the cells by necrosis or apoptosis. It should be noted that the availability of oxygen is important for the process to be completed. Photodynamic light sources might be intense pulsed light, light-emitting diodes, or lasers, where the ideal wavelength should be adjusted for each PS. PSs fall into three categories, including porphyrins, chlorophylls, and dyes. For the treatment of skin conditions, 5-aminolevulinic acid (ALA) and methyl aminolevulinate are used topically. This method is highly selective and effective; however, erythema, burning, and pain may occur [30, 31].
Ultrasound Sonic Waves
It involves the application of sonic waves that are able to produce micro-pores in the nails that facilitate drug permeation. This procedure is non-invasive with minimal relapse; however, it is expensive, and its safety is not completely addressed [5, 13].
Microneedles
Dissolvable microneedles can be used in the form of topical patches and they create pores in the nails to boost drug penetration. This method is easy, simple, and circumvents system toxicity with improved patient compliance [32].
Chemical Methods
The chemical method involves the usage of certain substances (before or with formulation) to cleave different bonds in the nail plate including the disulfide bonds. Keratinolytic enzymes such as papain and keratinase can be used as penetration enhancers. Sulfites (sodium sulfite) and thiols (mercaptoethanol) have the ability to break the nail disulfide bond. For example, N-acetyl-l-cysteine boosted the oxiconazole quantity retained in the nails upon its incorporation into the formulation [13]. Hydrophobins are fungal proteins that are classified as coating or protective agents; they were used successfully with terbinafine [33].
Regarding the incorporation of solvents in the formulation, dimethyl sulfoxide was proven to boost the nail plate penetrability [34]. The influence of polyethylene glycols (PEGs) on the transungual delivery of terbinafine gel formulation was studied in the absence and presence of iontophoresis (0.5 mA/cm2), where low molecular weight PEGs (200 and 400 MW) displayed enhanced drug delivery properties compared to PEGs with higher molecular weight (1000–3350 MW) in both cases [35]. A different class of chemical enhancers is nail softeners. This group includes sodium salicylate, salicylic acid, and urea, where their action is mainly due to keratin denaturation and solubilization via breaking disulfide bonds and thus enhancing drug permeation [5]. Some other chemicals were not found to be effective in increasing transungual drug delivery, such as sodium lauryl sulfate [15], neat alcohol [5], and acetone [15].
Topical Therapeutic Approaches
Nail Lacquer
Conventional pharmaceutical topical systems like solutions, lotions, gels, creams, or suspensions are usually unbefitting for resolving nail diseases, principally because of their poor ability to be retained at the site of application long enough to allow drug penetration. In this context, nail lacquers or paints are usually applied to improve the efficacy of antifungal drugs [36]. As shown in Fig. 1, nail lacquers are mainly formulated from film-forming polymers (water-soluble or insoluble resins) and volatile solvents, which dry quickly leaving a smooth film on the nail plate that acts as a depot for drug release [37]. The factors affecting the effectiveness of nail lacquer are displayed in Fig. 2. The antifungal drugs, amorolfine and ciclopirox, are marketed as nail lacquers and are advised to be applied after nail abrasion. Penlac® is an FDA-approved hydro-lacquer loaded with 8% ciclopirox [38], while Loceryl®, a water-insoluble nail lacquer, contains 5% amorolfine [39]. The incorporation of different polymers in nail lacquers, such as hydroxyl propyl chitosan and dual acrylate–silicone hybrid copolymer, resulted in boosting the permeation of ciclopirox and ketoconazole respectively [28]; nevertheless, nail lacquers are either easily washable and not provide enough sustaining effect or waterproof that are uneasy to remove.
Patches and Films
Nail patches have emerged as an improvement over nail lacquers, to shorten treatment periods and improve patient compliance, as patches provide a delayed release of drugs. It is usually made up of a pressure-sensitive adhesive matrix as a medication reservoir, a drug-impermeable backing membrane, and a release liner. Patches of ALA were able to sustain the drug release for 2 days [40]. Transungual films provide sustained drug release and they are formulated via film casting techniques or hot melt extrusion. Mididoddi et al. prepared a hydroxy propyl cellulose–based film of ketoconazole drug using hot melt extrusion [41].
Gels
Gels or hydrogels are formulated using hydrophilic polymers (natural or synthetic), which upon dispersion in a vehicle form a three-dimensional structure [42]. Their preference in the medicating of nail diseases is due to their ability to accommodate a significant amount of water and thus hydrate the nail plate, which in turn improves drug permeation [18]. Other advantages of gels are illustrated in Fig. 3. Nevertheless, the drawbacks of using gels in treating nail diseases include the unease of application due to viscosity and their dissipation from the nail surface during day-to-day activities. However, in situ gelling systems have been introduced where they are present in a liquid state at certain conditions (temperature, pH, and ionic strength) and then subsequently transformed into a gel (Sol–Gel Transition) upon changing these conditions, i.e., after application to the nail [9].
Poloxamers are a famous example that undergoes transition due to temperature fluctuations. Another point to be considered is that gels are hydrophilic in nature and therefore can be used concomitantly with iontophoresis to transport charged drug molecules across the nail plate [43].
