Abstract
Intracellular parasitic protozoa of Leishmania sp. causes leishmaniasis. The restricted access of the drugs to affected cells in the treatment of intracellular infections such as leishmaniasis is frequently hampered. Furthermore, most of today’s drugs have limited uses due to some containing toxic compounds, and drug resistance is on the rise. In the present investigation, Amphotericin B (AmB) and Terbinafine (Tbf) were loaded in microemulsion (ME) in combination and alone, and the in vivo efficacy was considered in BALB/c mice infected with Leishmania major (L. major). The wound size at the base of the mouse tail was measured, and real-time PCR was performed to quantify the parasite load after the infection challenge. The study demonstrated that the ME-AmB and ME-Tbf formulations are safe and effective compounds for the treatment of cutaneous leishmaniasis by enhancing the effectiveness of AmB and Tbf in reducing the parasite burden.










Similar content being viewed by others
References
Roberts C, McLeod R, Rice D, Ginger M, Chance M, Goad L. Fatty acid and sterol metabolism: potential antimicrobial targets in apicomplexan and trypanosomatid parasitic protozoa. Mol Biochem Parasitol. 2003;126(2):129–42. https://doi.org/10.1016/S0166-6851(02)00280-3.
Alvar J, Velez ID, Bern C, Herrero M, Desjeux P, Cano J, et al. Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE. 2012;7(5): e35671. https://doi.org/10.1371/journal.pone.0035671.
Asadi A, Kareshk AT, Sharifi I, Firouzeh N. Murine cathelicidin: as a host defensive response against Leishmania major infection. J Parasit Dis. 2020;44(3):633–8. https://doi.org/10.1007/s12639-020-01238-0.
Shalev M, Rozenberg H, Smolkin B, Nasereddin A, Kopelyanskiy D, Belakhov V, et al. Structural basis for selective targeting of leishmanial ribosomes: aminoglycoside derivatives as promising therapeutics. Nucleic Acids Res. 2015;43(17):8601–13. https://doi.org/10.1093/nar/gkv821.
Copeland NK, Aronson NE. Leishmaniasis: treatment updates and clinical practice guidelines review. Curr Opin Infect Dis. 2015;28(5):426–37. https://doi.org/10.1097/QCO.0000000000000194.
Sundar S, Mehta H, Suresh A, Singh SP, Madhukar R, Murray HW. Amphotericin B treatment for Indian visceral leishmaniasis: conventional versus lipid formulations. Clin Infect Dis. 2004;38(3):377–83. https://doi.org/10.1086/380971.
Soto J, Arana B, Toledo J, Rizzo N, Vega J, Diaz A, et al. Miltefosine for new world cutaneous leishmaniasis. Clin Infect Dis. 2004;38(9):1266–72. https://doi.org/10.1086/383321.
Rodrigues M, Costa R, Souza C, Foss N, Roselino A. Nephrotoxicity attributed to meglumine antimoniate (Glucantime) in the treatment of generalized cutaneous leishmaniasis. Rev Inst Med Trop Sao Paulo. 1999;41:33–7. https://doi.org/10.1590/S0036-46651999000100007.
Zulfiqar B, Shelper TB, Avery VM. Leishmaniasis drug discovery: recent progress and challenges in assay development. Drug Discov Today. 2017;22(10):1516–31. https://doi.org/10.1016/j.drudis.2017.06.004.
Croft SL, Sundar S, Fairlamb AH. Drug resistance in leishmaniasis. Clin Microbiol Rev. 2006;19(1):111–26. https://doi.org/10.1128/CMR.19.1.111-126.2006.
Mostafavi M, Farajzadeh S, Sharifi I, Khazaeli P, Sharifi H. Leishmanicidal effects of amphotericin B in combination with selenium loaded on niosome against Leishmania tropica. J Parasit Dis. 2019;43(2):176–85. https://doi.org/10.1007/s12639-018-1071-2.