Innovative Nanosystems for Transungual Drug Delivery
To ensure complete treatment of fungal nail infections for a short period of time, a sufficient amount of the drug should diffuse into the nail plate so that it can eliminate hyphae. On the other side, antifungal drugs possess physicochemical characteristics that act as a barrier for penetrating the keratinized nail plate such as lipophilicity and molecular weight (Fig. 4). The larger the molecular size, the lesser would be the drug penetration. On the other side, the larger the molecular size, the lesser would be the drug penetration. It should be noted that different antifungals have different acidic strengths, except miconazole which is independent of pH to get penetrated through a nail plate; moreover, efinaconazole and tavaborole do not bind to keratin. As per the mentioned facts, potential nanosystems have been anticipated to increase the penetration of drugs into the nails, and various examples are listed in Table I.
Nanovesicular Systems
Vesicular systems have become a well-established tool for drug delivery and diagnosis purposes. Nanovesicles such as liposomes, ethosomes, and transferosomes have been loaded with a wide drug variety, either hydrophobic or hydrophilic, to target specific sites of action, and applied through different routes, for example orally and topically. Lipososmes are unilamellar or multilamellar vesicles formulated using phospholipids and cholesterol and arranged into bilayers, while ethosomes contain alcohol to enhance the drug penetration, and both can be employed to treat onychomycosis [90]. Following, another nanovesicular generation with advanced penetration capabilities emerged compromising niosomes, transferosomes, spanlastics, and invasomes. These nanovesicles would be beneficial in transungual delivery for nail fungal infections. For example, terbinafine HCl was formulated as a film formulation loaded with liposomes. The films were synthesized by Eudragit or pullulan [72]. As niosomes are known for their high penetrability, itraconazole was formulated as niosomes where the cholesterol content was found to significantly affect the permeation of the drug through the skin [56]. Additionally, efinaconazole was loaded in transferosomes containing Tween 80 as a surfactant, which showed improved therapeutic results without any signs of erythema and/or edema [52]. Spanlastics are vesicular carriers that are mainly made up of Span 60 and an edge activator with enhanced penetrability. Efinaconazole and terbinafine were formulated as spanlastics for transungual delivery [53, 73]. Furthermore, itraconazole was formulated as invasosomes, which are flexible vesicles principally made of phospholipids and ethanol, in addition to terpene. Invasomes enhanced the permeation of the medication into the nail plates, while terpenes improved the drug infiltration through the skin, which occurred by disrupting the constrained arrangement of the stratum corneum lipids [57].
Nanoparticles
In the last decade, nanoparticles (NPs) were exploited as innovative delivery systems for the treatment of many diseases as they have a dual role in drug targeting and refining drug penetration. As a transungual drug delivery system, NPs have the advantage of convenient application and bypass the side effects of both orally administered drugs and undesirable problems associated with conventional dosage forms [18].
Lipidic Nanoparticles
Lipidic nanoparticles such as solid lipid nanoparticles and nanostructure lipid carriers (NLCs) are colloidal nano-transporters, which are widely applied for the delivery of antifungal drugs as they deposit in skin appendages and sustain the release of the drugs. Moreover, they have the ability to boost the moisture of the skin and nails moisture, and thus improve drug permeability [91]. NLCs are formulated using a mixture of solid and liquid lipids, where the oil lessens crystallization forming a disorganized lipid matrix with imperfections that allows higher entrapment efficiency of drugs [92]. For instance, ketoconazole enriched with Ucuùba (an Amazonian fat) was encapsulated in nanostructured lipid carriers, where the formulation was found to be biocompatible and bioactive [63]. Furthermore, terbinafine HCl was incorporated in solid lipid nanoparticles containing thiourea as a penetration enhancer which resulted in producing particle size of very small size with better penetrability properties [79]. Moreover, nanostructured lipid carriers of voriconazole were prepared using urea as the optimal penetration enhancer [87].
Polymeric Nanoparticles
Polymeric nanoparticles are biocompatible delivery systems with flexible designs. They are characterized by their stability and long duration of action with site specificity, improved therapeutic efficacy, and minimized toxicity [18]. For illustration, chitosan nanoparticles were formulated encapsulating both itraconazole and diflourinated curcumin using an ionotropic gelation technique. These particles were further loaded in Carbopol 940 gel [93].
Metallic Nanoparticles
Metallic nanoparticles have various applications in wide-ranging areas such as electronics, imaging, cosmetics, and drug delivery [94]. They have shown maximized therapeutic index of drugs through site-specificity thus overcoming multidrug resistance. They are synthesized either via the top-down approach (dispersion method) which involves size reduction, or the bottom-up approach (condensation method) which involves a high degree of supersaturation followed by nuclei growth [95]. Several metallic nanoparticles were employed for their antimicrobial activity. Metallic nanoparticles were widely employed either alone or mixed with another antifungal agent (e.g., griseofulvin) as shown in Table II. As an example, aluminum-phthalocyanine chloride was formulated as nanoemulsion with PS (30.49 nm) and PDI (0.166) containing 9 g of Cremophor ELP® and 3 g of castor oil for nanoemulgel preparation [96]. Zinc oxide nanoparticles and the nanopaint laden with zinc oxide nanoparticles displayed substantial antifungal activity. Furthermore, silver and gold nanoparticles displayed enhanced antifungal activity [97, 98].
Nanoemulsions and Nanoemulgel
Microemulsions (NEs) are thermodynamically stable systems with globule size of 10–100 nm. NEs have displayed heightened bioavailability, absorption, and permeation of hydrophilic and hydrophobic drugs. NEs are formulated using oil, surfactant, cosurfactant, and water in definite proportions [9]. NEs gained a broad reputation as topical formulations because of their ability to accommodate considerable quantities of drugs and boost their permeation through dermal membranes, besides exhibiting a high safety profile. Moreover, they displayed superior physical stability [101]. NEs can be formed spontaneously or through the use of high-energy emulsification methods [102]. NEs can be transformed into a gel to form a nanoemulgel by dispersing the oily phase (along with the drug) within an aqueous phase of the gel base. Emulgels have improved stability with a prolonged contact time [103]. Nanoemulgel was formulated with undecylenic acid as the oily phase and laden with amorolfine HCl incorporating thioglycolic acid as a permeation enhancer [44]. In addition, ketoconazole optimized nanoemulsion was formulated as a nanoemulgel by incorporating Carbopol® Ultrez 21 and thioglycolic acid as a penetration enhancer [59]. Moreover, ketoconazole was incorporated in a microemulsion prepared with nigella oil (as a penetration enhancer) and the microemulsion was added to a polymeric gel base [62].
Special Nanosystems
The application of nanotechnology in the pharmaceutical field yielded different nanosystems with enhanced properties. For instance, nanocapsules are special nanosystems that are formulated with a lipophilic solid or liquid core encapsulated in a polymeric shell made of synthetic polymers like poly-lactic acid and poly-lactide-co-glycolide [39]. Ciclopirox olamine was formulated as core-coat polymeric nanocapsules, where poly lactide-co-glycolide was employed as a coat that protects the drug against rapid release from the oily core [47]. Another special nanosystem is the nanospheres, which were formulated using Eudragit RSPO or ethyl cellulose to accommodate terbinafine HCl. In this context, the use of Eudragit RSPO was preferred to ethyl cellulose which resulted in repeatedly small particles with reasonably low polydispersity index when compared to ethyl cellulose [82]. Terbinafine HCl was also entrapped in PEGylated- keratin particles forming water channels, favoring drug diffusion and release over non-PEGylated keratin particles [85]. Antifungal agents were also formulated as nanosuspension and nanomicelles as nanosystems for their delivery to treat onychomycosis. Griseofulvin nanosuspension was formulated using hydroxypropyl methylcellulose acetate succinate and dodecyl trimethylammonum bromide (DTAB), as a surfactant, after which it was suspended with spray-dried silica-coated silver nanoparticles. Griseofulvin-loaded nanosuspensions with DTAB showed superior effectiveness, whereas colloidal silver did not appear to substantially enhance the antifungal activity [54]. Another antifungal agent, voriconazole, was formulated as nanomicelles, where thioglycolic acid was applied on the nails as a pre-treatment, which enhanced voriconazole permeation by threefold [88].
Natural Bioactives and Their Formulation as Nanosystems for the Treatment of Onychomycosis
Natural bioactives have been exploited as an alternative treatment or in combination with other drugs for the management of onychomycosis. The reason behind this is the low cost, minimum adverse reactions, and low risk for the emergence of fungal resistance because of the complex nature and composition of bioactive constituents [104]. Various essential oils were incorporated in different nanosystems either alone or mixed with other antifungal agents as exhibited in Table III. Tea tree oil was formulated as both nanoemulsions and nanocapsules. Nanocapsules were proved to be more efficient, and this may be attributed to their ability to reduce the volatilization of tea tree oil compared to nanoemulsions [105]. Furthermore, tioconazole and Melaleuca alternifolia essential oil were formulated as a Pickering emulsion which showed maximum stability when the fractional wetting conditions of stabilizing particles (silica nanoparticles) are similar for both oily and aqueous phases [106]. Chlorin e6 is a naturally occurring chlorin and is employed as a photosensitizer, and was loaded into nanovesicles incorporating penetration enhancer to examine the effect of the formulation on the photodynamic-mediated activity against T. rubrum, where the results showed higher nail hydration and drug uptake.
Application of Printing in the Treatment of Onychomycosis
Inkjet printing has evolved as a new technology and has been applied in the medical field for the purpose of treatment. Recently, Pollard et al. reported a method for the management of onychomycosis via printing terbinafine hydrochloride directly onto nails using a commercially available cosmetic printer for nails equipped with homemade ink containing the drug. The in vitro antifungal assay of the printed-on disks displayed the inhibition of T. rubrum growth in human nails [83].
Clinical Studies for Treating Onychomycosis
In general, clinical studies are conducted to verify the effectiveness and biosafety of the application of different treatments in patients. Different clinical studies were carried out to demonstrate the effectiveness and biosafety of some developed nanosystems in patients with onychomycosis. Regenail® a cyclodextrin polypseudorotaxanes nail lacquer was proven to minimize surface harshness without changing nail structure and met patient acceptance and satisfaction [70]. BB2603 is a nano-formulation of terbinafine hydrochloride and it was experimented clinically against (1%) Lamisil spray to evaluate systemic involvement, biosafety, and acceptability. The results of pharmacokinetic, safety (no sensitization), and efficacy (anti-dermatophytes activity) profiles supported the use of nanosystems for drug delivery to nails and even to the skin [81]. A clinical trial that utilizes photodynamic treatment facilitated by aluminum-phthalocyanine chloride entrapped in nanoemulsions was established. The approach revealed 60% resolution of the treated lesions with negative fungal culture for about a month, the absenteeism of local and systemic side effects, in addition to lack of collateral effects as a result of the local treatment, and the potentiality to reapply the treatment without inducing fungal resistance [96]. Moreover, Aggrawel et al. listed some nail formulations, such as NB 002, ME 1111, VT 1161, TDT 067, and MOB-015, that are going through different phases of clinical trials which are able to advance the efficiency of therapy [13].