Awasthi BP, Mitra K. In vitro leishmanicidal effects of the anti-fungal drug natamycin are mediated through disruption of calcium homeostasis and mitochondrial dysfunction. Apoptosis. 2018;23(7):420–35. https://doi.org/10.1007/s10495-018-1468-5.
Farajzadeh S, Heshmatkhah A, Vares B, Mohebbi E, Mohebbi A, Aflatoonian M, et al. Topical terbinafine in the treatment of cutaneous leishmaniasis: triple blind randomized clinical trial. J Parasit Dis. 2016;40(4):1159–64.
Ebrahimian S, Asilian A, Faghihi G. Comparetaive study on glucantime and oral terbinafine along with systemic glucantime on cutaneous leishmaniasis. Journal of Isfahan Medical School. 2011;28(118).
Zakai HA, Zimmo SK. Effects of itraconazole and terbinafine on Leishmania major lesions in BALB/c mice. Ann Trop Med Parasitol. 2000;94(8):787–91. https://doi.org/10.1080/00034983.2000.11813603.
Tripathi P, Jaiswal AK, Dube A, Mishra PR. Hexadecylphosphocholine (Miltefosine) stabilized chitosan modified Ampholipospheres as prototype co-delivery vehicle for enhanced killing of L. donovani. Int J Biol Macromol. 2017;105(1):625–37. https://doi.org/10.1016/j.ijbiomac.2017.07.076.
Singh N, Kumar M, Singh RK. Leishmaniasis: current status of available drugs and new potential drug targets. Asian Pac J Trop Med. 2012;5(6):485–97.
Sahoo S, Parveen S, Panda J. The present and future of nanotechnology in human health care. Nanomedicine. 2007;3(1):20–31. https://doi.org/10.1016/j.nano.2006.11.008.
Sahu T, Ratre YK, Chauhan S, Bhaskar L, Nair MP, Verma HK. Nanotechnology based drug delivery system: current strategies and emerging therapeutic potential for medical science. J Drug Deliv Sci Technol. 2021;63: 102487. https://doi.org/10.1016/j.jddst.2021.102487.
Herrero-Vanrell R, De La Torre MV, Andrés-Guerrero V, Barbosa-Alfaro D, Molina-Martínez IT, Bravo-Osuna I. Nano and microtechnologies for ophthalmic administration, an overview. J Drug Deliv Sci Technol. 2013;23(2):75–102. https://doi.org/10.1016/S1773-2247(13)50016-5.
Mei L, Zhang Z, Zhao L, Huang L, Yang X-L, Tang J, et al. Pharmaceutical nanotechnology for oral delivery of anticancer drugs. Adv Drug Deliv Rev. 2013;65(6):880–90. https://doi.org/10.1016/j.addr.2012.11.005.
Lin Y-H, Tsai M-J, Fang Y-P, Fu Y-S, Huang Y-B, Wu P-C. Microemulsion formulation design and evaluation for hydrophobic compound:catechin topical application. Colloids Surf, B. 2018;161:121–8.
Oliveira MB, Calixto G, Graminha M, Cerecetto H, González M, Chorilli M. Development, characterization, and in vitro biological performance of fluconazole-loaded microemulsions for the topical treatment of cutaneous leishmaniasis. Biomed Res Int. 2015;2015:1–12. https://doi.org/10.1155/2015/396894.
Chawla B, Madhubala R. Drug targets in Leishmania. J Parasit Dis. 2010;34(1):1–13.
Sundar S, Singh A, Singh OP. Strategies to overcome anti-leishmanial drugs unresponsiveness. J Trop Med. 2014;2014:1–7. https://doi.org/10.1155/2014/646932.
Bseiso E, Nasr M, Sammour O, Abd El Gawad N. Recent advances in topical formulation carriers of antifungal agents. Indian J Dermatol Venereol Leprol. 2015;81(5):457–63. doi: https://doi.org/10.4103/0378-6323.162328.