Conclusion
Onychomycosis represents a tenacious and invasive fungal infection because of the weak penetrability of the antifungal medications through the nail plate which eventually leads to the failure of therapy and, consequently, relapses. Mechanical, physical, and chemical methods of treatment suffer from high costs and unknown long-term side effects of some techniques. Topical formulations such as nail lacquers and patches do not provide enough sustaining effects. As per such conditions, nanosystems like nanoparticles and herbal-based formulations seem promising due to minimized side effects, and better drug penetration and retention. Being an invader of multiple fields, nanotechnology along with novel technology such as printing would be the most effective therapy to overcome the challenges of transungual drug delivery.
Data Availability
All data are represented in the manuscript.
References
Yadav V, Srivastava V, Dwivedi KP, Singh R, Yadav A, Verma NK. Disease of nails (fungal infection), diagnosis & treatment (nail lacquer): a review. 2022;11(10):663–694.
Mohamed SA, Hargest R. Surgical anatomy of the skin. Surgery (Oxford). 2021;40(1):1–7.
Bhattacharjee B, Dey N, Barman D, Karmakar A, Ahmed N. Understanding the drug delivery through nails: a comprehensive review. J Drug Deliv Ther. 2021;11(4):116–31.
Mrig PA, Meena N. Nail anatomy and physiology. Nail Disorders: CRC Press; 2019. p. 11–9.
Aggarwal R, Targhotra M, Kumar B, Sahoo P, Chauhan M. Treatment and management strategies of onychomycosis. J Mycol Méd. 2020;30(2): 100949.
Piraccini BM, Holzberg M, Pasch M, Rigopoulos D. The nail in dermatological conditions. Baran and Dawber’s diseases of the nails and their management 5th ed. Hoboken: John Wiley & Sons Ltd; 2019. p. 409–694.
Gupta AK, MacLeod MA, Tosti A. Onychomycosis: clinical aspects. Scher and Daniel’s nails. Springer; 2018. p. 153–159.
Pattanaik S, Thakur P, Guleria M, Tripathy S, Ali SI, Chhetri J, et al. Topical drug delivery of antimicrobial agent using modern technique to treat various nail infection. 2021;51(1):708–721.
Giri Y, Behera A, Mohanty B, Pattnaik G, Habibullah S. Transungual drug delivery system for the topical treatment of onychomycosis: a review. Drug Deliv Lett. 2022;12(1):2–18.
Gupta AK, Venkataraman M, Quinlan EM. Onychomycosis in the twenty-first century: an update on epidemiology and diagnosis. Dermatophytes and Dermatophytoses: Springer; 2021. p. 41–64.
Richert B. Nail disorders in the elderly. Baran and Dawber’s diseases of the nails and their management. 2018. p. 337–341.
Stewart CR, Algu L, Kamran R, Leveille CF, Abid K, Rae C, et al. Effect of onychomycosis and treatment on patient-reported quality-of-life outcomes: a systematic review. J Am Acad Dermatol. 2021;85(5):1227–39.
Aggarwal R, Targhotra M, Sahoo P, Chauhan MK. Onychomycosis: novel strategies for treatment. J Drug Deliv Sci Technol. 2020;57: 101774.
Gupta AK, Mays RR, Versteeg SG, Shear NH, Piguet V. Update on current approaches to diagnosis and treatment of onychomycosis. Expert Rev Anti Infect Ther. 2018;16(12):929–38.
Angelo T, Borgheti-Cardoso LN, Gelfuso GM, Taveira SF, Gratieri T. Chemical and physical strategies in onychomycosis topical treatment: a review. Med Mycol. 2017;55(5):461–75.
Gupta AK, Daigle D, Foley KA. Topical therapy for toenail onychomycosis: an evidence-based review. Am J Clin Dermatol. 2014;15(6):489–502.
Gupta AK, Polla Ravi S, Choi SY, Konda A, Cooper EA. Strategies for the enhancement of nail plate permeation of drugs to treat onychomycosis. J Eur Acad Dermatol Venereol. 2022;37(2):243–255.
Dhamoon RK, Popli H, Gupta M. Novel drug delivery strategies for the treatment of onychomycosis. Pharm Nanotechnol. 2019;7(1):24–38.
Baran R, Hay RJ, Garduno JI. Review of antifungal therapy and the severity index for assessing onychomycosis: part I. J Dermatol Treat. 2008;19(2):72–81.
Shivakumar H, Juluri A, Desai B, Murthy SN. Ungual and transungual drug delivery. Drug Dev Ind Pharm. 2012;38(8):901–11.
Murdan S. Enhancing the nail permeability of topically applied drugs. Expert Opin Drug Deliv. 2008;5(11):1267–82.
Rajendra VB, Baro A, Kumari A, Dhamecha DL, Lahoti SR, Shelke SD. Transungual drug delivery: an overview. J Appl Pharm Sci. 2012;2(1):203–209.
Repka MA, Mididoddi PK, Stodghill SP. Influence of human nail etching for the assessment of topical onychomycosis therapies. Int J Pharm. 2004;282(1–2):95–106.
Tratta E. Iontophoresis as a non-invasive enhancement technique for the administration of drugs across biological membranes. Thesis. 2015. p. 1–114.
Chen K, Puri V, Michniak-Kohn B. Iontophoresis to overcome the challenge of nail permeation: considerations and optimizations for successful ungual drug delivery. AAPS J. 2021;23(1):1–15.
Kawa N, Lee KC, Anderson RR, Garibyan L. Onychomycosis: a review of new and emerging topical and device-based treatments. J Clin Aesthet Dermatol. 2019;12(10):29.
Badola A, Satish SB. A review: transungal drug delivery a new and novel system. Asian J Pharm Sci Technol. 2015;5(4):227–33.
Tiwary AK, Sapra B. High failure rate of transungal drug delivery: need for new strategies. Ther Deliv. 2017;8(5):239–42.
Belikov AV, Tavalinskaya AD, Smirnov SN, Sergeev AN. Application of Yb, Er: Glass laser radiation for active drug delivery at the treatment of onychomycosis. J Biomed Photon Eng. 2019;5(1): 010305.
Correia JH, Rodrigues JA, Pimenta S, Dong T, Yang Z. Photodynamic therapy review: principles, photosensitizers, applications, and future directions. Pharmaceutics. 2021;13(9):1332.
Bhatta AK, Keyal U, Wang XL. Photodynamic therapy for onychomycosis: a systematic review. Photodiagn Photodyn Ther. 2016;15:228–35.
Albarahmieh E, AbuAmmouneh L, Kaddoura Z, AbuHantash F, Alkhalidi BA, Al-Halhouli A. Fabrication of dissolvable microneedle patches using an innovative laser-cut mould design to shortlist potentially transungual delivery systems: in vitro evaluation. AAPS PharmSciTech. 2019;20(5):1–14.
Gupta AK, Paquet M. Improved efficacy in onychomycosis therapy. Clin Dermatol. 2013;31(5):555–63.
Gregoriou S, Kyriazopoulou M, Tsiogka A, Rigopoulos D. Novel and investigational treatments for onychomycosis. J Fungi. 2022;8(10):1079.
Nair AB, Chakraborty B, Murthy SN. Effect of polyethylene glycols on the trans-ungual delivery of terbinafine. Curr Drug Deliv. 2010;7(5):407–14.
Souza AM, Ribeiro RC, Pinheiro GK, Pinheiro FI, Oliveira WN, Souza LB, et al. Polishing the therapy of onychomycosis induced by Candida spp.: amphotericin B–loaded nail lacquer. Pharmaceutics. 2021;13(6):784.
Dehari D, Mehata AK, Priya V, Parbat D, Kumar D, Srivastava AK, et al. Luliconazole nail lacquer for the treatment of onychomycosis: formulation, characterization and in vitro and ex vivo evaluation. AAPS PharmSciTech. 2022;23(6):1–17.
Leung AK, Lam JM, Leong KF, Hon KL, Barankin B, Leung AA, et al. Onychomycosis: an updated review. Recent Pat Inflamm Allergy Drug Disc. 2020;14(1):32–45.
Tampucci S, Terreni E, Zucchetti E, Burgalassi S, Chetoni P, Monti D. Formulations based on natural ingredients for the treatment of nail diseases. Curr Pharm Des. 2020;26(5):556–65.
Vikas A, Rashmin P, Mrunali P, Chavan RB, Kaushik T. Mechanistic insights of formulation approaches for the treatment of nail infection: conventional and novel drug delivery approaches. AAPS PharmSciTech. 2020;21(2):1–12.
Mididoddi PK, Repka MA. Characterization of hot-melt extruded drug delivery systems for onychomycosis. Eur J Pharm Biopharm. 2007;66(1):95–105.
Caló E, Khutoryanskiy VV. Biomedical applications of hydrogels: a review of patents and commercial products. Eur Polymer J. 2015;65:252–67.
Monti D, Egiziano E, Burgalassi S, Tampucci S, Terreni E, Tivegna S, et al. Influence of a combination of chemical enhancers and iontophoresis on in vitro transungual permeation of nystatin. AAPS PharmSciTech. 2018;19(4):1574–81.
Fatima M, Monawwar S, Mohapatra S, Alex TS, Ahmed A, Taleuzzaman M, et al. In silico drug screening based development of novel formulations for onychomycosis management. Gels. 2021;7(4):221.
Chouhan P, Saini T. D-optimal design and development of microemulsion based transungual drug delivery formulation of ciclopirox olamine for treatment of onychomycosis. Indian J Pharm Sci. 2016;78(4):498–511.
Cordoba Díaz D, Losa Iglesias ME, Becerro de Bengoa Vallejo R, Cordoba Diaz M. Transungual delivery of ciclopirox is increased 3–4-fold by mechanical fenestration of human nail plate in an in vitro model. Pharmaceutics. 2019;11(1):29.