Yazdanpanah Y, Sissoko D, Egger M, Mouton Y, Zwahlen M, Chêne G. Clinical efficacy of antiretroviral combination therapy based on protease inhibitors or non-nucleoside analogue reverse transcriptase inhibitors: indirect comparison of controlled trials. bmj. 2004;328(7434):1–7. https://doi.org/10.1136/bmj.37995.435787.A6.
Farajzadeh S, Esfandiarpour I, Haghdoost AA, Mohammadi S, Mohebbi A, Mohebbi E, et al. Comparison between combination therapy of oral terbinafine and cryotherapy versus systemic meglumine antimoniate and cryotherapy in cutaneous leishmaniasis: a randomized clinical trial. Iran J Parasitol. 2015;10(1):1–8.
Seifert K, Croft SL. In vitro and in vivo interactions between miltefosine and other anti-leishmanial drugs. Antimicrob Agents Chemothe. 2006;50(1):73–9. https://doi.org/10.1128/AAC.50.1.73-79.2006.
Omollo R, Alexander N, Edwards T, Khalil EA, Younis BM, Abuzaid AA, et al. Safety and efficacy of miltefosine alone and in combination with sodium stibogluconate and liposomal amphotericin B for the treatment of primary visceral leishmaniasis in East Africa: study protocol for a randomized controlled trial. Trials. 2011;12(1):1–10. https://doi.org/10.1186/1745-6215-12-166.
Garnier T, Croft SL. Topical treatment for cutaneous leishmaniasis. Curr Opin Investig Drugs. 2002;3(4):538–44.
Owais M, Gupta C. Targeted drug delivery to macrophages in parasitic infections. Curr Drug Deliv. 2005;2(4):311–8.
Minodier P, Parola P. Cutaneous leishmaniasis treatment. Travel Med Infect Dis. 2007;5(3):150–8. https://doi.org/10.1016/j.tmaid.2006.09.004.
Kale SN, Deore SL. Emulsion micro emulsion and nano emulsion: a review. Syst Rev Pharm. 2017;8(1):39–47. https://doi.org/10.5530/srp.2017.1.8.
Damasceno BP, Dominici VA, Urbano IA, Silva JA, Araújo IB, Santos-Magalhães NS, et al. Amphotericin B microemulsion reduces toxicity and maintains the efficacy as an antifungal product. J Biomed Nanotechnol. 2012;8(2):290–300.
Darole PS, Hegde DD, Nair HA. Formulation and evaluation of microemulsion based delivery system for amphotericin B. AAPS PharmSciTech. 2008;9(1):122–8. https://doi.org/10.1208/s12249-007-9022-8.
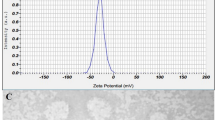
Butani D, Yewale C, Misra A. Amphotericin B topical microemulsion: formulation, characterization and evaluation. Colloids Surf, B. 2014;116:351–8.
Barot BS, Parejiya PB, Patel HK, Gohel MC, Shelat PK. Microemulsion-based gel of terbinafine for the treatment of onychomycosis: optimization of formulation using D-optimal design. AAPS PharmSciTech. 2012;13(1):184–92. https://doi.org/10.1208/s12249-011-9742-7.
Celebi N, Ermiş S, Özkan S. Development of topical hydrogels of terbinafine hydrochloride and evaluation of their antifungal activity. Drug Dev Ind Pharm. 2015;41(4):631–9. https://doi.org/10.3109/03639045.2014.891129.
do Vale Morais AR, Silva AL, Cojean S, Balaraman K, Bories C, Pomel S, et al. In-vitro and in-vivo antileishmanial activity of inexpensive Amphotericin B formulations: heated Amphotericin B and Amphotericin B-loaded microemulsion. Experimental parasitology. 2018;192:85–92.
Date AA, Nagarsenker M. Parenteral microemulsions: an overview. Int J Pharm X. 2008;355(1–2):19–30. https://doi.org/10.1016/j.ijpharm.2008.01.004.