Gaballah EY, Borg TM, Mohamed EA. Hydroxypropyl chitosan nail lacquer of ciclopirox-PLGA nanocapsules for augmented in vitro nail plate absorption and onychomycosis treatment. Drug Delivery. 2022;29(1):3304–16.
Puri V, Savla R, Chen K, Robinson K, Virani A, Michniak-Kohn B. Antifungal nail lacquer for enhanced transungual delivery of econazole nitrate. Pharmaceutics. 2022;14(10):2204.
Costa-Orlandi CB, Mordorski B, Baltazar LM, Mendes-Giannini MJS, Friedman JM, Nosanchuk JD, et al. Nitric oxide releasing nanoparticles as a strategy to improve current onychomycosis treatments. J Drugs Dermatol: JDD. 2018;17(7):717–20.
Lee BC, Pangeni R, Na J, Koo K-T, Park JW. Preparation and in vivo evaluation of a highly skin-and nail-permeable efinaconazole topical formulation for enhanced treatment of onychomycosis. Drug Deliv. 2019;26(1):1167–77.
Agrawal V, Patel R, Patel M, Thanki K, Mishra S. Design and evaluation of microemulsion-based efinaconazole formulations for targeted treatment of onychomycosis through transungual route: ex vivo and nail clipping studies. Colloids Surf, B. 2021;201: 111652.
Devi A, Chaurasia H, Singh R. Development of nano formuation and its optimization evaluation of efinaconazole loaded transfersomal gel for treatment of nail infection. 2021;40(11):23–43.
Almuqbil RM, Sreeharsha N, Nair AB. Formulation-by-design of efinaconazole spanlastic nanovesicles for transungual delivery using statistical risk management and multivariate analytical techniques. Pharmaceutics. 2022;14(7):1419.
Al-Obaidi H, Petraityte I, Hibbard T, Majumder M, Kalgudi R, Zariwala MG. Antifungal nanosuspensions with surfactants and silver for the treatment of onychomycosis. Eur J Pharm Biopharm. 2022;179:194–205.
Barot BS, Parejiya PB, Patel HK, Mehta DM, Shelat PK. Microemulsion-based antifungal gel delivery to nail for the treatment of onychomycosis: formulation, optimization, and efficacy studies. Drug Deliv Transl Res. 2012;2:463–76.
Wagh VD, Deshmukh OJ. Itraconazole niosomes drug delivery system and its antimycotic activity against Candida albicans. Int Sch Res Not. 2012;1–7.
Hoda Q, Aqil M, Ahad A, Imam SS, Praveen A, Qadir A, et al. Optimization of valencene containing lipid vesicles for boosting the transungual delivery of itraconazole. 3 Biotech. 2021;11:1–13.
Alqahtani A, Raut B, Khan S, Mohamed JMM, Fatease AA, Alqahtani T, et al. The unique carboxymethyl fenugreek gum gel loaded itraconazole self-emulsifying nanovesicles for topical onychomycosis treatment. Polymers. 2022;14(2):325.
Mahtab A, Anwar M, Mallick N, Naz Z, Jain GK, Ahmad FJ. Transungual delivery of ketoconazole nanoemulgel for the effective management of onychomycosis. AAPS PharmSciTech. 2016;17:1477–90.
Thatai P, Kaur K, Sapra B. In-vitro evaluation of transungual formulation of ketoconazole for the management of onychomycosis. Drug Deliv Lett. 2018;8(2):140–52.
Wang F, Yang P, Choi J, Antovski P, Zhu Y, Xu X, et al. Cross-linked fluorescent supramolecular nanoparticles for intradermal controlled release of antifungal drug—a therapeutic approach for onychomycosis. ACS Nano. 2018;12(7):6851–9.
Amra K, Momin M. Formulation evaluation of ketoconazole microemulsion-loaded hydrogel with nigella oil as a penetration enhancer. J Cosmet Dermatol. 2019;18(6):1742–50.
Pereira RR, Testi M, Rossi F, Silva Junior JO, Ribeiro-Costa RM, Bettini R, et al. Ucuùba (Virola surinamensis) fat-based nanostructured lipid carriers for nail drug delivery of ketoconazole: development and optimization using box-behnken design. Pharmaceutics. 2019;11(6):284.
Dehari D, Mehata AK, Priya V, Parbat D, Kumar D, Srivastava AK, et al. Luliconazole nail lacquer for the treatment of onychomycosis: formulation, characterization and in vitro and ex vivo evaluation. AAPS PharmSciTech. 2022;23(6):175.
Al-Abbasi D. Development of novel miconazole-loaded nail sheets for the treatment of fungal infections using 3d printing & nanotechnology: University of Petra (Jordan). 2022;Thesis(1:4).
Šveikauskaitė I, Briedis V. Effect of film-forming polymers on release of naftifine hydrochloride from nail lacquers. Int J Polym Sci. 2017;1476270.
Šveikauskaitė I, Briedis V. Potential of naftifine application for transungual delivery. Molecules. 2020;25(13):3043.
Bozoğlan BK, Duman O, Tunç S. Smart antifungal thermosensitive chitosan/carboxymethylcellulose/scleroglucan/montmorillonite nanocomposite hydrogels for onychomycosis treatment. Colloids Surf, A. 2021;610: 125600.