Louis Lima da Silveira W, PGL Damasceno B, F Ferreira L, LS Ribeiro I, S Silva K, Leandro Silva A, et al. Development and characterization of a microemulsion system containing amphotericin B with potential ocular applications. Current drug delivery. 2016;13(6):982–93.
R Dabhi M, A Nagori S, R Sheth N, K Patel N, V Dudhrejiya A. Formulation optimization of topical gel formulation containing micro-emulsion of terbinafine hydrochloride with simplex lattice design. Micro and Nanosystems. 2011;3(1):1–7.
Mohsin SMN, Hussein MZ, Sarijo SH, Fakurazi S, Arulselvan P, Hin T-YY. Synthesis of (cinnamate-zinc layered hydroxide) intercalation compound for sunscreen application. Chem Cent J. 2013;7(1):1–12. https://doi.org/10.1186/1752-153X-7-26.
Jaafari MR, Hatamipour M, Alavizadeh SH, Abbasi A, Saberi Z, Rafati S, et al. Development of a topical liposomal formulation of Amphotericin B for the treatment of cutaneous leishmaniasis. Int J Parasitol Drugs Drug Resist. 2019;11:156–65. https://doi.org/10.1016/j.ijpddr.2019.09.004.
Laniado-Laborín R, Cabrales-Vargas MN. Amphotericin B: side effects and toxicity. Rev Iberoam Micol. 2009;26(4):223–7.
Ajit C, Zaeri N, Munoz SJ, Suvannasankha A. Terbinafine-associated hepatotoxicity. Am J Med Sci. 2003;325(5):292–5. https://doi.org/10.1097/00000441-200305000-00008.
Tonomura Y, Yamamoto E, Kondo C, Itoh A, Tsuchiya N, Uehara T, et al. Amphotericin B-induced nephrotoxicity: characterization of blood and urinary biochemistry and renal morphology in mice. Hum Exp Toxicol. 2009;28(5):293–300.
van’t Wout JW. Herrmann WA, de Vries RA, Stricker BHC. Terbinafine-associated hepatic injury J Hepatol. 1994;21(1):115–7.
Acknowledgements
This paper has been extracted from a Ph.D. thesis (Baharvandi Z.). We appreciate the Infectious and Tropical Diseases Research Center, Health Research Institute, Deputy of Development and Research, Ahvaz Jundishapur University of Medical Sciences. The study Protocol No. IR.AJUMS.ABHC.REC.1398.048 was approved by the Ethics Committee on Research in the School of Medicine, Ahvaz Jundishapur University of Medical Sciences.
Funding
This study was supported by the Infectious and Tropical Diseases Research Center, Health Research Institute, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran (No. OG-9815).
Author information
Authors and Affiliations
Contributions
Conception and design of the study: Z. Baharvandi, A. Salimi, A. Jelowdar, and R. Arjmand. Acquisition of data and investigation: Z. Baharvandi, A. Salimi, and A. Jelowdar. Analysis and interpretation of data: Z. Baharvandi, A. Salimi, A. Jelowdar and, A. Rafiei. Drafting the manuscript: Z. Baharvandi, A. Salimi, and A. Jelowdar. Revising the manuscript critically for important intellectual content: Z. Baharvandi, A. Salimi, A. Jelowdar, R. Arjmand, and A. Rafiei. Approval of the version of the manuscript to be published: Z. Baharvandi, A. Salimi, A. Jelowdar, R. Arjmand, and A. Rafiei.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baharvandi, Z., Salimi, A., Arjmand, R. et al. Evaluation of the Efficacy of Amphotericin B and Terbinafine Microemulsions and Their Combination on Cutaneous Leishmaniasis and Comparison with the Conventional Drug Form in BALB/c Mice. AAPS PharmSciTech 23, 280 (2022). https://doi.org/10.1208/s12249-022-02435-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-022-02435-1