Hosseinzoi A, Galli F, Incrocci L, Smijs T. Mechanical properties of healthy and ex vivo onychomycosis nails and the influence of a porphyrin-propylene glycol antifungal formulation. Bri J Appl Sci Technol. 2016;14(1):1–14.
Fernández-Campos F, Navarro F, Corrales A, Picas J, Pena E, González J, et al. Transungual delivery, anti-inflammatory activity, and in vivo assessment of a cyclodextrin polypseudorotaxanes nail lacquer. Pharmaceutics. 2020;12(8):730.
Bseiso EA, Nasr M, Sammour OA, Abd El Gawad NA. Novel nail penetration enhancer containing vesicles “nPEVs” for treatment of onychomycosis. Drug Deliv. 2016;23(8):2813–9.
Tuncay Tanrıverdi S, Hilmioğlu Polat S, Yeşim Metin D, Kandiloğlu G, Özer Ö. Terbinafine hydrochloride loaded liposome film formulation for treatment of onychomycosis: in vitro and in vivo evaluation. J Liposome Res. 2016;26(2):163–73.
Elsherif NI, Shamma RN, Abdelbary G. Terbinafine hydrochloride trans-ungual delivery via nanovesicular systems: in vitro characterization and ex vivo evaluation. AAPS PharmSciTech. 2017;18:551–62.
Valdes BSG, Serro AP, Gordo PM, Silva A, Gonçalves L, Salgado A, et al. New polyurethane nail lacquers for the delivery of terbinafine: formulation and antifungal activity evaluation. J Pharm Sci. 2017;106(6):1570–7.
El-sherif NI, Shamma RN, Abdelbary G. In-situ gels and nail lacquers as potential delivery systems for treatment of onychomycosis. A comparative study. J Drug Deliv Sci Technol. 2018;43:253–61.
Thatai P, Sapra B. Terbinafine hydrochloride nail lacquer for the management of onychomycosis: formulation, characterization and in vitro evaluation. Ther Deliv. 2018;9(2):99–119.
Yang F, Yu X, Shao W, Guo P, Cao S, Wang M, et al. Co-delivery of terbinafine hydrochloride and urea with an in situ film-forming system for nail targeting treatment. Int J Pharm. 2020;585: 119497.
Nair AB, Al-Dhubiab BE, Shah J, Gorain B, Jacob S, Attimarad M, et al. Constant Voltage iontophoresis technique to deliver terbinafine via transungual delivery system: formulation optimization using Box-Behnken design and in vitro evaluation. Pharmaceutics. 2021;13(10):1692.
Abobakr FE, Fayez SM, Elwazzan VS, Sakran W. Effect of different nail penetration enhancers in solid lipid nanoparticles containing terbinafine hydrochloride for treatment of onychomycosis. AAPS PharmSciTech. 2021;22:1–12.
Ullah KH, Raza F, Munawar SM, Sohail M, Zafar H, Zafar MI, et al. Poloxamer 407 based gel formulations for transungual delivery of hydrophobic drugs: selection and optimization of potential additives. Polymers. 2021;13(19):3376.
Fuhr R, Cook D, Ridden J, Nield K, Leigh E, Cook J, et al. Results from a phase 1/2 trial of BB2603, a terbinafine-based topical nano-formulation, in onychomycosis and tinea pedis. Mycoses. 2022;65(6):661–9.
Puri V, Froelich A, Shah P, Pringle S, Chen K, Michniak-Kohn B. Quality by design guided development of polymeric nanospheres of terbinafine hydrochloride for topical treatment of onychomycosis using a nano-gel formulation. Pharmaceutics. 2022;14(10):2170.
Pollard TD, Bonetti M, Day A, Gaisford S, Orlu M, Basit AW, et al. Printing drugs onto nails for effective treatment of onychomycosis. Pharmaceutics. 2022;14(2):448.
Ullah KH, Rasheed F, Naz I, Ul Haq N, Fatima H, Kanwal N, et al. Chitosan nanoparticles loaded poloxamer 407 Gel for transungual delivery of terbinafine HCl. Pharmaceutics. 2022;14(11):2353.
Costa AF, Luís S, Noro J, Silva S, Silva C, Ribeiro A. Therapeutic textiles functionalized with keratin-based particles encapsulating terbinafine for the treatment of onychomycosis. Int J Mol Sci. 2022;23(22):13999.
Flores FC, Rosso RS, Cruz L, Beck RC, Silva CB. An innovative polysaccharide nanobased nail formulation for improvement of onychomycosis treatment. Eur J Pharm Sci. 2017;100:56–63.
Rocha KAD, Krawczyk-Santos AP, Andrade LM, de Souza LC, Marreto RN, Gratieri T, et al. Voriconazole-loaded nanostructured lipid carriers (NLC) for drug delivery in deeper regions of the nail plate. Int J Pharm. 2017;531(1):292–8.
Krawczyk-Santos AP, da Rocha PB, Kloppel LL, Souza BdS, Anjos JLV, Alonso A, et al. Enhanced nail delivery of voriconazole-loaded nanomicelles by thioglycolic acid pretreatment: a study of protein dynamics and disulfide bond rupture. Int J Pharm. 2021;602:120597.
Kushwaha AS, Sharma P, Shivakumar H, Rappleye C, Zukiwski A, Proniuk S, et al. Trans-ungual delivery of AR-12, a novel antifungal drug. AAPS PharmSciTech. 2017;18:2702–5.
Tanrıverdi ST, Özer Ö. Novel topical formulations of terbinafine-HCl for treatment of onychomycosis. Eur J Pharm Sci. 2013;48(4–5):628–36.
Gratieri T, Krawczyk-Santos AP, da Rocha PB, Gelfuso GM, Marreto RN, Taveira SF. SLN-and NLC-encapsulating antifungal agents: skin drug delivery and their unexplored potential for treating onychomycosis. Curr Pharm Des. 2017;23(43):6684–95.
Abd-Elsalam WH, Nagy YI, Abouelatta SM. Tailoring thixotropic mixed-lipid nanoconstructs of voriconazole for the management of Vulvovaginal candidiasis: Formulation, statistical optimization, in vitro characterization and in vivo assessment. Drug Delivery. 2021;28(1):1877–89.
Kesharwani P, Fatima M, Singh V, Sheikh A, Almalki WH, Gajbhiye V, et al. Itraconazole and difluorinated-curcumin containing chitosan nanoparticle loaded hydrogel for amelioration of onychomycosis. Biomimetics. 2022;7(4):206.
Thakkar KN, Mhatre SS, Parikh RY. Biological synthesis of metallic nanoparticles. Nanomedicine: Nanotechnol Biol Med. 2010;6(2):257–62.
Chandrakala V, Aruna V, Angajala G. Review on metal nanoparticles as nanocarriers: current challenges and perspectives in drug delivery systems. Emergent Mater. 2022;5:1593–1615.
Morgado LF, Trávolo ARF, Muehlmann LA, Narcizo PS, Nunes RB, Pereira PAG, et al. Photodynamic therapy treatment of onychomycosis with aluminium-phthalocyanine chloride nanoemulsions: a proof of concept clinical trial. J Photochem Photobiol, B. 2017;173:266–70.
Marcato PD, Durán M, Huber SC, Rai M, Melo PS, Alves OL, et al. Biogenic silver nanoparticles and its antifungal activity as a new topical transungual drug. J Nano Res. 2012;20:99–107.
Lotfali E, Fattahi M, Ghasemi R, Zakermashhadi F, Shafiei M, Borzouie M, et al. Enhancement of the anti-biofilm activity of gold nanoparticles-itraconazole conjugates in resistant Candida glabrata. Recent Adv Anti-Infect Drug Disc Formerly Recent Patents Anti-Infect Drug Disc. 2021;16(2):137–47.
Tiwari N, Pandit R, Gaikwad S, Gade A, Rai M. Biosynthesis of zinc oxide nanoparticles by petals extract of Rosa indica L., its formulation as nail paint and evaluation of antifungal activity against fungi causing onychomycosis. IET Nanobiotechnol. 2017;11(2):205–11.
Dantas KN, Andrade LR, Lisboa E, Santana VL, Santos AL, Mello TP, et al. Antimycotic nail polish based on humic acid-coated silver nanoparticles for onychomycosis. J Chem Technol Biotechnol. 2021;96(8):2208–18.
Garg A, Sharma GS, Goyal AK, Ghosh G, Si SC, Rath G. Recent advances in topical carriers of anti-fungal agents. Heliyon. 2020;6(8): e04663.
Qadir A, Faiyazuddin M, Hussain MT, Alshammari TM, Shakeel F. Critical steps and energetics involved in a successful development of a stable nanoemulsion. J Mol Liq. 2016;214:7–18.
Pandey P, Minocha N, Vashist N, Shah R, Saini S, Makhija M, et al. Emulgel: an emerging approach towards effective topical drug delivery. Drug Deliv Lett. 2022;12(4):227–42.
Christenson JK, Peterson GM, Naunton M, Bushell M, Kosari S, Baby KE, et al. Challenges and opportunities in the management of onychomycosis. J Fungi. 2018;4(3):87.
Flores F, De Lima J, Ribeiro RF, Alves S, Rolim C, Beck RCR, et al. Antifungal activity of nanocapsule suspensions containing tea tree oil on the growth of Trichophyton rubrum. Mycopathologia. 2013;175:281–6.
Vörös-Horváth B, Das S, Salem A, Nagy S, Böszörményi A, Kőszegi T, et al. Formulation of tioconazole and melaleuca alternifolia essential oil Pickering emulsions for onychomycosis topical treatment. Molecules. 2020;25(23):5544.
Maddur Taluk MD. Formulation and evaluation of efinaconazole microemulsion with Eucalyptus citrodora oil. 2022;11(13):1742–1759.
Yasin G, Nasr M, Gaber SAA, Hüttenberger D, Fadel M. Response surface methodological approach for optimization of photodynamic therapy of onychomycosis using chlorin e6 loaded nail penetration enhancer vesicles. J Photochem Photobiol, B. 2022;232: 112461.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
Wessam H. Abd-Elsalam and Samar M. Aboelatta: investigation; conceptualization; methodology; resources; data curation; writing—original draft; writing—review and editing; visualization.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abd-Elsalam, W.H., Abouelatta, S.M. Contemporary Techniques and Potential Transungual Drug Delivery Nanosystems for The Treatment of Onychomycosis. AAPS PharmSciTech 24, 150 (2023). https://doi.org/10.1208/s12249-023-02603-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-023-02603-x